April 1, 2024, marked the “official” Centennial anniversary of Mayo Clinic’s Department of Anesthesiology and Perioperative Medicine. April 1, 1924, is considered the start of the department based on the official designation on April 1, 1924, by the Mayo Clinic Board of Governors of the Section on Regional Anesthesia. The section was to evolve into the current Department of Anesthesiology and Perioperative Medicine. This Centennial Celebration also recognized the 31 years of nurse anesthesia preceding the official recognition of the future department, the contributions of Mayo Clinic nurse anesthetists to the establishment of the field of nurse anesthesia, and the development of the specialty of anesthesiology, respiratory therapy and intensive care units at Mayo Clinic.
With the recruitment of John Lundy, M.D. from Seattle by Dr. William Mayo and Dr. Lundy’s start at Mayo Clinic on April 1, 1924, the new Section on Regional Anesthesia began what was to evolve progressively to the Section on Anesthesia, the Department of Anesthesiology, and now the Department of Anesthesiology and Perioperative Medicine. Dr. Lundy quickly added innovative advances to the nascent specialty of anesthesiology, both internally at Mayo Clinic and nationally. Dr. Lundy established the first anatomy lab at the Mayo Clinic. He believed that the lab would serve as a useful tool for teaching residents as well as research into regional anesthetic techniques. To advance the science of anesthesiology, Dr. Lundy developed the concept of balanced anesthesia, pioneered the introduction of barbiturates (e.g., pentothal) to the practice of anesthesia, and developed anesthesia section services for the use of ventilators, ventilator vests, oxygen tents, and nasal oxygen supplementation. Remarkably, in 1935 he also established the nation’s first blood bank.
The Centennial Celebration lasted from April 1, 2024, to April 27, 2025. A Centennial Project team was established. This team consisted of physicians, nurses, administrators, and historical staff.
- Douglas R. Bacon, M.D.
- Sherri L. Durst, M.B.A. (Administrator)
- Marlea A. Judd, CRNA, D.N.P.
- Mary Marienau, CRNA, Ph.D.
- Erin E. Martin, CRNA, D.N.P.
- Alec J. Thicke, M.L.I.S. (Archivist)
- Mark A. Warner, M.D.
- Renee E. Ziemer (Mayo History Unit)
Some of the accomplishments from this project include:
- A Centennial Gala on April 13, 2024.
- This historical webpage was created and grew exponentially.
- From September 7, 2023, through November 7, 2024, Dr. Mark Warner and the rest of the Centennial Project Team produced and distributed 59 weekly updates that contained very brief descriptions of articles or vignettes that highlighted the department’s development, remarkable personnel across the spectrum of the department (e.g., respiratory therapists, nurse anesthetists, anesthesiologists, scientists, and administrators), and contributions to the specialty’s advances and recognition.
- A series of visiting professors came to Rochester to speak at the Mayo Clinic about the history of the department and its impact on the specialty.
- Alec Thicke, our department archivist, curated a small exhibit titled “Celebrating 100 Years of Anesthesiology at Mayo Clinic” that was put on display on the 12th floor of the Plummer Building. This exhibit was on display from March 2024-October 2024. The exhibit focused on the history of the Department of Anesthesiology.
- Alec Thicke, our department archivist, also curated a larger exhibit titled “100 Years of Innovation: Mayo Clinic and the History of the Specialty of Anesthesiology” was put on display at the International Museum of Surgical Science. This exhibit will be on display from August 2024-August 2025. This exhibit was a collaboration between Mayo Clinic and the International Museum of Surgical Science and features artifacts from both institutions.
- To close out the Centennial, from April 25, 2025 to April 27, 2025, the annual meeting of the Anesthesia History Association (AHA) was held in Rochester, Minnesota at the Marriott and Kahler Hotels. It was co-hosted by Mayo Clinic’s Department of Anesthesiology and Perioperative Medicine and the History of Anesthesia Society.
Mayo Clinic History of Medicine Visiting Speakers
The visiting professors that came to Rochester to speak about the history of the department and its impact on the specialty included:
- November 18, 2024: Christine Ball, M.D., is an anaesthesiologist at Alfred Hospital in Melbourne, Victoria, Australia. She was the 2020-2024 Wood Library-Museum of Anesthesiology’s Laureate of the History of Anesthesiology. She also is the long-serving Honorary Curator of the Geoffrey Kaye Museum of Anaesthesia History.
- December 9, 2024: Peter J. Featherstone, M.B.B.Ch., is an anaesthesiologist and intensivist at Cambridge University Hospitals in England. He has won numerous awards in anesthesia history. He currently is the president of the History of Anaesthesia Society (Great Britain).
- April 28, 2025: David J. Wilkinson, M.B.B.S., is a retired consultant anaesthesiologist from St. Bartholomew’s Hospital in London. He was the 2008-2012 Wood Library-Museum of Anesthesiology’s Laureate of the History of Anesthesiology. He also served as president of the World Federation of Societies of Anaesthesiologists from 2008 through 2012. He will present on April 28, 2025.
Centennial Celebration Weekly Updates
To better search these weekly updates, please use this provided index.
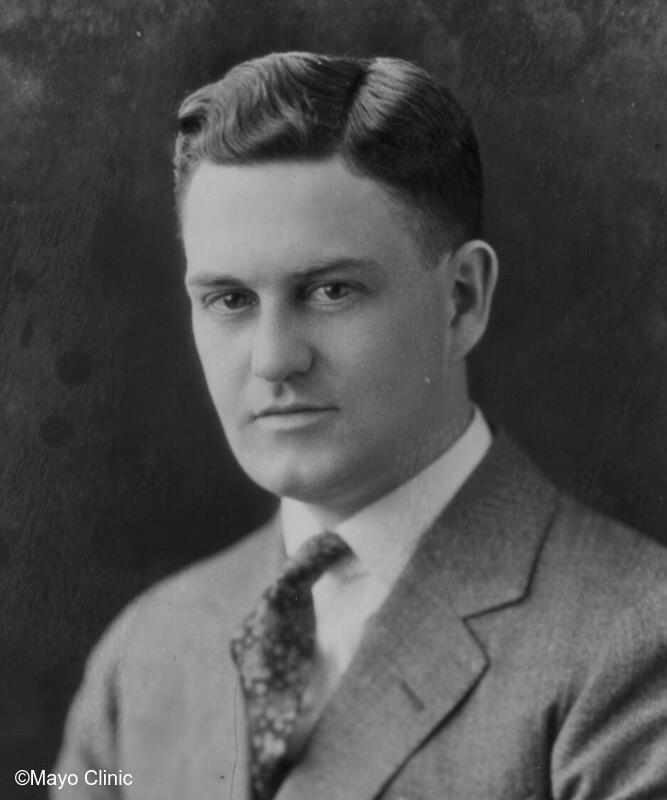

Photograph 1: Mayo Clinic employee photograph of Dr. John Silas Lundy, undated.
Photograph 2: Alice Magaw Kessel, undated.
Initial Announcement
This is the first of 80 weekly email updates that you will receive as we celebrate the Mayo Clinic Department of Anesthesiology and Perioperative Medicine’s 100th anniversary over the next 18 months.
I am proud to announce that the Department of Anesthesiology and Perioperative Medicine will be celebrating the centennial anniversary of the department in April 2024. This date is based on the official designation on April 1, 1924, by the Mayo Clinic Board of Governors of the Section on Regional Anesthesia. The section was to evolve into our current Department of Anesthesiology and Perioperative Medicine. This Centennial Celebration will also recognize the 31 years of nurse anesthesia preceding the official recognition of the future department, the contributions of Mayo Clinic nurse anesthetists to the establishment of the field of nurse anesthesia, and the development of the specialty of anesthesiology, respiratory therapy and intensive care units at Mayo Clinic.
With the recruitment of John Lundy, M.D. from Seattle by Dr. William Mayo and Dr. Lundy’s start at Mayo Clinic on April 1, 1924, the new Section on Regional Anesthesia began what was to evolve progressively to the Section on Anesthesia, the Department of Anesthesiology, and now the Department of Anesthesiology and Perioperative Medicine. Dr. Lundy quickly added innovative advances to the nascent specialty of anesthesiology, both internally at Mayo Clinic and nationally. As described by our colleagues Drs. Terry A. Ellis, Bradly J. Narr, and Douglas R. Bacon in a 2004 article in the Journal of Clinical Anesthesia, Dr. Lundy established the first anatomy lab at the Mayo Clinic. He believed that the lab would serve as a useful tool for teaching residents as well as research into regional anesthetic techniques. To advance the science of anesthesiology, Dr. Lundy developed the concept of balanced anesthesia, pioneered the introduction of barbiturates (e.g., pentothal) to the practice of anesthesia, and developed anesthesia section services for the use of ventilators, ventilator vests, oxygen tents, and nasal oxygen supplementation. Remarkably, in 1935 he also established the nation's first blood bank.
For the next year-and-a-half, the Centennial Project Team will be sending you short weekly emails, with each containing very brief descriptions of articles or vignettes that highlight the department’s development, remarkable personnel across the spectrum of the department (e.g., respiratory therapists, nurse anesthetists, anesthesiologists, scientists, and administrators), and contributions to the specialty’s advances and recognition. These emails will contain links to either the articles directly or to these stories on our new History of the Department of Anesthesiology website. The website will be available to everyone, both those within Mayo Clinic’s firewall and those outside of the institution. I promise that you will find many of the articles and stories to be quick reads, interesting, and often entertaining.
For this Introductory update, I’ve linked two published articles that showcase our founders, Dr. Lundy and Alice Magaw. I also have attached a pdf file of an article by Scott Atchison, written in our 2002 department newsletter, describing our good friend and long-time colleague, Dr. Rungson Sittipong. I believe you will enjoy reading them.
- “Alice Magaw (Kessel): Her Life In and Out of the Operating Room" by Jeffrey E. Nelson, CRNA, MNA; Steve F. Wilstead, CRNA, MNA. AANA Journal 2009.
- "Developing a Specialty: J.S. Lundy Three Major Contributions to Anesthesiology” by Terry A. Ellis II MD; Bradly J. Narr MD; Douglas R. Bacon MD, MA. Journal of Clinical Anesthesia Volume 16, Issue 3, May 2004, Pages 226-229.
- “Our Friend Rungson” Mayo Anesthesiology Alumni Newsletter. September 2002, Vol. 1, No. 1
Mystery Photos
We’ll also have an Anesthesia History Mystery Photo each week. Everyone who sends me a correct identification of the person in the photo via email response (warner.mark@mayo.edu) within three days of us sending out the emailed update will be entered into a drawing for a $10 gift card to Starbucks. You will need to send me your name and contact information so that I can send out the card to the winner each week. Each person will be allowed a single win during the series of 80 updates during the Centennial Celebration’s 18 months.
This month’s mystery person, a remarkable leader:

I’ll provide more information in the coming months as we near the start of the 100th anniversary and throughout the year of celebration. On behalf of the Centennial Project Team (listed below), we hope that you enjoy reading about the amazing colleagues who developed one of the world’s outstanding departments of anesthesiology.


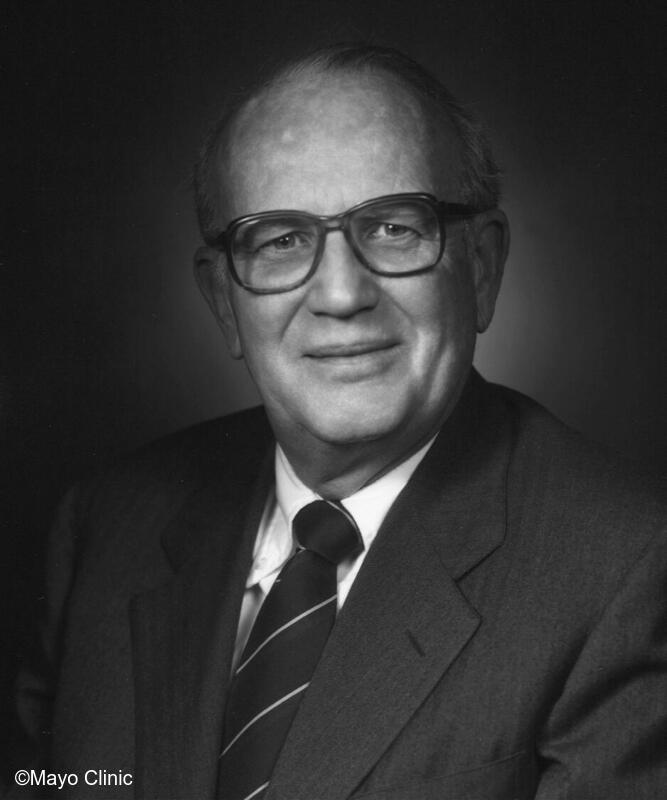
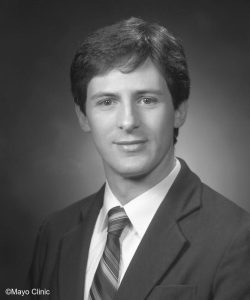
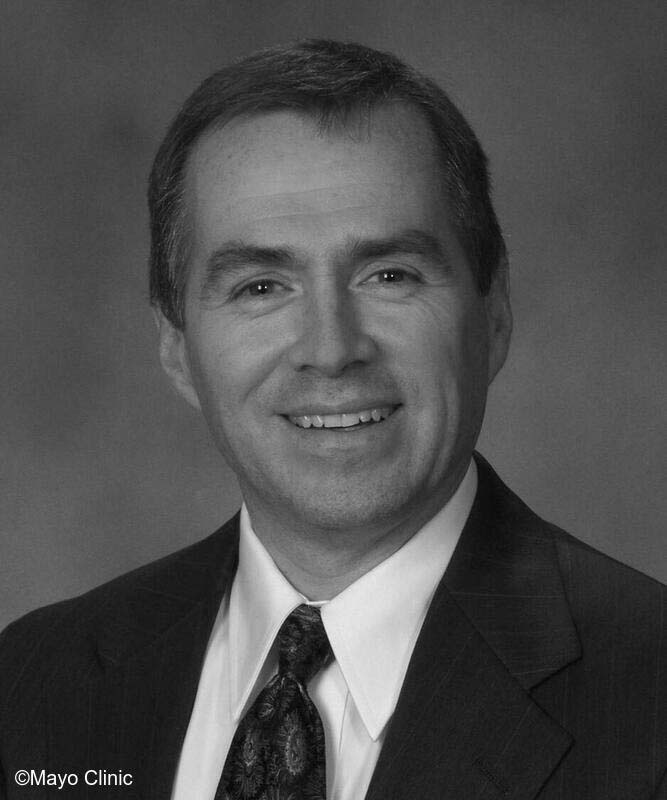
Photograph 1: Mayo Clinic employee photograph of Dr. Douglas Bacon, 2023.
Photograph 2: Mayo Clinic employee photograph of Jane Post, undated.
Department History
Welcome back. I promised you updates that will be much shorter than last week’s (September 7th) introduction to the Centennial Celebration.
- “How Old is the Mayo Department of Anesthesiology?”: There is some debate as to the original start of the Department of Anesthesiology, at least as we know it in its present form. Doug Bacon describes this debate in one of our 2004 department newsletters.
- “A Conversation with Mrs. Jane Post”: Jane Post, one of our department’s lead office staff members, worked for our Legal Department’s Harry Blackman starting in 1955, four years before Mr. Blackman became a federal court of appeals judge and in 1970 became an associate Supreme Court justice). Jane interacted with John Lundy regularly and partnered with every department chair from Albert Faulconer in 1955 through Duane Rorie when she retired in 1994. Peter Southorn’s summary of her observations gives us great insights into the characters and characteristics of these department chairs.
Mystery Photos
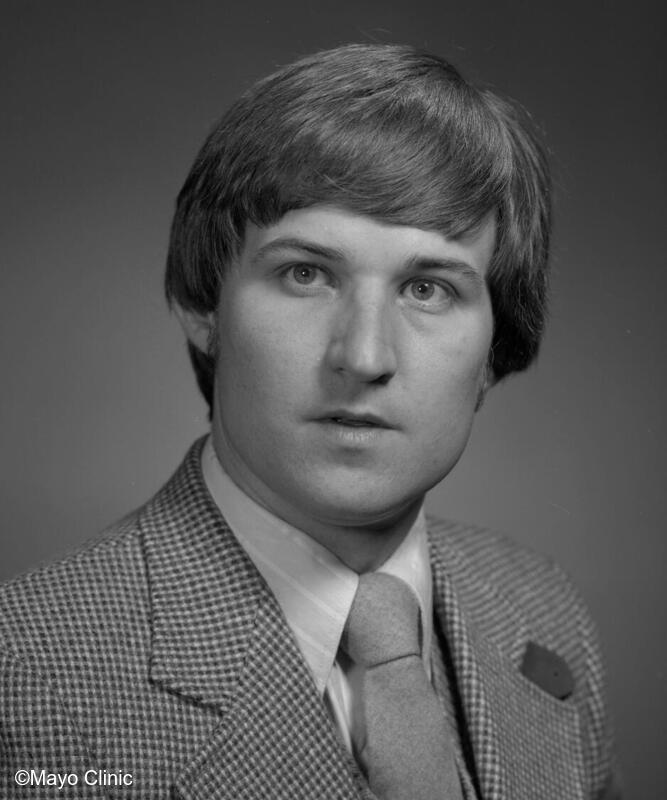
Last week’s History Mystery Photo was Alan Sessler. Alan was department chair from 1977-89.

