The History of Mayo Clinic's Department of Anesthesiology and Perioperative Medicine
Welcome
Mayo Clinic’s Department of Anesthesiology and Perioperative Medicine was officially formed on April 1, 1924. In its first century, the department has played pivotal roles in a variety of important developments that have advanced the specialty of anesthesiology. These include:
- Dedicated nurses at Mayo Clinic who delivered anesthesia in the 1890s, starting the field of nurse anesthesia.
- Early trials that led to the use of sodium pentothal.
- Innovations such as the nation’s first blood bank and postoperative intensive care unit.
- Creation of the intravenous catheter.
- Training of “90-day wonders,” physicians trained in anesthesiology during World War II, many of whom became major leaders of the specialty.
- Co-founding and leadership of specialty organizations such as the American Society of Anesthesiologists and the American Board of Anesthesiology.
The 2024-2025 Centennial Celebration
April 1, 2024, marked the “official” Centennial anniversary of Mayo Clinic’s Department of Anesthesiology and Perioperative Medicine. April 1, 1924, is considered the start of the department based on the official designation on April 1, 1924, by the Mayo Clinic Board of Governors of the Section on Regional Anesthesia. The section was to evolve into the current Department of Anesthesiology and Perioperative Medicine. This Centennial Celebration also recognized the 31 years of nurse anesthesia preceding the official recognition of the future department, the contributions of Mayo Clinic nurse anesthetists to the establishment of the field of nurse anesthesia, and the development of the specialty of anesthesiology, respiratory therapy and intensive care units at Mayo Clinic. This webpage is a testament to not only the first 100 years of the department, but for the future as well. You can learn more about the Centennial Project by going to the “2024-2025 Centennial Celebration” section beneath the “Department History” tab.
Centennial Celebration Weekly Updates
From September 7, 2023, through November 7, 2024, Dr. Mark Warner and the rest of the Centennial Project Team produced and distributed weekly updates that contained very brief descriptions of articles or vignettes that highlighted the department’s development, remarkable personnel across the spectrum of the department (e.g., respiratory therapists, nurse anesthetists, anesthesiologists, scientists, and administrators), and contributions to the specialty’s advances and recognition. These updates can all be viewed on the “2024-2025 Centennial Celebration” page.