Here is this week’s Mystery Photo:

Please email your response at warner.mark@mayo.edu within 3 days of this update. I will also need your name and contact information. All correct responses will be placed into a drawing for a $10 Starbucks card. Only one winner per individual over the 80 weeks of Mystery Photos.

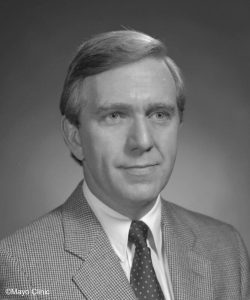
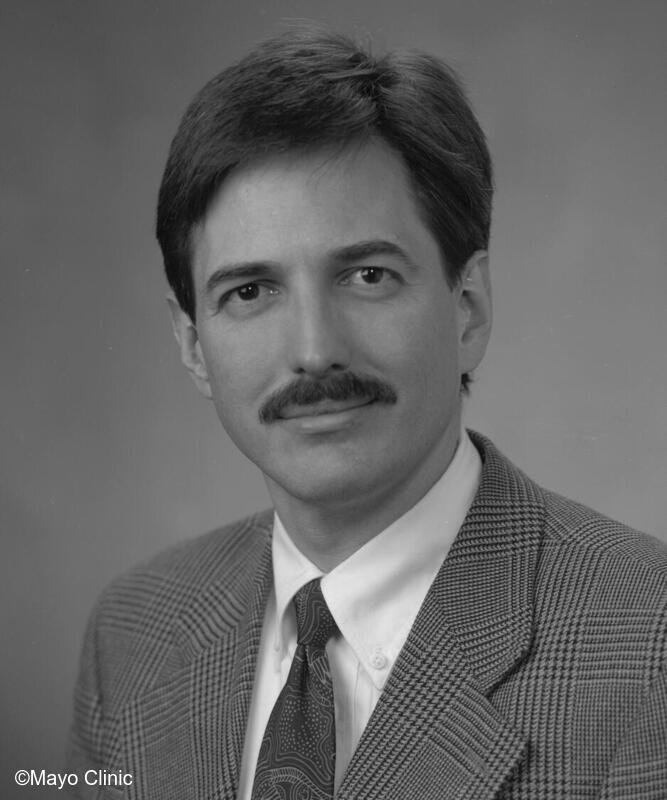
Mayo Clinic employee photograph of Dr. Steven Rettke, undated.
Call for Military Information
Will and Charlie Mayo were strong supporters of the U.S. military. Their advocacy led to the creation of the U.S. Army Medical Reserve Corps and their intensive work during WWI led to a remarkable advance in the quality of care provided to our soldiers, sailors, and pilots both during the war and far into the future. Many Mayo physicians and nurses played important roles in the military in WWI and in conflicts since that time.
The Department of Anesthesiology’s personnel also contributed to our armed forces military readiness and responses. In the coming months you will be amazed by the stories of our department colleagues and their military contributions in every branch of service. Here are two short military-related stories that provide details on some of our colleagues and a program at Mayo Clinic that helped launch the specialty of anesthesiology as we know it now.
- “Military Profiles”: This 2003 summary describes the military experiences of four of our colleagues, with their actions involving WWII through Desert Storm.
- “The Mayo Clinic World War II Short Course and Its Effect on Anesthesiology”: The linked article from Anesthesiology, V 105, No 1, Jul 2006, showcases our department’s leadership in the creation and implementation of the WWII “Short Course” that rapidly produced anesthesia-trained physicians for WWII.
Steve Rettke, a distinguished U.S. Navy carrier fighter pilot and retired Navy captain, as well as long-time leader of our Methodist Hospital clinical practices, will be creating webpages on our new history website. This website is being created and will become fully operational on November 1st. In the meantime, you can read its interim homepage at Anesthesiology Department | Mayo Clinic | History and Heritage.
If you have served at any point in the U.S. Armed Forces, Steve is asking for you to send the following information to both him (Rettke.steven@mayo.edu) and Alec Thicke (Thicke.alec@mayo.edu). Alec is our department’s new archivist and major contributor to our Centennial Project. They will create a database and add this information and your stories to the webpages.
- Name:
- Service:
- Rank:
- MOS / Specialty:
- Deployments/ Assignments:
- Anesthesiology Department Association:
- Photos of your time in the military, if any:
Mystery Photos
Last week’s History Mystery Photo was Mary Marienau. Mary was director of our Rochester Nurse Anesthesia training program and took it through advances that led to Master’s and then DNP degrees for graduates.

Here is this week’s Mystery Photo:

Please email your response at warner.mark@mayo.edu within 3 days of this update. I will also need your name and contact information. All correct responses will be placed into a drawing for a $10 Starbucks card. Only one winner per individual over the 80 weeks of Mystery Photos.

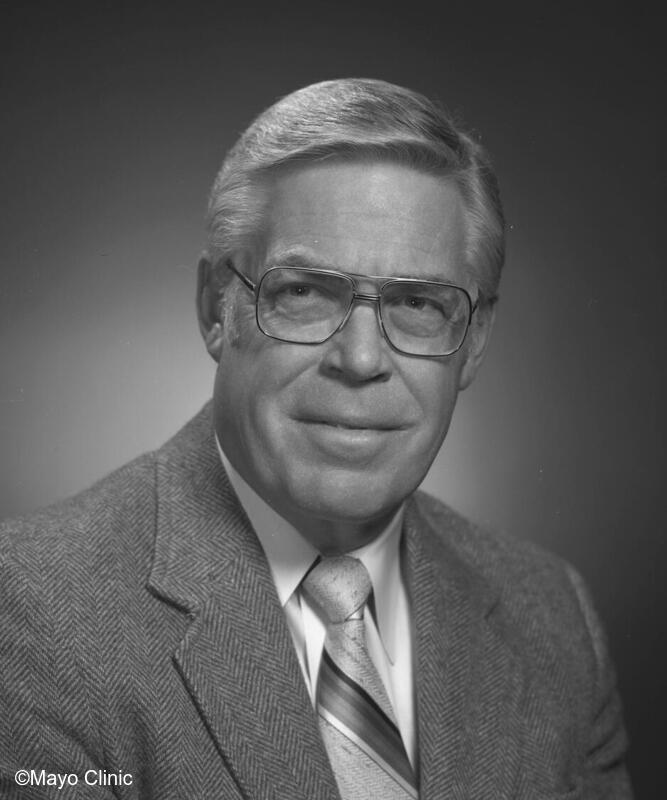
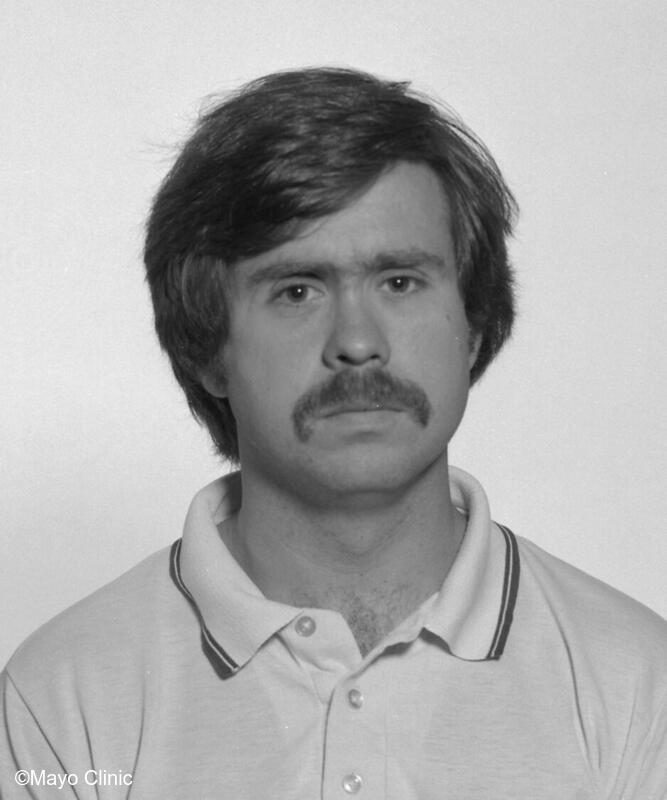
Photograph 1: Mayo Clinic employee photograph of Dr. Allan Sessler, undated.
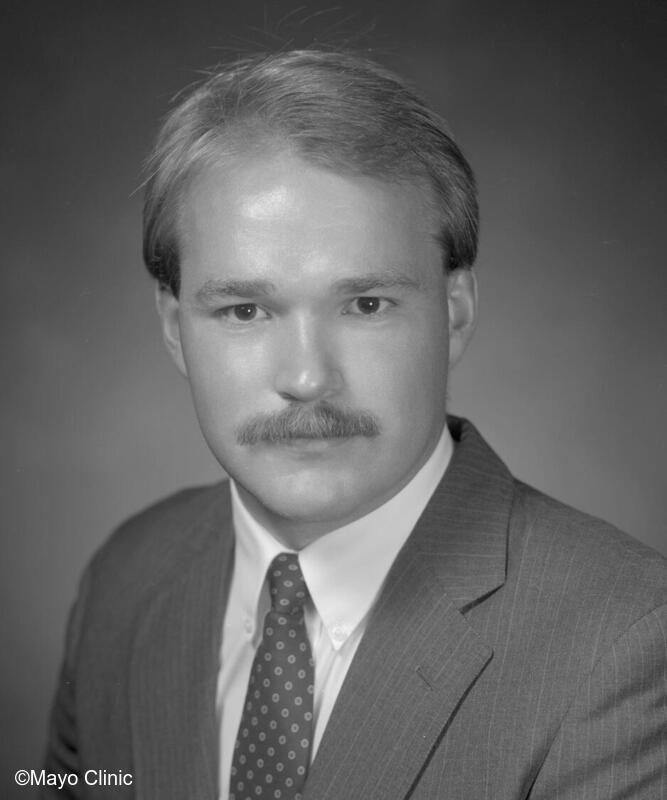
Mayo Clinic employee photograph of Dr. Charles Restall, undated.
Centennial Celebration First Month Update
Thank you for your readership. We are completing the first month of our 18-month period of celebrating the Centennial Anniversary of the department. The first six months from now until April 2024 will be used to provide background information on the department. During the actual anniversary year (April 2024 through April 2025), there will be a variety of events and activities. These include:
- A gala celebration dinner.
- A series of visiting professors at all three sites who will speak about the history of the department and impact on the specialty.
- A special session on Mayo Clinic at the 2024 Anesthesia History Association’s annual meeting and co-hosting the association’s 2025 annual meeting in Rochester.
- A number of historical vignettes about Mayo Clinic in Anesthesiology through the Centennial year.
- Two department-specific presentations in the series of dinners sponsored by Mayo Clinic’s Fye Center for History of Medicine.
- Progressive development of an expansive Mayo Clinic Anesthesiology history website, hosted as a section within the Mayo Clinic Heritage website. This website, Mayo Clinic | History and Heritage, is available to be accessed externally as well as internally
- Support for any and all of us to research, present, and publish department history.
Regarding research, presentations, and publications about our department’s history, I would like to introduce you to Alec Thicke (pronounced “THEE-kee”) and, for those who may not know him, Doug Bacon.

- Alec Thicke is an outstanding medical archivist who joined us for this Centennial Celebration. Alec serves within Mayo Clinic’s Fye Center for History of Medicine and is a remarkable source for historical materials related to the department. Alec is a Rochester native, graduating from Mayo High School. He has been an archivist for the Wisconsin History Society in Madison and St. Olaf’s College in Northfield, MN.

- Doug Bacon, M.D., is one of the world’s leading anesthesia historians. He was recognized by the Wood Library-Museum of Anesthesiology as its Laureate of Anesthesia History in 2012. Laureates carry that honor for 4-years; Doug is only one of eight individuals so recognized in the first 3 decades of the award (Dr. Douglas R. Bacon - Wood Library-Museum of Anesthesiology (woodlibrarymuseum.org). Doug was a member of our Rochester staff, chair both the Section on Anesthesia History and the South Division, from 2000-2012. Subsequently, he has been chair of the Departments of Anesthesiology at Wayne State University and the University of Mississippi. Doug retired from clinical practice and his Mississippi department chair role earlier this year and is now assisting our department with the Centennial Project.
We hope that a number of our trainees and staff members work with Alec and Doug to develop historical projects during the Centennial Celebration and far into the future. Our department is and will remain one of the world leaders in anesthesia history.
Speaking of leaders . . .
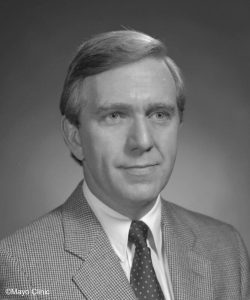
I’ve attached two great stories form our 2004 department newsletter. The first is about former Rochester department chair Alan Sessler and the second about one of the department’s most memorable clinicians, Charlie Restall. I think you’ll find them to be interesting and even entertaining.
- “Profile of Alan Sessler”: This summary encompasses two stories, one written by Peter Southorn and the other a set of reflections written by Mike Marsh. Peter is one of our most active emeritus professors. He is an astute observer of his colleagues and a prolific writer. He served as our department’s newsletter editor and co-wrote and edited our department’s history tome, Art to Science. This book was published in 2000. In many respects, our new department history website will be the next version of the book except that the website allows far more flexibility and inclusion of materials such as oral and video histories, links to many supporting materials such as digitized publications, etc. Mike formerly was a great anesthesiology and intensivist for us before leaving in 1991 to serve as long-term chair of the Department of Anesthesiology at Wayne State University.
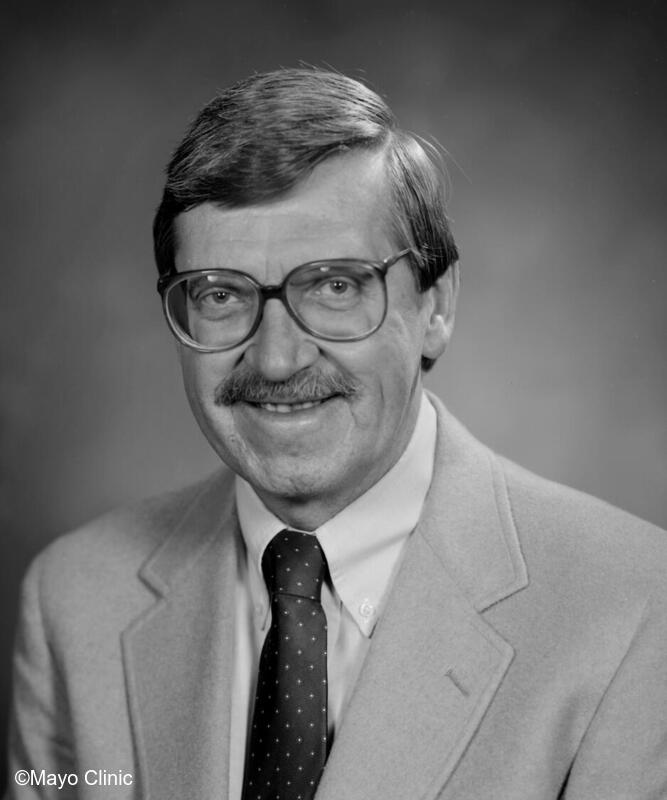
- “Fond Memories of Charlie Restall”: Written by Peter Southorn, this short summary provides hints into the amazing life of Charlie Restall. He was one of our many staff members who served in the military, with extensive action in WWII. He also is the subject of many of the department’s greatest, most humorous stories. He could be gruff and curmudgeonly as well as compassionate and soft as a teddy bear. Interesting reading.
Mystery Photos
Last week’s Mystery Photo was Jeff Ward.

Jeff served as the education coordinator for our Respiratory Therapy training program for more than 3 decades. During that period the program trained more than 350 respiratory therapists. Shirley Johnson partnered with Jeff during most of his time as overall education coordinator. Shirley served as the program’s clinical coordinator. Paul Didier and Dave Plevak were the medical directors of the program during most of Jeff’s time in his leadership role.
Here is this week’s Mystery Photo:
Please email your response at warner.mark@mayo.edu within 3 days of this update. I will also need your name and contact information. All correct responses will be placed into a drawing for a $10 Starbucks card. Only one winner per individual over the 80 weeks of Mystery Photos.
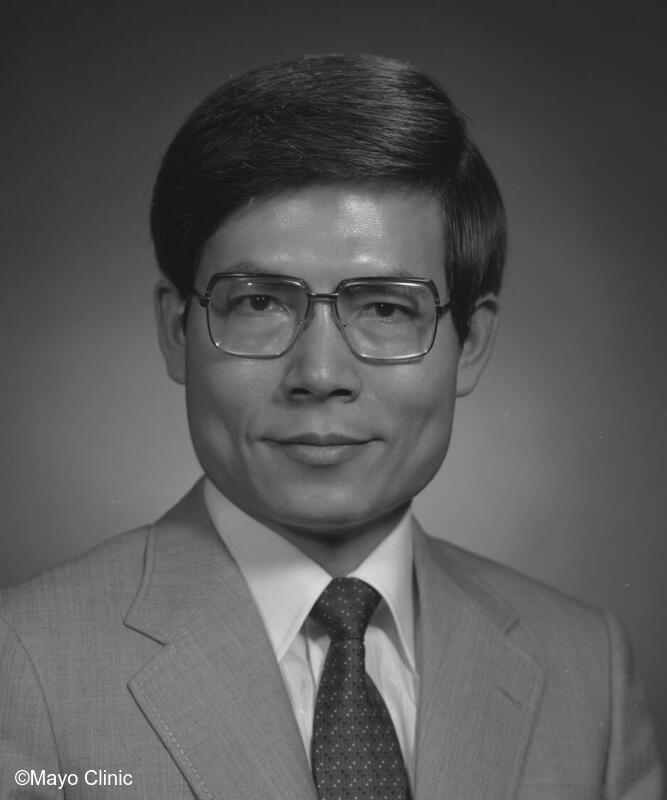



Photograph 1: Mayo Clinic employee photograph of Dr. Josef Wang, undated.
Photograph 2: Mayo Clinic employee photograph of Dr. Lee Nauss, undated.
Photograph 3: Mayo Clinic employee photograph of Dr. James Glenski, undated.
Photograph 4: Mayo Clinic employee photograph of Dr. Mark Warner, undated.
Photograph 5: Mayo Clinic employee photograph of Dr. Brian Dawson, undated.
Innovations: The Department and Neuraxial Opioids
Thank you for your readership and welcome to Update #5. And for those of you involved in guessing the people in our Mystery Photos, I sincerely appreciate your responses. We’ve had more than 150 responses to each photo thus far, with approximately 90% of them being correct.
We can be very proud of the multiple areas in which the department contributed to advances in the specialty and patient safety over the past century. Today and in the coming months, we will highlight a number of these innovations and the individuals who created them.
Our department played the lead role worldwide in establishing the safety and effectiveness of neuraxial opioids for pain relief. Peter Southorn provides a wonderful summary titled “The First Human Demonstration that Intrathecal Opiates Produce Pain Relief” of the work of Joe Wang and Lee Nauss in the late 1970s, with Joe initially studying the use of intrathecal narcotics in the laboratory and Lee administering the first dose to a patient. Their seminal paper “Pain Relief by Intrathecally Applied Morphine in Man” led to an international explosion of studies and the rapid introduction of both intrathecal and epidural opioid use in adults for perioperative analgesia into clinical practice.
In 1984, Jim Glenski, Mark Warner, and Brian Dawson took the next logical step and reported on a case series of children who experienced excellent pain relief with epidural opioids “Postoperative Use of Epidurally Administered Morphine in Children and Adolescents”. This was the first report of the use of neuraxial opioids in children.
Mystery Photos
Last week’s Mystery Photo was John McMichan.
John is originally from Melbourne, Australia and served as a critical care fellow in Rochester in 1976-7. After 10 years on staff in Rochester, he moved to Scottsdale to start the Department of Anesthesiology in Arizona. He served in that role for six years and has remained a strong advocate for the department in Phoenix and for the specialty. A special shout out to John for his leadership and service to Mayo and our department.
Here is this week’s Mystery Photo:

Please email your response at warner.mark@mayo.edu within 3 days of this update. I will also need your name and contact information. All correct responses will be placed into a Monday morning drawing for a $10 Starbucks card. Only one winner per individual over the 80 weeks of Mystery Photos.


Photograph 1: Mayo Clinic employee photograph of Dr. David Byer, undated.
Photograph 2: Mayo Clinic employee photograph of Dr. Kelly McQueen, undated.
International Care
Will and Charlie Mayo traveled the world to learn medicine and surgery. They also invited international guests to Rochester for stays between 4 and 12 weeks. They purchased a house on 2nd Street SW, immediately south of the current Mayo Building and it sat in the green space between what is now the Hilton Building and the Mayo Medical School. This house hosted international guests from 1895 through 1915. Each workday evening during these two decades, either Will, Charlie, or other Mayo staff members would gather the visitors in the house’s living room and talk about a topic of medical or surgical care. The goal was to share their knowledge with physicians from outside the U.S. and improve care far beyond Mayo Clinic.
Members of the Department have participated in this noble venture of working to improve care worldwide, especially in low resource countries. Here are two stories that highlight different approaches by two of our alumni:
- “And Especially the Children of Africa”. David Byer worked in orthopedic anesthesia at Methodist Hospital for more than 30 years and served as the long-term Minnesota representative to the American Society of Anesthesiologists Board of Directors. David passed away from complications related to multiple myeloma in 2014 (Mayo Clinic Alumni Association | David E. Byer, M.D. (ANES ’73). His favorite motto continues to inspire many of us, “Live simply; give generously.”
- “So Much Remains to be Done”. Kelly McQueen is one of our country’s leaders of global health and anesthesia initiatives. She was a resident graduate of Mayo Clinic Arizona and a fellow in obstetric anesthesia in Rochester. Currently, she is chair of the Department of Anesthesiology at the University of Wisconsin. You may read more about her at Kelly McQueen - Wikipedia.
The department has many wonderful colleagues in our physician and nurse anesthetist ranks who care for patients in low resource countries. Our trainees have the option of pursuing grants to serve overseas in low resource countries through the Mayo Clinic Global Health Program. In addition, Peace Eneh, one of our new Rochester staff members, and members of our Mayo Global Anesthesia interest group have organized a one-month training experience in Zambia. This pilot project will start this year with several residents and fellows, plus staff anesthesiologists. Hopefully, this program will soon expand to all anesthesia trainees and staff members across the institution.
Mystery Photos
Last week’s Mystery Photo was Jim Harper.

Jim served in the U.S. Army Special Forces from 1967-1970, then attended medical school at the University of Arizona. He joined our Rochester staff in 1982 and moved to Jacksonville to start our Florida department. He was chair of the department for 8 years.
Here is this week’s Mystery Photo:

Please email your response at warner.mark@mayo.edu within 3 days of this update. I will also need your name and contact information. All correct responses will be placed into a Monday morning drawing for a $10 Starbucks card. Only one winner per individual over the 80 weeks of Mystery Photos.


Photograph 1: Mayo Clinic employee photograph of Dr. Robert Devloo, undated.
Photograph 2: Mayo Clinic employee photograph of Dr. Emerson Moffitt.
Photograph 3: Mayo Clinic employee photograph of Dr. Roger White.
Cardiovascular Anesthesia
Mayo Clinic has been a leader in a number of surgical and anesthesia specialties. Today we will highlight the leadership roles of three extraordinary leaders in cardiovascular anesthesia: Drs. Bob Devloo, Emerson Moffit, and Roger White.
- Bob Devloo “A Pioneer in Cardiac Anesthesia”. Bob was from Belgium and experienced WWII during conflicts in India and Burma, learning how to deliver an anesthetic in the tropical heat for wounded soldiers. He trained at Mayo Clinic in 1948 and joined our staff in 1953. During his nearly 30 years on staff, he worked with John Kirklin, Dick Theye, Emerson Moffit, Roger White, John Tinker and others to establish one of the world’s finest cardiovascular surgery programs.
- Emerson Moffitt “A Pioneer in Cardiac Anesthesia”. Emerson was from New Brunswick, Canada and served in the Canadian Royal Navy before completing Dalhousie Medical School in Halifax, Nova Scotia. After a fellowship in Rochester, he joined our staff in 1957 and worked closely with distinguished scientists and clinician investigators such as Earl Wood, Jeremy Swan, and Dwight McGoon. His work helped the maturing field of cardiovascular anesthesia. He led our section of anesthesiology at St. Mary’s Hospital and was president of the Minnesota Society of Anesthesiologists. He left Mayo in 1972 to become dean of Dalhousie Medical School.
- Roger White “An Unsung Hero”. Roger is from Ontonagon, Michigan on Lake Superior and attended college and medical school at the University of Michigan. In 1965 he started his residency training in Internal Medicine in Rochester, but his training was interrupted by a 2-year stint in the U.S. Army. Upon his return, he joined the anesthesiology residency program and then the staff in 1970. He continues as an active, innovative leader now after 53 years as a consultant. Roger is one of the world’s leaders in emergency medical services and cardiac life support. His launch of an early defibrillation program in Rochester gained worldwide attention by producing the highest survival rate in the U.S. for out-of-hospital cardiac arrest.
Mystery Photos
Last week’s Mystery Photo was Virginia Hartridge.

Virginia was originally from Milwaukee and earned her M.D. from the Woman’s Medical College in Philadelphia. She served as an officer in the U.S. Army from 1942 through 1946 and while a medical student from 1946 through 1950. She transferred to the U.S. Navy after medical school and served as one of a small handful of navy women physicians on active duty. In 1953 she joined Mayo Clinic as an anesthesiology fellow and came on staff in 1956. She worked primarily in obstetric, general and orthopedic surgery, all at St. Marys Hospital, until her retirement in April 1982. Mary Ellen and I were privileged to share her retirement dinner with her on top of the Hilton Hotel in San Francisco at the annual meeting of the IARS, the last anesthesia meeting that she attended.
Virginia served as the director of our nurse anesthesia training program from 1956 through 1976. Like many other trainees who interacted with Virginia and as a young intern on an orthopedic surgical service, I knew her to be tough as nails. But as a young colleague during her last year on staff, I also knew her to be kind and gracious. Upon her death in 2001, she left most of her considerable estate to the Rochester Area Foundation to support women in domestic abuse situations and single mothers who struggle to raise their families. Her endowed fund continues to make an impact on these two areas today.
Last week’s contest winner was Bob Friedhoff.
Here is this week’s Mystery Photo. Over the course of the 80 weekly updates, the Mystery photos will vary in difficulty of recognition. I will note that this will be one of the more difficult photos for most alumni and staff to identify as he was in Rochester only a short time and quite a long time ago. However, his work at Mayo and elsewhere played a significant role in improving the perioperative care of children worldwide. It’s a very good story and worthy of highlighting with a Mystery photo.

Please email your response at warner.mark@mayo.edu within 3 days of this update. I will also need your name and contact information. All correct responses will be placed into a Monday morning drawing for a $10 Starbucks card. Only one winner per individual over the 80 weeks of Mystery Photos.
Photograph of Sonja Dawson and her husband Dr. Brian Dawson, undated.
Mayo Clinic Three Shield Logo
The Department of Anesthesiology has exerted considerable positive influence on the institution over the century. Many of the influences improved clinical practice, education, and research. However, none stands out for its clarity and impact than a simple napkin drawing created by Sonja Dawson, spouse of Brian Dawson, one of our first pediatric anesthesiologists. Peter Southorn tells the tale as only he can in this very interesting short story from the department’s newsletter from 2002 titled “Sonja Dawson and the Prototype Design of the Mayo Clinic Three Shield Logo”.
Peter describes Sonja’s original idea that the three shields would represent William Worrell Mayo (center) and his two sons, Charlie and Will, at his sides. It is interesting that the Mayo Clinic Board of Governors did not approve these Mayo family representations but instead substituted Education, Research, and Clinical Practice as the three shields. It has often been said that the biggest (center) of the shields represents the large clinical practice. However, that designation was never made by the Board of Governors. In fact, it can be reasonably argued that education or research could be the core (center) shield in that it was the Mayo Foundation for Medical Education and Research (MFMER), established by the Mayo families in 1915 through a large endowment to the University of Minnesota, that firmly established “the Mayo Clinic” as the non-profit educational institution that has trained more health care professionals than any other academic center in the U.S.
Mystery Photos
Last week’s Mystery Photo was David Hatch of London.

David was a fellow at Mayo Clinic in Rochester in 1967 and 1968. During his time with us, he was involved in cardiac anesthesia, caring primarily for children, and in our fledgling intensive care units with Alan Sessler. Kai Rehder convinced David to stay longer with a six-month opportunity in pulmonary research and he became Kai’s first research fellow. Upon returning to London, he became Consultant at Great Ormand Street Hospital and the world’s first professor of pediatric anesthesia. David made many major contributions to our understanding of the perioperative care of children, especially those cardiopulmonary defects. You may read more about David’s in this biography.
Here is this week’s Mystery Photo.

Please email your response at warner.mark@mayo.edu within 3 days of this update. I will also need your name and contact information. All correct responses will be placed into a Monday morning drawing for a $10 Starbucks card. Only one winner per individual over the 80 weeks of Mystery Photos.

Mayo Clinic employee photograph of Dr. John Michenfelder, undated.
Neuroanesthesia
Once in a while, I will highlight exceptional individuals and characters who stand out in our department’s history. This week’s subject is Jack Michenfelder. In the accompanying article, Ron Faust describes Jack’s many contributions to both the specialty and the department. Jack is perhaps best known for coining the term “neuroanesthesia” and serving as the editor-in-chief of Anesthesiology. There was, however, much more to Jack. I believe you will enjoy this story from one of the departments 2004 newsletters titled “Jack Michenfelder and the Achievement of Professional Respect”. For more information on Jack’s career, please see his obituary.
Mystery Photos
Last week’s Mystery Photo was Bernie Gilles.

Bernie was born in 1930 in North Dakota and served in the US. Army infantry during the Korean War. He subsequently became an outstanding nurse anesthetist in our department. He was very involved in much of the early pulmonary physiology research in our department and served as the nurse anesthetist partner to Alan Sessler as they developed the St. Marys intensive care units during the 1960s and 70s. Bernie and Alan built our respiratory therapy program and Bernie served as our clinical director for respiratory therapy for more than 20 years.
Here is this week’s Mystery Photo.

Please email your response at warner.mark@mayo.edu within 3 days of this update. I will also need your name and contact information. All correct responses will be placed into a Monday morning drawing for a $10 Starbucks card. Only one winner per individual over the 80 weeks of Mystery Photos.


Photograph 1: Mayo Clinic employee photograph of Dr. Keith Berge, undated.
Photograph 2: Mayo Clinic employee photograph of Renee Casewell,
Photograph 3: Mayo Clinic employee photograph of Dr. William Lanier, undated.
Hobbies
We’ve focused these first 10 weeks on department history and its role in the evolution of anesthesiologists, nurse anesthetists, and respiratory therapists. However, there is so much more to life than work. The following three stories provide a snapshot of the hobbies of three influential alumni/staff members.
- Keith Berge “Leading a Balanced Life”: Keith was born in Rochester and attended the University of Minnesota and Mayo Medical School. Steve Kunkle and I were able to convince Keith early in his ENT residency that he would love life better by working from the other side of the ether screen. Keith worked primarily in critical care and our neuroanesthesia division during his career in Rochester. He played a dominant national role in defining the risks of personal use of fentanyl and other narcotics by anesthesia professionals, making recommendations that have saved the lives of countless individuals over the years.
- Renee Caswell “A Stitch in Time”: Renee was born in Lindstrom, Minnesota and attended Moorhead State University and the University of Colorado College of Medicine. After residency and pain medicine training in Rochester, she joined our Rochester staff before moving in 1997 to Scottsdale. She was our Arizona residency program director from 2009-2016, associate dean of the School of Graduate Medical Education from 2003-2008, and recipient of Mayo’s Distinguished Educator Award in 2015.
- William Lanier “A Sporting Life”: Bill was born in Statesboro, Georgia and attended the University of Georgia and the Medical College of Georgia. After his residency training at Wake Forest, Bill was a Mayo Clinic fellow in neuroanesthesia and related research. He subsequently served as president of the Society for Neuroscience in Anesthesiology and Critical Care, was one of only a handful of “super-senior” examiners ever for the American Board of Anesthesiology, became the longest-serving editor-in-chief of Mayo Clinic Proceedings as it evolved to become one of the world’s most read and cited general medicine scientific journals, and received many honors during his career (e.g., the Mayo Clinic’s Distinguished Career Award).
Mystery Photos
Last week’s Mystery Photo was Richard (Dick) Theye.