Highlighted Sections of this Site
Here you can read the 59 "Centennial Celebration Weekly Updates" that Dr. Mark Warner wrote during the 2024-2025 Centennial Celebration of the Department. These updates contain very brief descriptions of articles or vignettes that highlighted the department’s development, remarkable personnel across the spectrum of the department (e.g., respiratory therapists, nurse anesthetists, anesthesiologists, scientists, and administrators), and contributions to the specialty’s advances and recognition.
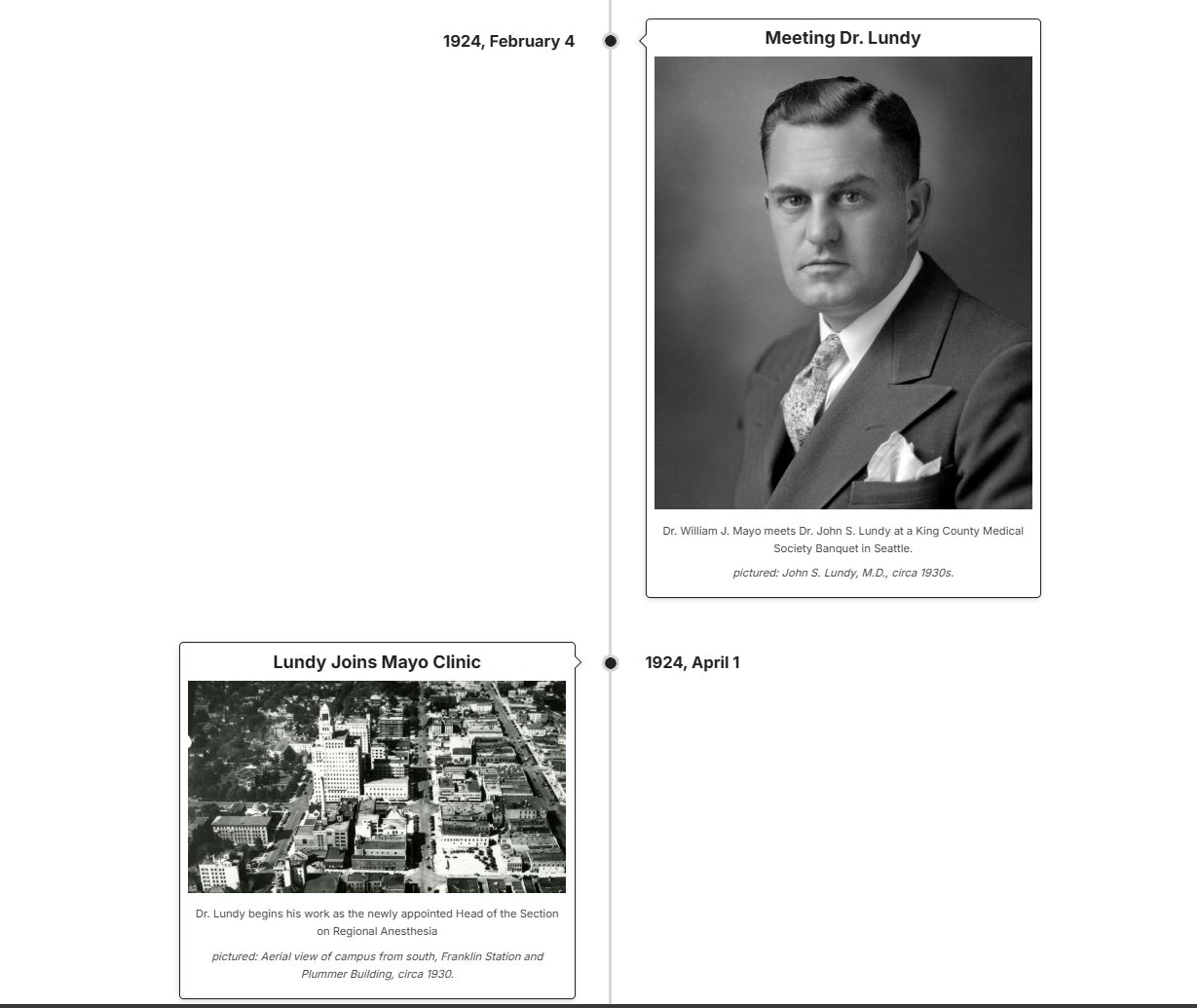
Check out this created timeline that shows major events in the department’s history and highlights how the Department of Anesthesiology has impacted the field of anesthesia. Did you know that Dr. William J. Mayo met Dr. John S. Lundy at a King County Medical Society Banquet in Seattle on February 4, 1924, which led to Dr. Lundy coming to work at Mayo Clinic on April 1st of that same year?

Learn more about the archival collections that the Mayo Clinic Archives holds related to the Department of Anesthesiology. Some collections to note are: the Department of Anesthesiology Records, the Nurse Anesthesia Education Program Records, and the CRNA Division Alumni Records.

Read bios about department staff members that were highlighted in Dr. Mark Warner’s Centennial Celebration weekly updates in 2024. Did you know that Dr. Virginia Hartridge served as the director of Mayo Clinic’s nurse anesthesia training program from 1956 through 1976?

See how individuals from the Department of Anesthesiology have served our country in the armed forces. Did you know that Dr. Edward Paul Didier flew 37 missions with the 479th Bomb Group in the B-29 “Thumper”?

Learn more about the history of the department through interviews with those who have been a part of it. There are five interviews from the Section on the History of Anesthesiology Living History Series where five retired staff members are interviewed about their time at Mayo Clinic.
Read past alumni newsletters from the Department of Anesthesiology. From 2002 until 2008 the department produced a department newsletter that contained vignettes and stories from the department
This webpage was designed in partnership between the Department of Anesthesiology and Perioperative Medicine, the W. Bruce Fye Center for the History of Medicine, Mayo Clinic Archives in Rochester, and Mayo Clinic History & Heritage.
The information, photographs, videos, and attachments that are found on this webpage have been curated together in partnership between the Department of Anesthesiology and Perioperative Medicine, the W. Bruce Fye Center for the W. History of Medicine, Mayo Clinic Archives in Rochester, and Mayo Clinic Media Asset Management (MAM).
Photographs used with permission of Mayo Foundation for Medical Education and Research. All rights reserved.