Dick was from Ft. Wayne, Indiana, a graduate of Indiana University, and trained in anesthesiology in Indianapolis. After a stint in the U.S. Navy and a short time in private practice, he moved to Mayo Clinic and rapidly established his interest in clinical research, specifically pulmonary gas exchange, cardiac output, and regional oxygen uptake measurement during anesthesia. He became the first department staff member to be assigned dedicated research time and was instrumental in the research training of Jack Michenfelder and Kai Rehder. He served as department chair from 1971 through 1976 and was a director of the American Board of Anesthesiology. Sadly, he passed away from ALS in 1977 just as he was in the prime of his career.
Here is this week’s Mystery Photo.

Please email your response at warner.mark@mayo.edu within 3 days of this update. I will also need your name and contact information. All correct responses will be placed into a Monday morning drawing for a $10 Starbucks card. Only one winner per individual over the 80 weeks of Mystery Photos.

Photograph 1: Mayo Clinic employee photograph of Dr. Kai Rehder, undated.
Photograph 2: Mayo Clinic employee photograph of Dr. Russell Van Dyke, undated.
Halothane
Halothane was the first halogenated hydrocarbon volatile anesthetic. It’s introduction to clinical practice in 1955 was a huge advance for the safety of anesthesia as it soon replaced the more flammable ether and chloroform anesthetics. Within a few years, clinicians began to report patients who had developed postoperative liver dysfunction or “halothane hepatitis.” Several national studies in the U.S. and Great Britain confirmed the existence of this potentially fatal syndrome. The search was on to discover the risk factors associated with halothane hepatitis and its etiology.
Our department played a major role in elucidating the etiologies that can be associated with halothane hepatitis. Kai Rehder and Russell Van Dyke (in the photos below on the left and right, respectively) worked separately on this issue before joining our department in the mid-1960s and then collaboratively while in side-by-side laboratories at Mayo. They sought to determine whether halogenated volatile anesthetics, including halothane and methoxyflurane, were metabolized and if those metabolites were toxic to human organs. Their findings led to the currently accepted knowledge that the liver was the primary site for this metabolism and that the metabolites were toxic to the liver (halothane) and kidney (methoxyflurane). Even today’s halogenated anesthetics (i.e., isoflurane, sevoflurane and desflurane) have metabolites that can produce liver toxicity, albeit at a much lower rate than halothane. You can read Rehder’s paper from 1967 titled “Biotransformation of Halothane in Humans” and Van Dyke’s paper from 1973 titled “Biotransformation of Volatile Anaesthetics with Special Emphasis on the Role of Metabolism in the Toxicity of Anaesthetics”.
Russ and Kai’s efforts influenced anesthesia delivery worldwide for more than 4 decades, with clinicians avoiding the use of halothane in patients with liver dysfunction and the use of methoxyflurane in patients with renal dysfunction. Their work also led to the development and production of isoflurane, sevoflurane, and desflurane in ways that reduce the percentage of metabolites in humans. It is not an exaggeration to project that their efforts have saved hundreds, if not thousands, of lives in the past half century.
Mystery Photos
Last week’s Mystery Photo was Denise Wedel.

Denise was born in Duluth, Minnesota and received undergraduate and medical degrees from the University of Minnesota. After her Rochester residency, she served as a regional anesthesia fellow at Virginia Mason Clinic in Seattle. She joined our staff in 1982. She recently retired as an emeritus professor. Denise was responsible for re-invigorating the use of regional anesthesia in our Rochester practices and became one of the leading voices for regional anesthesia and its safe use internationally. She served as president of both the American Society for Regional Anesthesia and the International Anesthesia Research Society. She also was a long-serving editor for regional anesthesia and pain medicine in Anesthesia & Analgesia. She published extensively in regional anesthesia as well as malignant hyperthermia. She and protégé Terre Horlocker published the seminal recommendations on neuraxial anesthesia and the management of anticoagulants, impacting and improving the safety of patient care worldwide.
Here is this week’s Mystery Photo.

Please email your response at warner.mark@mayo.edu within 3 days of this update. I will also need your name and contact information. All correct responses will be placed into a Monday morning drawing for a $10 Starbucks card. Only one winner per individual over the 80 weeks of Mystery Photos.



Photograph 1: Edith Graham in nursing school, 1887.
Photograph 2: Florence Henderson, circa early 1900s.
Photograph 3: Carte de Visite of Isabella Herb, circa 1890s.
Anesthesia in Rochester – the Early Years
Edith Graham was not the first nurse to administer anesthesia. That honor appears to have belonged to Catherine Lawrence at the 2nd Battle of Bull Run in the American Civil War. However, Edith started nurse anesthesia at what is now Mayo Clinic in 1889 when William Worrall Mayo (Will and Charlie’s dad) trained her to administer ether. She was essentially the sole anesthetist for Will and Charlie until 1893, the year she married Charlie and stopped practicing as a nurse and nurse anesthetist. Edith’s sister, Dinah, also learned to administer anesthesia in 1893 as she worked with Dr. Augustus Stinchfield, the first non-Mayo to join the St. Marys Hospital practice. Dinah provided anesthesia for a short period of time for Augustus and presumably several of his patients. He primarily left the performance of surgeries to Will and Charlie and cared for the St. Marys Hospital and Rochester patients who did not need surgery. Unfortunately, Dinah’s anesthesia efforts are not well-documented, and it is not clear if she provided anesthesia for the patients of Will or Charlie or only for those of Augustus.
An excellent summary about Edith, her relatively short time as a nurse and nurse anesthetist, and her remarkable life of achievements as Mrs. Edith Graham Mayo can be found in this article by our own Darlene Bannon while she was a student in our Nurse Anesthesia Program titled “Edith Graham Mayo: Mayo Clinic’s First Nurse Anesthetist”. This article also contains fascinating insights into the initial difficulties that William Worrall Mayo and his sons had in the first few years of St. Marys Hospital in enticing patients to be admitted. Recall that in the 1880s and 90s, hospitals had very high mortality rates and few patients wanted to enter them. It was the great care provided by the Franciscan nurses and the surprisingly successful surgical outcomes of the Mayos that eventually attracted patients to Rochester and St. Marys Hospital over the course of that initial decade.
Fortunately, before leaving nursing in 1893, Edith trained her Chicago nursing school classmate, Alice Magaw, who was newly arrived in Rochester. Alice became one of the most famous nurse anesthetists of her time and Charlie fondly referred to her as the “Mother of Anesthesia.” In 1906, she reported on her experience of more than 14,000 anesthetics without a death attributable to the anesthetic in her review titled “A Review of Over Fourteen Thousand Surgical Anaethesias”.
By 1899, Will and Charlie were performing more than 1,600 surgeries annually. This required more than one operating room and additional people to deliver anesthesia. In 1899, they recruited Dr. Isabella Herb to move from Chicago where she had administered more than 1,000 anesthetics. With the move, Isabella became one of Mayo’s first women physicians and you can read more about her career in Robert Strickland’s, M.D., article titled “Isabella Coler Herb, M.D.: An Early Leader in Anesthesiology”. Alice Magaw primarily provided care for the patients of Will, and Isabella took over the patients of Charlie. Isabella left Rochester in 1904, leaving an opening. Florence Henderson, a new nurse who had started working at St. Marys Hospital in 1903, was recruited and trained by the Mayo Brothers to give anesthesia for Charlie’s patients. Joan Hunziker wrote about Florence’s career in an article titled “Voice and Touch: Florence Henderson on the Skills of an Ether Specialist”. She was to give more than 13,000 anesthetics for Charlie’s patients before leaving Mayo.
Mystery Photos
Last week’s Mystery Photo was Neil Feinglass.

Neil was born in Miami, Florida and earned his medical degree from Vanderbilt University. He trained in anesthesiology as well as critical care medicine at the University of Florida. After a one-year cardiothoracic anesthesia fellowship at Texas heart Institute with Arthur Keats, he moved to Rochester in 1987. In 1988, he transferred to Jacksonville, initiated intraoperative echocardiography services and chaired the Section on Cardiac Anesthesia at Mayo Clinic Florida. In 1998, he became one of the nation’s first board-certified echocardiographers in anesthesiology.
Here is this week’s Mystery Photo.
Please email your response at warner.mark@mayo.edu within 3 days of this update. I will also need your name and contact information. All correct responses will be placed into a Monday morning drawing for a $10 Starbucks card. Only one winner per individual over the 80 weeks of Mystery Photos.

Photograph 1: Mayo Clinic employee photograph of Dr. Matthew Crawford, undated.
Photograph 2: Photograph of Dr. Dennis Moriarity, undated.
Photograph 3: Mayo Clinic employee photograph of Dr. Edmund Carton, undated.
International Education and Fellows:
Will and Charlie Mayo often traveled overseas and strongly encouraged their colleagues to do the same. They understood the importance of learning from others and then sharing that knowledge when back home. Over time, they traveled abroad as invited guests, still learning, but now primarily teaching their colleagues overseas.
Their love and respect for education led them in 1915 to donate a significant amount of $1.5 million to the University of Minnesota to establish the Mayo Foundation for Medical Education and Research (MFMER). That donation would be worth more than $45 million in 2023. Proceeds from MFMER continue to support our medical and research education initiatives across the institution. These initiatives include funds that offset expenses of a number of national as well as international residents and fellows. Approximately 22% of all trainees in our Mayo Clinic School of Graduate Medical Education (MCSGME) across the institution come from outside the U.S. Our 25,000+ alumni of MCSGME have come from more than 180 countries worldwide. In a count performed in 2008, 84 of these countries had one or more alumni who had served as their prime ministers of health (or equivalent title).
The following stories from our department newsletters in 2007 and 2008 showcase three of our Department of Anesthesiology’s international anesthesia fellows, two from Dublin, Ireland and one from Sydney. Their contributions here within Mayo Clinic and back home highlight the continuing importance of working closely with our international colleagues in anesthesiology.
- Matt Crawford, Sydney: Matt came to Rochester in 1982 and stayed through 1985 as a special clinical fellow. He was a remarkable clinician, teacher, and researcher. His story titled “A Return Visit from Australia” from the department’s 2008 newsletter provides the highlights of his time at Mayo Clinic and describes his contributions to the evolution of pediatric perioperative care in Australia.
- Denis Moriarity and Ed Carton, Dublin: Denis came to Rochester in 1974 as a one-year fellow and was profoundly influenced by Jack Michenfelder, Kai Rehder, Rungson Sittipong, and Alan Sessler. Ed came to Rochester in 1988 as an outstanding liver transplant fellow. We were fortunately able to convince Ed and his wonderful wife, Louise, to stay longer. Ed completed a second fellowship (Critical Care Medicine) and then joined our faculty from 1990 through 1993 before he and Louise returned to Dublin. Both Denis and Ed have played major roles in Ireland’s anesthesia advancements and within the College of Anaesthesiologists of Ireland. You can read more about their accomplishments from a 2007 department newsletter article titled “The Rochester-Dublin Connection”.
Mystery Photos
Last week’s Mystery Photo is Tony Jones.
Tony was born in Anniston, Alabama and earned his M.D. at the University of Alabama, Brimingham (UAB) in 1982. After completing his anesthesiology residency in Rochester, Tony trained with Kai Rehder in the physiology of smooth muscle, with emphasis on mechanisms that are responsible for smooth muscle hypersensitivity and asthma. In 2006, Tony, Evelyn, and his children moved back to Birmingham where he was appointed to a named professorship and installed as chair of UAB’s Department of Anesthesiology and Perioperative Medicine. He has subsequently held many major leadership roles within the UAB Health System and its Heersink School of Medicine. He also has been at the forefront of leadership in U.S. anesthesiology as a member of the FAER Board of Directors and chair of the Board of Directors of the IARS. You may read more about Tony at Keith A. Jones, MD | AMGA and Meet medicine leadership in 2022, a series: Get to know Tony Jones, M.D. - Heersink School of Medicine News | UAB.
Here is this week’s Mystery Photo.
Please email your response at warner.mark@mayo.edu within 3 days of this update. I will also need your name and contact information. All correct responses will be placed into a Monday morning drawing for a $10 Starbucks card. Only one winner per individual over the 80 weeks of Mystery Photos.



Photograph 1: Mayo Clinic employee photograph of Dr. Laurence Torsher, undated.
Photograph 2: Mayo Clinic employee photograph of Dr. Paula Craigo, undated.
Photograph 3: Mayo Clinic employee photograph of Dr. Klaus Torp, undated.
Photograph 4: Mayo Clinic employee photograph of Dr. David Seamans, undated.
Anesthesia and Simulation
The specialty of anesthesiology has been a leader in the development of medical simulation, with anesthesiologists producing and introducing the first simulators in the context of resuscitation and subsequently intraoperative patient care. An excellent summary of the origin and introduction of anesthesia simulation in general can be found at Simulation Training and Skill Assessment in Anesthesiology - StatPearls - NCBI Bookshelf (nih.gov).
At Mayo Clinic, our department has played a major role in introducing simulation into all of our training programs, anesthesiology and otherwise, and has been a leader nationally in advances in simulation. In Rochester, leaders of our anesthesia simulation programs were Laurence Torsher and Paula Craigo. Laurence started our Rochester program in 2005. Their colleagues in Arizona and Florida were Dave Seamans and Klaus Torp, respectively. Dave started the Arizona program in 2010 and Klaus followed in 2011 in Florida.
Laurence has provided a brief summary of our department’s evolution of simulation “Simulation in Anesthesia at Mayo Clinic”. He also has written an excellent review of the use of simulation in medical education in general that provides more insights into the overall development of this education-related field “History of Anesthesia Simulation”. Note that our department was one of the first five in the U.S. endorsed for providing instruction in simulation to fulfill MOCA credits as required by the American Board of Anesthesiology. Laurence and Paula deserve our thanks and admiration for the remarkable efforts they put into achieving this distinct honor. Dave and Klaus made remarkable inroads to place our department in simulation leadership roles in Arizona and Florida.
Mystery Photos
Last week’s Mystery Photo is Martin Abel.
Martin is from Johannesburg, South Africa and earned his medical degree at the University of Witwatersrand. After training in anesthesiology at Charing Cross Hospital in London and a fellowship in cardiovascular anesthesiology at Mt. Sinai Hospital in New York City, he moved to Rochester as a Special Clinical Fellow in Cardiovascular Anesthesiology and Critical Care Medicine. He joined the staff in 1982. Martin introduced the use of intraoperative echocardiography into our practice and has been a long-serving member of the American Society of Echocardiography’s Intraoperative Council and ASA’s Transesophageal Echocardiography Task Force. He chaired our Rochester Division of Cardiovascular and Thoracic Anesthesiology for 12 years and moved in 2017 to become chair of our department in Jacksonville. In that capacity, he has nearly doubled the size of the department and led to the major growth of its clinical and academic activities.
Martin is a master clinician, recognized with multiple department clinician and teacher of the year awards. He is one of only three Rochester-based department members to have received the Mayo Clinic’s Distinguished Clinician Award (2005). The other two from Rochester were Sait Tarhan (1993) and Mary Ellen Warner (2010). Two of our Arizona-based department members have received this award, Joel Larson in 2005 and Terry Trentman in 2018. Roy Cucchiara received this award for his work in our Florida department in 2005.
Interestingly, 3 of the 5 recipients of the Mayo Clinic Distinguished Clinician award across the institution in 2005 were anesthesiologists from each site of our department (Abel, Cucchiara, and Larson). That year was very special for the department as it was also in 2005 that we had members who served as either the president, president-elect, or immediate past president of 6 of the 8 major anesthesia subspecialty societies. To my knowledge, no other department in the country has ever achieved that distinction.
Here is this week’s Mystery Photo.

Please email your response at warner.mark@mayo.edu within 3 days of this update. I will also need your name and contact information. All correct responses will be placed into a Monday morning drawing for a $10 Starbucks card. Only one winner per individual over the 80 weeks of Mystery Photos.



Photograph 1: Mary Ellen Warner, M.D., undated.
Photograph 2: Marlea Judd, RN, CRNA, undated.
Photograph 3: Steve Osborn, RN, CRNA, undated.
Photograph 4: Brad Narr, M.D., undated.
Photograph 5: Steve Jorgenson, M.D., undated.
Gonda and its Outpatient Procedure Centers
In the late 1990s and early 2000s, anesthesia department across the country and abroad were being requested to provide an increasing number of non-operating room anesthetics (NORA). These new outpatient procedures were great for patients and proceduralists but difficult to staff from an anesthesia perspective. Often, several anesthesia professionals were needed to care for a single patient who had complex needs in a remote site. The rapid expansion of requests for NORA did not promote an efficient practice and was one that contributed to a shortfall of anesthesia providers everywhere, including Mayo Clinic in all sites. There were also major concerns about patient safety, especially in the early days of NORA expansion.
In Rochester, we were fortunate to have leaders such as Brad Narr and Mary Ellen Warner involved in the development of plans for the new Gonda Building. Although the initial plans did not include any space to consolidate outpatient procedure practices, we were able to convince the institution that we could ensure patient safety and improve surgical efficiency by integrating consolidated outpatient procedural practices into the building design. We were granted procedure centers on three levels of the building, an institutional decision that resulted in a very positive impact on Mayo finances, patient safety and satisfaction, and surgical efficiency.
Mary Ellen, Marlea Judd, Steve Osborn, Brad Narr, and Steve Jorgensen led the development of these procedural practices. They were able to take advantage of several opportunities that allowed new practice models, cost-savings, and increased patient and provider satisfaction. These opportunities included Minnesota’s decision to opt-out of Centers for Medicare and Medicaid Services (CMS) requirements of medical direction of nurse anesthetists; an agreement between our department and the Upper Midwest Medicare carrier, Blue Cross/Blue Shield to allow us to use a non-medically directed anesthesia payment model and receive strong compensation for our services; and a collaboration between our department and the Mayo Department of Nursing that allowed our department to directly hire the nurses who staffed these procedural centers. The latter promoted robust cross-training and work efforts between nurses, CRNAs, and our physicians, all leading to excellent satisfaction in the practices and high efficiency of throughput, room turnover times, etc.
The story about this remarkable transition and its start with a single procedural center on Gonda 7 was first provided by Mary Ellen in a 2007 department newsletter in an article titled “Gonda Outpatient Procedure Center”. The care models developed by the team triggered a rush of institutions to send representatives to Rochester to learn what we had done and how we had done it. More than 75 institutions worldwide visited the Gonda 7, 2, and 15 practices between 2003 and 2013 and all implemented either our practice model or modifications of it. Future Centennial Updates will describe the development of Mayo Clinic outpatient surgical centers in Arizona, Florida, and the Mayo Clinic Health System.
Mystery Photos
Last week’s Mystery Photo is Peter Southorn.

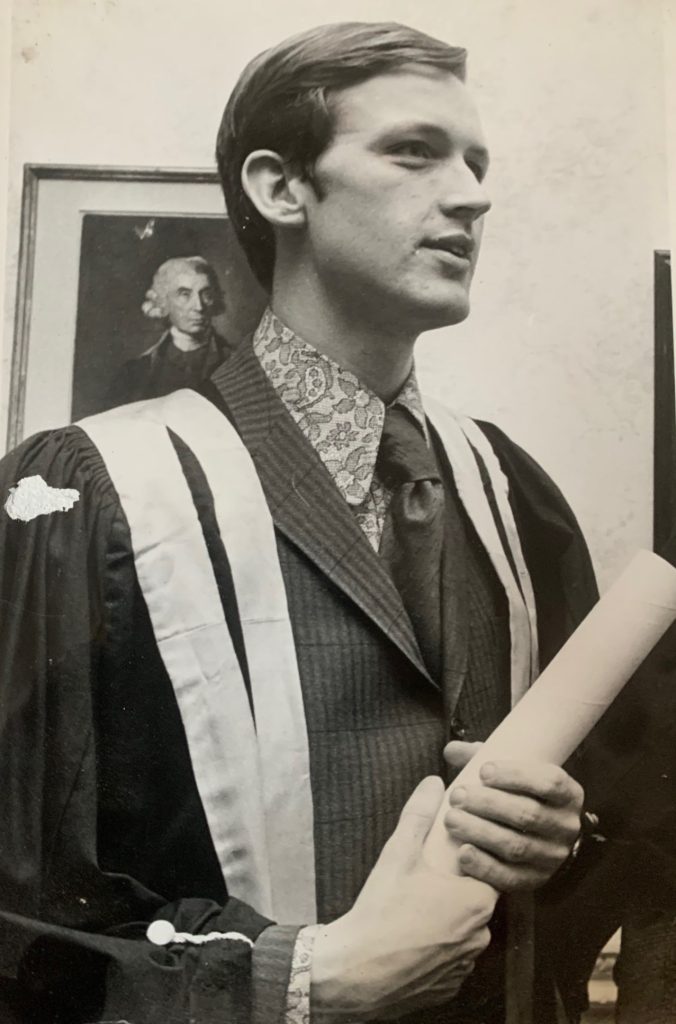
Peter is from northeast England near Newcastle upon Tyne. He attended undergraduate and medical school at University College in London. After extensive anesthesia training in London, he moved to Rochester in 1973 for a one-year fellowship. He returned to University College as a staff member before making his definitive trip across the Atlantic to join our Mayo staff in 1976. During his career he made major contributions to the evolution of our critical care activities, led enhancement of our intraoperative and ICU patient monitoring capabilities, and was very involved in the development of our solid organ transplant services. Peter played major roles in Mayo’s medical school (admissions committee) and the Mayo Alumni Association (executive committee member). A quiet leader, he was a founding member of the American Society of Critical Care Anesthesiologists (currently named the Society of Critical Care Anesthesiologists) and president of the Minnesota Society of Anesthesiologists.
To many of us, Peter is best known for his gracious demeanor, crooked surgical hat, ready smile, and willingness to help on any project. Peter, Alan Sessler, and Kai Rehder wrote our department’s history in “Art to Science.” That book will be revised in 2025 at the conclusion of the Centennial Celebration.
Here is this week’s Mystery Photo.

Please email your response at warner.mark@mayo.edu within 3 days of this update. I will also need your name and contact information. All correct responses will be placed into a Monday morning drawing for a $10 Starbucks card. Only one winner per individual over the 80 weeks of Mystery Photos.
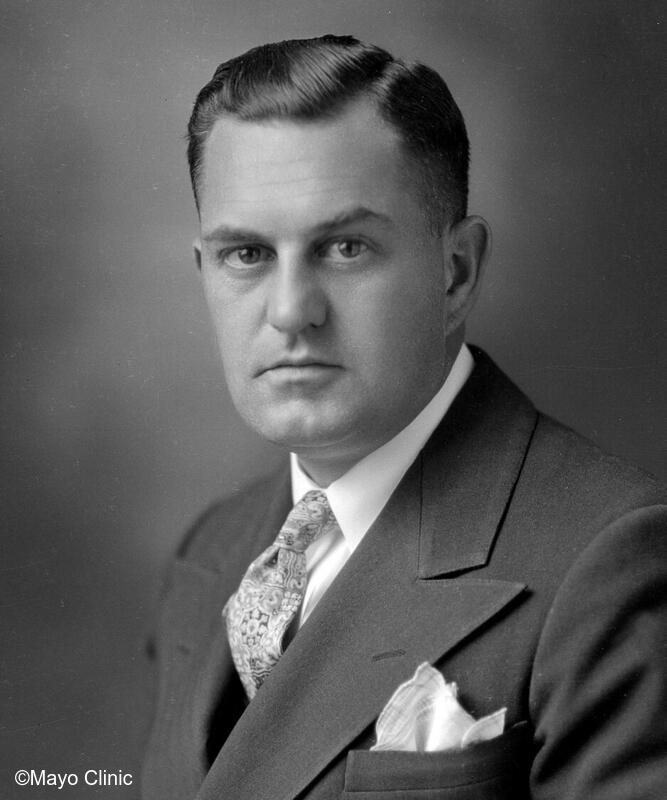
Mayo Clinic employee photograph of John Silas Lundy, M.D., 1934.
Mayo Clinic, the American Board of Anesthesiology, and the Evolution of the Specialty
In a previous Update, we discussed the evolution of anesthesia at Mayo Clinic and the remarkable achievements of our earliest nurse anesthetists. The physician side of anesthesia developed more slowly, with modest advances during the first decades of the 20th century. Our own John Lundy and the University of Wisconsin’s Ralph Waters, a 1926 Mayo alumnus, were two of the leaders who spearheaded efforts to have anesthesiology recognized as an academic specialty. They pushed hard to develop certification in anesthesiology. Specifically, they were able to convince the American Board of Surgery to provide anesthesia certification in 1937. This led to the incorporation of the American Board of Anesthesiology (ABA) the next year as an affiliate of the American Board of Surgery. In 1941 the American Medical Association’s Council on Medical Education and the American Board of Medical Specialties approved the ABA as an independent certifying board. John Lundy’s influence with the American Medical Association provided the push to get final approval.
Lundy was appointed as one of the nine founding members of the ABA. For the next 18 years he influenced the ABA as it guided the fledgling specialty’s evolution, establishing norms for the certification of individual physicians and setting standards in education and research for anesthesiology training programs. What he lacked in political finesse in the ABA and national specialty societies, he made up for with a dominant personality and tenacity. He and Waters often disagreed on how the specialty should develop. The early ABA directors fell into two cliques: those linked to John Lundy and those linked to Ralph Waters. Lundy recruited a number of former Mayo trainees to become ABA directors. These included alumni Ralph Tovell, Charles McCuskey, Ed Tuohy, and Albert Faulconer. His efforts started a cascade of Mayo Clinic alumni who have served as directors of the ABA for 75 of the 85 years of its existence. No other department has provided more directors to the ABA. In addition, more than 100 department alumni from Rochester, Arizona, and Florida have served as examiners for the ABA or participated in the development of the ABA’s primary and subspecialty certifying examinations. The department’s sustained support for the academic development of the specialty and the certification processes of the ABA is astounding.
Why is Mayo Clinic’s continuous leadership in the ABA important? The ABA is one of the most influential organizations in U.S. anesthesiology because it determines the criteria for board certification. Training programs, through standards established by the Anesthesiology Review Committee of the Accreditation Council for Graduate Medical Education (ACGME), need to adapt to the criteria set by the ABA. As a consequence, much of the academic progress of the specialty is guided by the ABA.
Here is a list of 11 Mayo Clinic directors of the ABA. Note that Mark Keegan currently is the ABA Treasurer (Mark T. Keegan, M.B., B.CH. - The American Board of Anesthesiology (theaba.org).
- John Lundy (1938-1955)
- Ralph Tovell (1938-1949)
- Charles McCuskey (1940-1953)
- Edward Tuohy (1950-1955)
- Albert Faulconer (1955-1969)
- Robert Patrick (1962-1974)
- Richard Theye (1969-1976)
- Alan Sessler (1977-1989)
- Mark Warner (1998-2010)
- David Warner (2010-2022)
- Mark Keegan (current)
Mystery Photos
Last week’s Mystery Photo is Pauline Bisel.

Pauline is from Co. Meath, Ireland. She was one of twelve children and grew up in the country 30 miles north of Dublin. Following her elementary and secondary education she completed a two-year program on the care of children at St. Clare’s Dietetic Hospital in Co. Meath. On completion of this she worked for several years at St. Mary’s Hospital for children in Baldoyle, Dublin. Most of the patients were children who had post poliomyelitis complications.
In her early twenties she decided to become a Catholic nun joining a community in New York State involved in the care of the elderly. After two years in this endeavor she realized she could not spend her life living with all women! She returned home to Ireland and after a short while travelled to England where she attended the Chelmsford School of Nursing in Chelmsford, Essex. While there she met and married her husband Steve who was serving in the United States Air Force.
Upon returning to the United States she worked for several years in various hospitals in different states gaining experience in multiple specialties including intensive care. During this time she and Steve were blessed with two daughters.
In 1979 Pauline applied to the Nurse Anesthetist program at Mayo Clinic, in Rochester, MN. As she drove to her interview in Rochester, she recalled first reading about Mayo Clinic in a book she discovered in her uncle’s house when she was 9 or 10 years old. At that time Mayo Clinic and Rochester, Minnesota were a very long distance away. The mere thought she could be there one day was absurd. At this interview she recalls meeting the esteemed Dr. Peter Southorn who impressed her with his warmth and sincerity.
She entered the Nurse Anesthetist program in September 1979 and upon graduating stayed on as staff anesthetist at St. Mary’s Hospital. The first two years were in Cardiac Anesthesia where she was very fortunate to be involved in pediatric cardiac anesthesia under the tutoring and mentoring of Drs Beynan and Raimundo. Pauline’s love for taking care of children was clearly met. In 1987 Dr. John McMichan invited her to join the anesthesia group going to Scottsdale, Arizona. It was a department of three MDs and one CRNA. This move created unique challenges. The local anesthesia providers were not welcoming CRNAs. However, over time and due to the excellent health care Mayo Clinic provided to the community acceptance was gained. Even though challenging this was also a very exciting time.
After eleven years Pauline stepped down from administrative duties to be a full time clinical anesthetist. For several years she travelled to Mexico and Haiti with a small Mayo group who were part of International Medical Assistance. This was a very rewarding experience. Pauline retired in 2013 after thirty-two years on staff. In retirement she continues aiding her neighbors to the south by being part of a small group of Mayo Clinic Colleagues offering mobile medical clinics in Ensenada, Mexico.
Here is this week’s Mystery Photo.

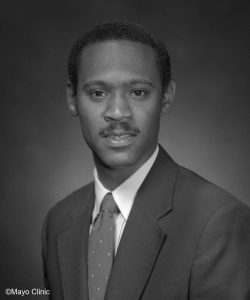
Dan Cole, M.D., undated.
Our Mayo Clinic Department of Anesthesiology’s Heritage Website
First An Apology,
Upon reading Update #16 last week, I was aghast to learn that I failed to include one of my best friends and closest colleagues, Dr. Dan Cole, from the list of Mayo Clinic anesthesiologists who have served as a director of the American Board of Anesthesiologists. My sincere apology to Dan. Dan served as chair of our Mayo Clinic Arizona department from 2003 through 2014. Dan currently is my successor as president of the Anesthesia Patient Safety Foundation and Professor of Anesthesiology at UCLA. I have corrected this omission in an amended Update #16 as it will join the other updates in a compilation on our new department heritage website. While I made the initial mistake, it will be corrected when our colleagues access the updates into the future.
Our archivist, Alec Thicke, and I met this past week and reviewed the Phase One model of our new Heritage Website. It will be an outstanding site for archiving our department’s history. We hope to have initial public access to the Heritage Website by the middle of January. In it, you will find a compilation of the updates, as well as early entries into distinct webpages dedicated to audio and video recordings, information about our colleagues who have served in the military, photos, publications related to our department’s history, and a variety of links. As the website evolves over 2024’s centennial year, we’ll add a digitalized Art to Science, the department’s history book edited by Kai Rehder, Peter Southorn, and Alan Sessler. We believe this website will be the finest anesthesiology department website in the country, if not the world, as it evolves.
Phoenix, Arizona: Home to Many Mayo-Trained Anesthesiologists
Clearly, we’ve made significant advances and had huge growth of our Department of Anesthesiology in Arizona over the past 35 years. In Update #5 (October 5th, 2023) we highlighted John McMichan, our colleague who first chaired the department. We also highlighted Pauline Bisel in Update #16th (December 21st, 2023), our first nurse anesthetist supervisor in the department.
Our graduating residents have also made a significant impact on anesthesiology in “the Valley” in private practice. In this 2007 article from our department newsletter, Joe Sanders (Class of 1990) reflects on his time at Mayo Clinic in Rochester and comments on Valley Anesthesiology Consultants and the many Mayo alumni who served in that group at that time. Since that article was written, the dynamics and organization of anesthesia provision in the Phoenix area has evolved but we still have many alumni actively involved. Many of you will recognize the alumni noted in Joe’s article.
Mystery Photos
Last week’s Mystery Photo is Bill Oliver.

Bill was born in Panama City, Florida and attended school at the University of Alabama. He was probably the biggest booster ever of Coach Bear Bryant (and later Nick Saban) and the University of Alabama football team. He was a nice guy, regardless. Ha!
After graduating medical school in Birmingham, Alabama in 1983, he moved to Rochester as resident in our department. Bill went on to become one of our most respected and beloved anesthesiologists. He was legendary in his devotion and dedication to children with complex congenital heart disease. Even though personally limited at times by flare ups with cystic fibrosis, he had prodigious levels of energy and tenacity when it came to caring for “his kids.” His compassion was boundless. He received the honorary Humanitarian Award from the Mayo Alumni Association for his dedication to children who have congenital and chronic diseases. He trained many of us in pediatric cardiac anesthesiology and earned the academic rank of Professor of Anesthesiology. Sadly, Bill passed away at age 62 in 2018. Fittingly and not surprisingly, he was on call for the postoperative intensive care unit and its complement of congenital heart disease children that evening.
Here is this week’s Mystery Photo.

Please email your response at warner.mark@mayo.edu within 3 days of this update. I will also need your name and contact information. All correct responses will be placed into a Monday morning drawing for a $10 Starbucks card. Only one winner per individual over the 80 weeks of Mystery Photos.



Photograph 1: Sten Lindahl, M.D., undated.
Photograph 2: Petter Steen, M.D., undated.
Photograph 3: Jukka Rasanen, M.D., undated.
A Scandinavian Connection
Ever since Will and Charlie started inviting international guests to Rochester, we’ve had visitors who have been interested in anesthesia delivery at Mayo Clinic. They started the International Surgeons Club in 1906 and purchased a home on 2nd Street SW, now immediately south of the Mayo Clinic Building and between the Hilton Building and Mayo Medical School. As many as 30 surgeons and medical leaders from around the world visited at a time for periods ranging from 2 to 8 weeks. They were able to observe daily patient evaluations and surgeries. As noted by Charlie, the Mayo institution should help develop with professional education “a system of medicine which will combine the best elements to be found in all countries.”
The professional education associated with the Surgeons Club provided great exposure of the visitors to evening lectures by the Mayo brothers and their colleagues. However, with the development and implementation of the Mayo School of Graduate Medical Education in 1915, in conjunction with the University of Minnesota, the need for the Surgeons Club dissipated and the club ended in 1916. At that point in time, departments served as the hosts of these visitors, with many departments creating visiting clinician and research positions.
Our department was very involved in accepting international visitors from around the world. Today, we’ll focus on three anesthesiologists from Scandinavia who joined us for various lengths of time and who have gone on to make major contributions to the specialty and medicine in general.
- Sten Lindahl (Sweden): Sten was born in Malmö, Sweden and received his M.D. in 1971 from the University of Lund. After 5 years of training in pediatrics, he completed a 4-year residency in anesthesiology. During his residency training, he also completed a Ph. D. He served as the head of pediatric anesthesia at the University of Lund during the 1982-1986 period and, during that time, spent 6 months in research with Mayo alumni David Hatch at Great Ormand Street in London and a similar period with Kai Rehder here in Rochester. Sten moved to Rochester in 1986 for three years and made major contributions to our understanding of thermogenesis in neonates and pulmonary mechanics in infants and toddlers. A story from our department newsletter in 2006, titled “Scandinavia and Mayo Anesthesia” describes his time in Rochester. He returned to Sweden in 1988 and, in 1990, was appointed chair of the Department of Anesthesiology and Intensive care at the Karolinska Hospital and Institute in Stockholm. He served multiple years on the Nobel Prize Committee on Physiology and Medicine, including several years as chair of the committee. He also has been president of the Scandinavian Society of Anesthesiology and Intensive Care.
- Petter Steen (Norway): Petter was born in Oslo, Norway and received his M.D. in 1972 from the University of Oslo. He also earned his Ph.D. in 1979 from the same institution. He came to Mayo Clinic in 1978 and worked primarily with Jack Michenfelder on cerebral ischemia studies. He also published cardiac studies with John Tinker and Sait Tarhan. After that year in Jack´s lab and his return to Oslo, he would return from Norway for a month each year for the next decade, often bringing research fellows from Norway with him. He returned to the University of Oslo and, in 1982, was appointed as chair of its Department of Anesthesiology. In 1992, he transitioned to the university’s Division on Prehospital Care and was appointed as a professor of Emergency Medicine. After a remarkably prolific academic career with multiple anesthesia-related publications, his focus shifted to resuscitation. He has served on the European Resuscitation Council, chaired the World Federation of Societies of Anaesthesiologists’ Committee on Cardiopulmonary Resuscitation, and as a member of the European Academy of Anaesthesiology. Petter co-chaired the International Liaison Committee on Resuscitation (ILCOR), a committee that publish the CPR guidelines with American Heart Association (AHA). Amongst other efforts and recognitions, Petter received a Lifetime Achievement Award from AHA and ILCOR; worked in Romania during its 1989 revolution and in a field hospital during the civil war in Kosovo; taught in Gaza, Lebanon and Syria; and ended up being knighted by the King of Norway. Today, his work has been cited more than 21,000 times, making him one of the specialty’s most influential researchers in Europe.
- Jukka Räsänen (Finland): Jukka was born in Lahti, Finland and received his M.D. from the University of Helsinki in 1978. After his anesthesiology residency at that same institution, he moved to Columbus, Ohio as a Critical Care Medicine fellow. He returned to Helsinki and directed pediatric critical care at the Children’s Hospital. In 1990, he moved to Tampa, Florida and joined the University of South Florida’s Department of Anesthesiology. During this time, he worked with John Downs, M.D. and expanded his research in respiratory mechanics in acute lung injury and the use of novel technologies to detect each pulmonary deterioration. We were able to entice him to come to Rochester in 1997. During his time until his retirement in 2013, Jukka served as chair of our Division of Multispecialty and did extensive work in our pediatric ICUs. He also served as medical director for Smile Train International. While at Mayo Clinic and in retirement, he has continued to be involved in multiple medical missions overseas.
Mystery Photos
Last week’s Mystery Photo is Roy Cucchiara.

Roy was born and raised in New Orleans. After medical school at Louisiana State University, he interned at Charity Hospital in New Orleans. He moved to Rochester and completed his residency and a fellowship in neuroanesthesia in 1973. He subsequently served two years in the U.S. Army at Walter Reed Army Medical Center in Washington, DC before returning to Rochester.
Upon his return to Rochester, he joined one of the country’s most prestigious and influential neurosurgical and neuroanesthesia practices, working (over a period of time) with luminary neuroanesthesia colleagues such as Jack Michenfelder, Joe Messick, Gerry Gronert, Ron Faust, Leslie Milde, and Bill Lanier. His surgical colleagues were also internationally recognized and included Collin MacCarty, Ross Miller, Thor Sundt, Burt Onofrio, Ed Laws, PJ Kelly, Ross Miller, Rick Marsh, and Fred Meyer. Together, they brought huge recognition to Mayo Clinic and were prolific contributors to our understanding of neuroanesthesia and neurosurgery.
Roy was a trainee’s dream educator. He could speak to any topic and always had time to teach anyone. He was an excellent educator, whether one-on-one at the bedside, in the classroom, or in front of 1,000 ASA members during his prolonged run of outstanding refreshers courses on neuroanesthesia at ASA annual meetings. He was an exceptional oral examiner for the ABA. One of his favorite philosophies was that you could be “good and slow or good and fast” . . . and no one was faster or better than Roy with assessing, inducing, and caring for neurosurgical patients with complex morbidities. His extraordinary clinical skills carried through his career. In 2005 Mayo Clinic honored him with one of only five Distinguished Clinician Awards throughout the institution that year.
He was chair of our Rochester Department of Anesthesiology from 1988 through 1991, then subsequently served as chair of the anesthesia department at the University of Florida (1993-1997) and interim chair of our Mayo Clinic Florida department (2003-2004) during his stellar career.
Here is this week’s Mystery Photo.

Please email your response at warner.mark@mayo.edu within 3 days of this update. I will also need your name and contact information. All correct responses will be placed into a Monday morning drawing for a $10 Starbucks card. Only one winner per individual over the 80 weeks of Mystery Photos.


Photograph 1: John Pender, M.D., undated.
Photograph 2: John Hattox, M.D.
California, Here We Come . . .
Who would have thought that Rochester, Minnesota, and California would be two of the most alluring locations in the country for young physicians after World War II? OK, perhaps not alluring but certainly great locations in which to learn (Rochester) and practice (California) anesthesia. Today we’ll focus on two WWII veterans who trained and worked at Mayo Clinic during and after the war. Both went on to long, distinguished careers in California, one a leader of Palo Alto Medical Clinic and Stanford University Medical Center and the other the primary leader of Anesthesia Service Medical Group of San Diego, a group that at one time was the country’s largest anesthesia private practices.
- John Pender: John trained at Mayo Clinic from 1940 through 1942 before being pulled to active duty in the U.S. Navy Reserves from 1942 to 1946. At the conclusion of the war and his assigned duty, John returned to Rochester where he worked until 1954. Upon settling in 1954 in Palo Alto, he continued to be involved in academic anesthesia with his association with Stanford University. He also played major roles in academics and the specialty, including serving as Associate Editor for Anesthesiology, chair of the AMA’s Section on Anesthesia, a trustee of the Wood Library and Museum (WLM) of Anesthesiology, and president of the Academy of Anesthesiology. John was a strong supporter of anesthesia history and the WLM. In 2001, at his request, the Pender family established the “Mayo Clinic Room at the WLM”. The linked article also provides an excellent story about John’s life. In his honor, the foundation named its oral history collection after him (Living History Interviews - Wood Library-Museum of Anesthesiology (woodlibrarymuseum.org)). Mayo alumni who are highlighted in the Pender Collection include:
- John Lundy
- Charles McCuskey
- John Pender
- T. Harry Seldon
- Ralph Waters
- John Hattox
- John “Jack” Michenfelder
- Mark Warner.
- John Hattox: After completing an internship and three additional months in anesthesia training at the U.S. Naval Hospital in San Diego at the end of WWII, John was a little shocked to learn that his first assignment would be as chief of anesthesiology in the same hospital, one of the largest in the U.S. at the time with more than 1,000 beds. This is one of many great stories about John. Bob Adams; a 1971 graduate of our Rochester anesthesia training program, a former staff member from 1973-1974, and son of Charles Adams, the department’s second chair from 1952 to 1953; has written a wonderful summary of John’s contributions to the specialty in 2004’s department newsletter titled “John S. Hattox Jr., M.D.”. John was discharged from duty in 1948 and chose Mayo Clinic for his anesthesia training. After completing his training in 1950, John moved back to San Diego and joined a relatively new private practice group, Anesthesia Service Medical Group. In addition to providing outstanding leadership to what was to grow to be a group of nearly 200 anesthesiologists in the 1990s, he became very involved in anesthesiology professional organizations. John was president of the California Society of Anesthesiologists in 1967 and president of the American Society of Anesthesiologists (ASA) in 1980. He is one of 10 Mayo alumni/staff members to have received the ASA’s Distinguished Service Award. There have been 76 of these award winners, overall. The Mayo recipients include:
- Ralph Waters (1946)
- John Lundy (1948)
- Ralph Tovell (1951)
- Charles McCuskey (1953)
- Ralph Knight (1960)
- Jack Michenfelder (1990)
- John Hattox (1992)
- Alan Sessler (2001)
- Mark Warner (2018)
- Dan Cole (2020).
Mystery Photos
Last week’s Mystery Photo is John Tinker.

John was born in Cincinnati, Ohio. His father was, for a time, a tennis teaching professional, and John became one of Ohio’s best high school tennis players in the late 1950s. After earning his M.D. degree at the University of Cincinnati as valedictorian of his 1968 graduating class, he trained in anesthesiology at the Peter Bent Brigham Hospital in Boston where he excelled but also sparked controversy in a surgeon-dominated institution. This linked historical case report about John provides interesting insight into understanding John’s penchant to challenge authority and conventional wisdom (Anesthesia in the late 1960s at Peter Bent Brigham Hospital, Boston: A case report - ScienceDirect). To various degrees, he carried this attribute of challenging authority and accepted practices and behaviors through his entire career, primarily to push for improvements in patient safety but at times to the detriment of his career.
After a two-year stint in the U.S. Army reserves from 1972 to 1974, John moved to Rochester in 1974. For the next decade, he and Jack Michenfelder were arguably our department’s most visible members to the general anesthesia community as they gave refresher courses and other presentations at nearly every major anesthesia meeting. John was an outstanding cardiac anesthesiologist and a prolific investigator and writer. His work with Jack on issues such as nitroprusside toxicity and colleagues such as Sait Tarhan on perioperative myocardial injury and its epidemiology and etiologies dramatically improved patient safety, especially for patients with cardiovascular disease. He was chair of our Section on Cardiovascular Anesthesia from 1978 through 1983. John was a remarkable teacher. Many residents and students recall times he would sit on a patient cart outside of a cardiac operating room towards the end of a long day and spontaneously discuss any topic related to anesthesia (or his favorite hobby of fishing).
John left Mayo Clinic in 1983 to become chair of the Department of Anesthesia at the University of Iowa, a position he held until 1997. He subsequently moved to Omaha, Nebraska and chaired the University of Nebraska’s Department of Anesthesiology from 1997 through 2008. He passed away at age 74 in 2016.
Here is this week’s Mystery Photo.

Please email your response at warner.mark@mayo.edu within 3 days of this update. I will also need your name and contact information. All correct responses will be placed into a Monday morning drawing for a $10 Starbucks card. Only one winner per individual over the 80 weeks of Mystery Photos.

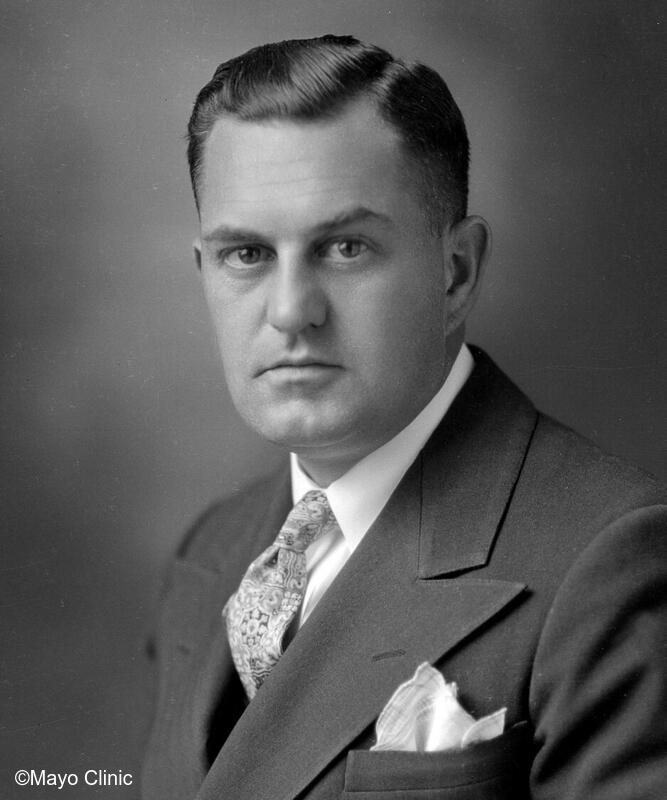
Photograph 1: Edward Tuohy, M.D., undated.
Photograph 2: John Silas Lundy, M.D., 1934.
Historic Inventions by Department Members
Members of our department during its first 100 years have made significant contributions to the specialty through innovation. While there are many I could select, let me start with just three important innovations associated with our department between 1926 and 1945. You may be surprised to learn of them and appreciate the positive impact they provide to modern perioperative care. Additional innovations will be highlighted in future Updates.
- John Lundy, Sodium Pentothal: Short-acting barbiturates became available in the 1920s and early 1930s. John Lundy was one of the first anesthesiologists who was motivated to learn if they would produce clinically useful anesthesia. He tried sodium amytal, sodium pentobarbital, and hexobarbital. Each one of them failed. For example, Lundy tested the use of pentobarbital (Nembutal) on his wife, Charlie Mayo, and even ex-heavyweight boxing champion Jack Dempsey and found that it was not appropriate to induce acceptable anesthesia. You can read more in the following paper by Asher Orkaby and Sukumar Desai titled “The Death of Sodium Pentothal: The Rise and Fall of an Anesthetic Turned Lethal”. It makes you wonder how they felt about its failure to induce suitable anesthesia, doesn’t it? In 1934 Abbott Laboratories provided him with vials of sodium pentothal (also known as sodium thiopental or thiopentone) to test. By early 1935 Lundy was convinced that sodium pentothal was safe and effective. He reported on his findings in the “1934 Annual Report of the Section of Anesthesia”. As with many innovations, there was early controversy as to origin. In this instance, the controversy was about who deserved credit for first using, introducing, and advocating for sodium pentothal’s use in anesthesia. Despite the early controversy, it is now generally accepted that Lundy’s clinical trial of the drug in patients was the first. His work was influential in introducing sodium pentothal to anesthesia and its use around the world.
- John Lundy, Citrated Blood, and Blood Banking: In 1933 Charlie Mayo asked John Lundy for the Section on Anesthesia to manage blood transfusion for children. By the next year, this was expanded to adult patients. In general, transfused blood at that time was fresh, with the need to have donors readily available. While citrate and glucose were first used in 1914 to preserve blood for transfusion and early preserved blood transfusions were made in World War I, there was not widespread use of citrated blood in the 1920s. When citrated blood was available, its preservation was measured in just a few days and not weeks. In 1935, Lundy found that citrated blood stored in an ice box could be safely and effectively used for up to two weeks. As described in “Mayo Clinic and the Origins of Blood Banking” by our own Jennifer Rabbits, Doug Bacon, and Greg Nuttall and Transfusion Medicine’s Breandan Moore here in Rochester, Lundy and colleagues such as Charles Adams and T. Harry Seldon established the country’s first blood bank.
- Ed Tuohy, Tuohy Epidural Needle and Continuous Spinal/Epidural Anesthesia: The use of regional anesthesia declined with the expanded use of sodium pentothal and ether, as well as other volatile drugs, prior to World War II. However, the use of general anesthesia in severely wounded, hemodynamically unstable soldiers, sailors, airmen, and Marines during the war, especially by individuals inexperienced in anesthesia, led to renewed interest in the use of regional anesthesia. Ed Tuohy trained at Mayo Clinic in the mid-1930s, was on staff in Rochester, and then was in the Army Medical Corps during the war. He understood the issues of both general and regional anesthesia and the opportunity that continuous spinal or epidural anesthesia might provide in the war setting. He used a previously designed needle with a curved end and a small ureteral catheter (a technique he learned with continuous spinal drainage at Mayo) to test continuous spinal and epidural anesthesia. There is a degree of controversy over the Tuohy needle’s name as described in this excellent article, “Edward Tuohy: The Man, His Needle, and Its Place in Obstetric Analgesia” by our own Josh Martini, Doug Bacon, and Gary Vasdev. Regardless, the Tuohy needle has become one of the most widely used epidural needles around the globe.
Mystery Photos
Last week’s Mystery Photo is Ron Mackenzie.

Ron was born in Detroit, Michigan and attended Alma College. After graduation from the University of Health Sciences Osteopathic School of Medicine 1967, he was a resident in anesthesiology at Detroit Osteopathic Hospital (2 years), Cleveland Clinic (1 year), and here in Rochester (1 year). He served many leadership roles in the department over his 43 years as a consultant, including chair of the former GYN/ENT (also known as the former South or current Jacobson) Division during Alan Sessler and Roy Cucchiara’s times as department chair. In addition he served as Vice-Chair of the department during Duane Rorie’s time as chair. Ron also led Mayo Clinic’s Equipment Committee for a number of years. He was an excellent teacher and was recognized multiple times by the residents as Teacher of the Year.
Ron was a wonderful advocate for young colleagues, nurse anesthetists, nurses, and just about all people in general. I don’t believe I ever met anyone who did not like Ron. Ron was a leader by example. He served as president of both the Minnesota Society of Anesthesiologists and the American Society of Anesthesiologists. Personally for Mary Ellen and me, Ron was a gracious friend and colleague throughout our careers. I started my first two weeks in anesthesia in July 1979 with him, one-on-one in old OR 16 at Methodist Hospital. He ended his career working day-by-day with Mary Ellen as they created and led the evolution of our creative new practices on Gonda 7. He worked clinically until age 77, stopping only to assist his beloved wife, Nancy, as they matured together.
Ron passed away far too early for us all on August 21, 2022. Here is a link to a farewell I wrote in the ASA’s newsletter.
Here is this week’s Mystery Photo.

Please email your response at warner.mark@mayo.edu within 3 days of this update. I will also need your name and contact information. All correct responses will be placed into a Monday morning drawing for a $10 Starbucks card. Only one winner per individual over the 80 weeks of Mystery Photos. If you win a weekly drawing, however, please keep submitting your responses. An overall winner (with the most correct responses in the series of 80 Updates) will receive a $100 Starbucks card.
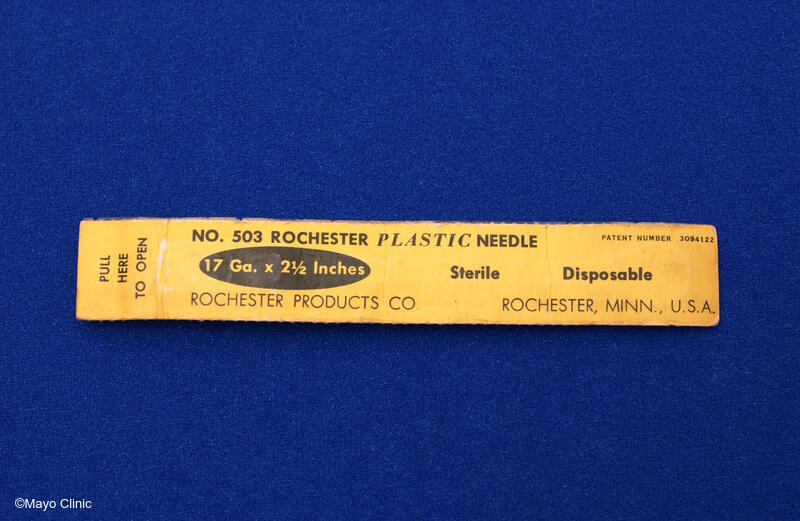
Our New Department Repository for History – Introducing “The History of the Mayo Clinic Department of Anesthesiology and Perioperative Medicine” webpage
After several months of preparation, we now have our “Phase 1” of the department’s new history webpage up and running. It comes as a webpage under the overall Mayo Clinic Heritage Website, which highlights the history of the Mayo Clinic as a whole. It is a great resource to access Mayo Clinic heritage films and other historical materials. If you have not yet seen any of Mayo Clinic’s heritage films, I strongly recommend watching the 2023 Heritage Film “Rising to the Challenge: The Mayo Aero Medical Unit in World War II”.
You will find that in the “Phase 1” release of our department webpage, there will be incomplete information in most of the sections. For example, more than 200 individuals influential in the development of the specialty, the institution, the department, or otherwise uniquely noteworthy will be described in some detail during the 18-months of the Centennial Project and its 80 weekly Updates. Much of this information and other materials are currently being compiled and the website will continue to be expanded. We will quickly be adding and modifying various sections and welcome your input and engagement in this celebration. The beautiful part of having a webpage for our history is that we can rapidly make corrections, adjustments, and additions. It is a “living document”.
The webpage will include, but is not limited to:
- The Centennial Weekly Updates.
- Newsletters from our nurse anesthetist alumni and our department newsletters during the 2000-2007 period.
- Department statistics for department, institution, and extramural society leadership.
- Additional stories and articles about our department.
- Photos from the past and present.
- Audio and video interviews from the past, with more being conducted in the future.
- A section specifically made to highlight our colleagues who have been in the military.
- Timelines, vignettes, etc.
- Digitalized books such as our 2000 “Art to Science” department history book.
- In the near future, sections specific for our Florida and Arizona sites as well as Respiratory Care.
More to come on the webpage. “Phase 2” of this webpage begins late this week. During the next few months, we’ll dramatically increase the information available on the webpage. Again, we’ll be seeking your suggestions, corrections, and ideas for improvement as we move forward over the next year.
Historic Inventions by Department Members, Part 2
Members of our department during its first 100 years have made significant contributions to the specialty through innovation. Continuing from last week’s description of the department’s involvement with the introduction of sodium pentothal into clinical practice, the development of the first U.S. blood bank, and the first use of the Tuohy needle for continuous spinal and epidural anesthesia, here is an important innovation associated with our department in the 1950s. Additional innovations will be highlighted in future Updates.
- David Massa, Intravascular Catheter (IV catheter): It seems so straightforward now, but prior to the 1950s giving intravenous fluid was problematic. Needles allowed vascular access but could become dislodged easily and couldn’t not be used for long periods without immobilizing extremities. Veins could be cannulated with cutdown techniques, but the tubing needed was not readily available, at least until the middle 1940s. It took a Mayo anesthesiology fellow, David Massa, in 1950 to develop the precursor of today’s intravenous angiocath. You can read more about this in this article “A Plastic Needle” and from this portion of the “Proceedings of the Staff Meetings of the Mayo Clinic” from 1950. He started by designing and testing prototypes in his basement and sterilizing the cannulas in his kitchen “The Massa or Rochester Plastic Needle”. As described by our own Peter Southorn and Brad Narr, the “catheter over a needle” concept was soon produced by the Rochester Products Company. Sales grew slowly at first but by the mid-1960s, more than 3 million of these needles had been produced. This innovation made a dramatic change in surgery and medicine and is noted by Atul Gawande, one of the country’s most preeminent surgeons, as an “ingenious creation” and one of medicine’s most consequential in his history of the first 200 years of surgery “Two Hundred Years of Surgery”.
Mystery Photos
Last week’s Mystery Photo is T. Harry Seldon, M.D.

Dr. Seldon was born on January 16, 1905, in Exeter, Ontario, Canada. He received the M.D.C.M degree in 1929 from Queen's University in Ontario. After completing an internship at Toronto Western Hospital (1929-1930), he was in private practice in Sharlot Lake, Ontario (1930-1936). He entered the Mayo School of Graduate Medical Education in 1936 as a fellow in anesthesiology and received the M.S. degree in anesthesiology from the University of Minnesota in 1940. That same year, Dr. Seldon was appointed a Mayo Clinic consultant. In addition to an interest in general anesthesia, he was very involved in the department’s growing work in orthopedic and plastic surgery. He also led the institution’s blood transfusion service.
Dr. Seldon was very involved in the evolution of the science and specialty of anesthesiology. He was president of the American Association of Blood Banks and the Minnesota Society of Anesthesiologists. He was especially active in the International Anesthesia Research Society (IARS).
- Member of the Board of Trustees, 1948-1976.
- Chair of the Board, 1955-1957
- Editor (in-chief) of the IARS’s Current Researches in Anesthesia and Analgesia (which became Anesthesia and Analgesia . . . Current Researches in 1957 and then Anesthesia and Analgesia in 1979), 1955-1976.
- Harry documented the early history of the IARS in 1971 on the 50th anniversary of Anesthesia and Analgesia.
- Recognized in 1983 by the IARS Board of Trustees when it established the T. H. Seldon Memorial Lecture in his honor.
- This keynote lecture opens the IARS Annual Meeting and brings renowned experts to spark important conversations on anesthesiology and beyond.
Dr. Seldon retired from Mayo Clinic in March 1970 and died in Rochester’s Charter House on October 22, 1991.
Here is this week’s Mystery Photo.

Please email your response at warner.mark@mayo.edu within 3 days of this update. I will also need your name and contact information. All correct responses will be placed into a Monday morning drawing for a $10 Starbucks card. Only one winner per individual over the 80 weeks of Mystery Photos. If you win a weekly drawing, however, please keep submitting your responses. An overall winner (with the most correct responses in the series of 80 Updates) will receive a $100 Starbucks card.


Photograph 1: John Silas Lundy, M.D., 1950.
Photograph 2: Jerry Dorsch, M.D., 1988.
Books, Books, and More Books
The Mayo Clinic Department of Anesthesiology was a major contributor to the education of nurse anesthetists and anesthesiologists through publication of scientific articles and textbooks. There have been many important texts from Mayo anesthesiologists. For today’s Update, I will address two of the classic textbooks written by our colleagues. These are John Lundy’s Clinical Anesthesia and Jerry and Susan Dorsch’s Understanding Anesthesia Equipment.
- John Lundy, Clinical Anesthesia: As John Lundy gained national visibility in the specialty during the 1924-1941 time period from his significant work in advancing regional anesthesia, advocating for balanced anesthesia, doing the initial clinical studies on sodium pentothal, starting an anatomy laboratory specifically for teaching regional anesthesia, developing the first blood bank in the U.S., and helping to found the American Board of Anesthesiology and the journal Anesthesiology, he also found time to write one of the country’s first comprehensive and most widely-read textbooks on anesthesiology. Clinical Anesthesia was used by a generation of physicians and nurse anesthetists as the fledgling specialty was evolving into a scientific field of study and educational programs. Many of the physicians who trained in 90-day anesthesia courses during WWII and subsequently played major roles in improving combat-related fatalities across the European and Pacific theaters of war used Lundy’s text as their primary source of basic anesthesia knowledge.
- Jerry and Susan Dorsch, Understanding Anesthesia Equipment: In 1969 while both were residents in anesthesiology in Pittsburgh, Jerry and Susan Dorsch set out to write what in 1975 would become one of the most world’s widely-read textbooks on anesthesia equipment. Since its first review and through reviews of its 5th edition in 2008, it has been repeatedly described as “the bible on anesthesia equipment.” Jerry and Susan wrote 5 additional textbooks, including their 2010 A Practical Approach to Anesthesia Equipment. This text is a simplified version of their much larger text and received outstanding reviews in Anesthesiology titled “Reviews of Educational Material A Practical Approach to Anesthesia Equipment” and in Anesthesia & Analgesia titled “A Practical Approach to Anesthesia Equipment Review”.
- Jerry was a member of our Mayo Clinic Department of Anesthesiology in Jacksonville from 1987 through 2003. Susan was in private practice. Here is an outstanding report on their careers, a wonderful photo of Jerry and Susan, and a note about their 2008 Wood Library-Museum Wright Lecture titled “Beyond Blue Lips: Advances in the Prevention of Hypoxia”.
Mystery Photos
Last week’s Mystery Photo is Sheila M. Muldoon, M.D.

Dr. Muldoon was born on July 6, 1935, in Kells, Ireland. She graduated medical school at the University College in Dublin in 1963. After initial postgraduate training at Mater Hospital in Dublin, she moved to Rochester and started her anesthesiology residency in 1966. During her training, she earned an M.S. degree in anesthesiology and physiology from the University of Minnesota while advised by Dr. Richard They. She was a staff member of our department from 1969 through 1977. While in Rochester, she worked clinically in our growing Respiratory Care Service. She received multiple research grants, including from the NIH, and worked closely with former department chair Dr. Duane Rorie and researchers Drs. Gertrude Tyce and Paul Vanhoutte.
In 1977 Sheila moved to the Washington, D.C. area and was one of the very first women appointed to the new Uniformed Services University for Health Sciences (USUHS) faculty. During her time at USUHS she identified growing military concerns about exertional heat illnesses, including the potential of unrecognized malignant hyperthermia (MH) in military personnel. She established what was to become one of the country’s leading MH testing and research laboratories, now designated as the “Sheila Muldoon Malignant Hyperthermia Diagnostic Center.” The center was one of a handful of muscle testing centers in the U.S. and provided testing services similar to those in our Mayo Rochester laboratory that was led by Drs. Jerry Gronert, Denise Wedel and Margaret Weglinski. Dr. Muldoon was very active in the evolution of Malignant Hyperthermia Association of the U.S. (MHAUS) and its MH Hotline. A wonderful summary of her contributions to MH research and MHAUS, written by MHAUS President Henry Rosenberg, M.D. can be found here.
Dr. Muldoon became chair of the USUHS Department of Anesthesiology in 1987, a position she held until 2001. An excellent summary of her contributions to the USUHS is found in this article about the institution’s early women pioneers.
Last week’s contest winner was Kai Rehder.
Here is this week’s Mystery Photo.

Please email your response at warner.mark@mayo.edu within 3 days of this update. I will also need your name and contact information. All correct responses will be placed into a Monday morning drawing for a $10 Starbucks card. Only one winner per individual over the 80 weeks of Mystery Photos. If you win a weekly drawing, however, please keep submitting your responses. An overall winner (with the most correct responses in the series of 80 Updates) will receive a $100 Starbucks card.

Gaston Labat, M.D., undated.
Our Department of Anesthesiology Innovations: Gaston Labat and the Rise of Regional Anesthesia at the Mayo Clinic and Across the U.S.
Mayo Clinic was thriving in 1920 as the world rebounded from the impact of World War I. The Mayo brothers and their colleagues, including our nurse anesthetists, continued to produce excellent surgical outcomes. Their contributions of Mayo Clinic personnel, and their personal involvement, in the war had increased the Mayo reputation in the U.S., Europe, and elsewhere around the world. However, Will and Charlie were never satisfied with the status quo; they wished for patient care to improve as medical practices evolved. To this end, they personally traveled across the U.S. and abroad to learn new surgical and diagnostic techniques and treatments. They also encouraged their colleagues to travel.
While visiting Victor Pauchet, a well-known professor of surgery in Paris in 1920, Charlie observed the anesthesia performed by Gaston Labat. He was particularly impressed with Labat’s use of regional blocks and recognized the potential of regional anesthesia to improve muscle relaxation and operating conditions, especially for intra-abdominal and intra-pelvic procedures. Labat had worked for three years as a medical student at the University of Paris with Pauchet. Pauchet was a strong advocate for the use of regional anesthesia. In 1914, Pauchet had published the first edition of L’Anesthesie Regionale. A revised second edition followed in 1917. Charlie promptly invited Labat to Rochester to teach the Mayo surgeons how to administer regional anesthesia.
Our own Doug Bacon provides an excellent summary (“Gaston Labat, John Lundy, Emery Rovenstine, and the Mayo Clinic: The spread of Regional Anesthesia in America Between the World Wars”) of Labat’s time in Rochester from September 1920 through October 1921 and the long-term positive impact of his Mayo connection on the growth of regional anesthesia in the U.S. During his stay, Labat produced his classic text, Regional Anesthesia: Its Technic and Clinical Application. It was published in 1922 after Labat had moved to New York City and was working at New York University and Bellevue Hospitals. His advocacy and the textbook led to the increase in enthusiasm for and use of regional anesthesia in the U.S. and elsewhere. His text was revised into a 2nd edition in 1928. Labat became a strong advocate for regional anesthesia and was a founding member of the original American Society of Regional Anesthesia.
Labat’s regional anesthesia textbook created controversy of its own as it was very similar to the earlier Pauchet text. Our own Annie Côté, Claude Vachon, Terre Horlocker, and Doug Bacon describe this controversy, with Labat never crediting Pauchet in their 2003 article titled “From Victor Pauchet to Gaston Labat: The Transformation of Regional Anesthesia from a Surgeon’s Practice to the Physician Anesthesiologist”. Mystery arises with Labat’s death in 1934 and the apparent “loss” of a third edition of the text, described by our own Claude Vachon, Doug Bacon, and Steve Rose in their 2008 article titled “Gaston Labat’s Regional Anesthesia: The Missing Years”.
Simply put, Labat was the primary catalyst for the rise of regional anesthesia in the U.S. His advocacy and textbook led to several generations of anesthesia leaders (e.g., Lundy, Ralph Waters, and Emory Rovenstine) who carried the enthusiasm for the use of regional anesthesia forward and across the country.
Mystery Photos
Last week’s Mystery Photo is Florence McQuillan, CRNA.

As described by the AANA (Profiles of Nurse Anesthetists/Nurse Anesthesiologists - AANA - American Association of Nurse Anesthesiology), she was born in 1903 in Mahtowa, Minnesota (25 miles SW of Duluth) and graduated from the Central School of Nursing at the University of Minnesota in 1925. She received her anesthesia education at the Minneapolis General Hospital in 1926. John Lundy invited Florence to join his staff at the Mayo Clinic in 1927. She worked closely with Lundy as chief nurse anesthetist, cared for the patients of the Mayo brothers, and served as a clinical instructor for new nurse anesthetists.
In 1936, Lundy asked Florence and Dr. Lloyd Mousel, a new resident, to select papers for presentation at a staff, resident, and nurse anesthetist journal club. Attendees were initially asked to review the papers and prepare reports for the journal club, an additional task that they resented. Within a year, Florence suggested to Lundy that an abstract for each paper be prepared by either her or our Mayo Section on Publications to reduce the burden on the attendees. This proved popular and in 1937 Lundy and Florence began publishing these abstracts in a new format, Anesthesia Abstracts. The journal Anesthesia Abstracts was produced from 1937 through 1966 and was widely read. It’s successor publication, Survey in Anesthesiology, was published through 2017. Florence also prepared abstracts for the fledgling Anesthesiology from 1940 through 1947.
In 1948 Florence resigned from Mayo Clinic and became the first AANA Executive Director (formerly Executive Secretary), a position she held until her retirement in 1970. In her 22 years as Executive Director, she was influential in virtually all areas of the AANA’s growth and expansion. Under her guidance, the US Department of Health, Education, and Welfare officially recognized the AANA’s authority to grant accreditation for nurse anesthesia programs and to grant certification for nurse anesthetists/nurse anesthesiologists. She also instituted the AANA’s voluntary continuing education program, which made the AANA the first professional nursing organization to recognize the need for continuing professional education; this eventually led to the adoption of a mandatory CE program. Florence received the AANA Award of Appreciation in 1970 and the Agatha Hodgins Award of Outstanding Accomplishment in 1981.
An excellent summary of her career can be found at Florence McQuillen (1903–1981), “Benevolent Dictator” of Nurse Anesthetists - Working Nurse.
Last week’s contest winner was Kelsey Nelsen.
Here is this week’s Mystery Photo.
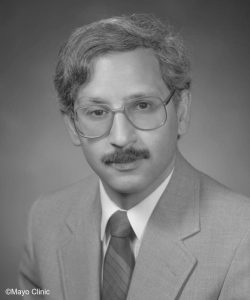
Please email your response at warner.mark@mayo.edu within 3 days of this update. I will also need your name and contact information. All correct responses will be placed into a Monday morning drawing for a $10 Starbucks card. Only one winner per individual over the 80 weeks of Mystery Photos. If you win a weekly drawing, however, please keep submitting your responses. An overall winner (with the most correct responses in the series of 80 Updates) will receive a $100 Starbucks card.



Photograph 1: Harriet Cronk, Noreen Robins, Dr. Lundy, Dr. Albert Faulconer, Jr., and Helene Romness checking supplies at Saint Marys Hospital before the Clinic Blood Bank moved to Mayo Clinic from Saint Marys Hospital, 1951.
Photograph 2: Daryl Kor, M.D., undated.
Photograph 3: Matthew Warner, M.D., undated.
Department of Anesthesiology Innovations: Preoperative Transfusion Triggers for Low Hemoglobin
Drs. John Lundy and Charles Adams, the first two chairs of our department in 1924-1952 and 1952-1953, respectively, worked closely throughout their careers. Both had a strong interest in improving patient care and safety. Adams joined the department as a fellow in 1935, the same year that Lundy established the country’s first hospital blood bank and used refrigerated, citrated blood. One of their common interests was preoperative anemia and its potential impact on the outcomes of surgical patients. Based on their clinical observations, they published a 1942 article in the Journal of Surgery, Gynecology, and Obstetrics (now known as the Journal of the American College of Surgeons) and highlighted the importance of transfusing blood when the preoperative hemoglobin was less than 8 to 10 grams per cubic centimeter of whole blood. Lundy also advocated for preoperative transfusions for anemia in his classic 1942 textbook, Clinical Anesthesia: A Manual of Clinical Anesthesiology (pages 380-381).
As with many new ideas, there was controversy around the issue of transfusion triggers. For example, Myhre noted in his work, “Clinical Commentary: The Transfusion Trigger-the Search for a Quantitative Holy Grail”, that Lundy and Adams presented no data upon which to base their recommendation. Nonetheless, their strong advocacy and, especially, Mayo Clinic and Lundy’s national visibility and credibility led to the general spread of using transfusion triggers in preoperative assessment of surgical patients. Lundy was particularly influential as his textbook became the official source for information used in the 90-day anesthesia training programs for physicians in WWII. Many of these physicians would become leaders of the specialty during the decades that followed the war.
Interestingly, our department continues to lead the country in evaluating and treating preoperative anemia. Drs. DJ Kor and Matt Warner currently oversee a large clinical research effort that includes many of our colleagues to evaluate and implement perioperative patient blood management strategies. Examples from their work have been published extensively this past year in journals such as JAMA, Annuals of Surgery, Anesthesia and Analgesia, and the Journal of Clinical Anesthesia.
Mystery Photos
Last week’s Mystery Photo is Bob Chantigian, M.D.
Bob was born in Philadelphia in 1951 and attended Temple University. Not content to be a typical college student, he was engaged in the university for a decade and graduated with not one but three degrees (B.A. in Mathematics, B.S. in Pharmacy, and M.D.). He came to Mayo in Rochester for his residency training in 1979, joining an incoming group of new residents that included Steve Rettke, Mary Ellen Warner, and Mark Warner. Amazingly, these four individuals have spent a cumulative 165 years in the department. By the time you read this Update, Bob will have retired as his last work day as a consultant is Wednesday, February 14th, a Valentine’s Day that many of us will associate with Bob’s retirement date.
After completing his residency program, Bob trained in obstetric anesthesia at Brigham and Women’s Hospital in Boston and then in pediatric anesthesia at Children’s National Medical Center in Washington, D.C. He joined the staff of Brigham and Women’s Department of Anesthesiology from 1983 through mid-1985 before returning to Rochester. Upon his return he became the department’s Director of Obstetric Anesthesia, serving in that capacity for 10 years and remaining a mainstay in that area for two decades.
Bob is a remarkable teacher and clinician. He has been awarded 10 Teacher of the Year Awards from the residents and student nurse anesthetists and is a member of the Mayo Fellows Association Teaching Hall of Fame. In 2013, the department recognized him with its Commitment to Education Award. He also earned Distinguished Clinician Awards from residents and colleagues.
In 1992 Brian Hall and Tony Jones wrote the first edition of their best-selling board examination preparation book, Anesthesia: A Comprehensive Review. They published a 2nd edition in 1997 before Tony left Mayo to become chair of the Department of Anesthesiology at the University of Alabama at Birmingham. With Tony’s move, Bob joined Brian in producing editions 3 through 6 in 2003, 2010, 2015, and 2019, respectively. Their text is one of the best-selling in the U.S. over three decades and has become an anesthesia library staple. They currently are working on the book’s 7th revision. They believe it will be available at the end of this year.
Last week’s contest winner was Monica Green.
Here is this week’s Mystery Photo.

Please email your response at warner.mark@mayo.edu within 3 days of this update. I will also need your name and contact information. All correct responses will be placed into a Monday morning drawing for a $10 Starbucks card. Only one winner per individual over the 80 weeks of Mystery Photos. If you win a weekly drawing, however, please keep submitting your responses. An overall winner (with the most correct responses in the series of 80 Updates) will receive a $100 Starbucks card.

Steven Rettkee, M.D., undated.
Department of Anesthesiology Colleagues Who Have Served in the Military
For much of the Department of Anesthesiology’s first 100 years, our colleagues have contributed to the U.S. armed forces military readiness and responses. Steve Rettke, a distinguished U.S. Navy carrier fighter pilot and retired Navy captain, as well as long-time leader of our Methodist Hospital clinical practices, is creating a webpage on our history website that will be part of our overall department’s history repository webpage.
You will find Phase 1 of the military webpage development here on the webpage in the Mayo Clinic Military Anesthesia Statistics section. In the coming months, we hope to have a more comprehensive compilation of our military colleagues and their accomplishments. If you (alumni or department members past or present) have served at any point in the U.S. Armed Forces, Steve is asking for you to send the following information to both him (Rettke.steven@mayo.edu) and Alec Thicke (Thicke.alec@mayo.edu). Alec is our department’s archivist. They will create a database and add this information and your stories to the webpages.
If you are interested in learning more about Mayo Clinic and its role with the military over the years, there are two interesting films produced by the institution that you might find fascinating. You may find them on the Mayo Clinic History & Heritage website.
- Rising to the Challenge: Mayo Clinic and the Military. This film documents the remarkable Mayo Clinic project during World War II that led to the development of the G-suit and oxygen masks for our pilots, innovations that contributed to aerial warfare advantages and played major roles in the ultimate success of the U.S. in the war.
- Serving with Honor: Mayo Clinic and the Military. This film describes Mayo Clinic’s major contributions to our country’s military efforts during the past century. Our institution has been a leader in supporting our military and our colleagues who participated in these efforts.
Mystery Photos
Last week’s Mystery Photo is Leslie N. Milde, M.D.

Leslie was born in Rochester, NY and attended the University of Rochester. She served as the chief pulmonary function and senior clinical research technician in the Cardiovascular Research Institute of the University of California, San Francisco (UCSF) for five years before entering the UCSF School of Medicine in 1973. She completed her anesthesiology residency and critical care fellowship in 1981 at Massachusetts General Hospital, serving as an editor of the widely read MGH Handbook on Clinical Procedures of the MGH while in training. She subsequently moved to Rochester as a neuroanesthesia research fellow with Jack Michenfelder. She joined our staff in 1982 and rapidly rose to the rank of Professor of Anesthesiology in 1993, becoming our department’s first woman to attain that high rank.
Leslie was a champion of anesthesia education, receiving Teacher of the Year awards and serving as the anesthesiology residency’s program director. She served 16 years as an oral examiner for the American Board of Anesthesiology. She was very involved in leading the development of neuroanesthesiology, serving as treasurer of the Society for Neuroscience in Anesthesiology and Critical Care and a long-time editor of the Journal of Neurosurgical Anesthesiology. She also was chair of the American Society of Anesthesiology’s Committee on Experimental Neurosciences and a member of its Subcommittee on Neuromuscular Transmission.
Leslie moved to Arizona in 1994 and served as chair of our Mayo Clinic Arizona (MCA) Department of Anesthesiology from 1997 through 2003. While in Arizona, she made major contributions to the evolution of MCA as a member of the MCA Board of Governors and its Executive Committee and the MCA Executive Operations Team, serving as the Executive Operations Team for six years. In that role she led an Academic Development course for women physicians and an administrative course for administrative interns. She was the leader of Public Relations for MCA during that time period. She subsequently sat on the Board of Governors for the institution and was part of the group to redefine its administrative structure. She chaired a task force to integrate the three existing geographically-define Mayo Clinic internet entities into the one institutional internet site we have today. While on the Mayo Clinic Board of Governors, she simultaneously was a physician member of the Board of Trustees. An endowed travel grant for an anesthesiology resident research winner in MCA has been named in her honor. Although retired in 2010, she continued to provide anesthesia care through 2017 as a supplemental consultant.
Last week’s contest winner was Karen Hammell.
Here is this week’s Mystery Photo.

Please email your response at warner.mark@mayo.edu within 3 days of this update. I will also need your name and contact information. All correct responses will be placed into a Monday morning drawing for a $10 Starbucks card. Only one winner per individual over the 80 weeks of Mystery Photos. If you win a weekly drawing, however, please keep submitting your responses. An overall winner (with the most correct responses in the series of 80 Updates) will receive a $100 Starbucks card.

Gerald "Gerry" Gronert, M.D., undated
Our Department of Anesthesiology and Its Role in Elucidating Succinylcholine-Induced Hyperkalemia and also Mechanisms of Malignant Hyperthermia
Members of our Rochester-based Neuroanesthesiology Division have made significant contributions over the years to our understanding of a variety of diverse clinical conditions, including brain protection strategies and mechanisms; perioperative air embolism and its prevention and treatment; cerebral blood flow; and many others. These will be addressed in future Updates. Today, we will focus on the work of Dr. Gerald (Gerry) Gronert. His findings related primarily but not exclusively to succinylcholine-induced hyperkalemia and mechanisms of malignant hyperthermia. They have dramatically impacted our clinical practices and improved patient safety worldwide.
Gerry wrote about his work in our department and also during a short stint in the Air Force in a summary that Peter Southorn placed in our department’s September 2006 Newsletter "Mayo ala Gerald A. Gronert". He was interviewed for his work on succinylcholine-induced hyperkalemia in 2009 by David S. Warner (no relation to me and a different person than our own David O. Warner). In the interview, Gerry provided additional insights into his research on this issue. His early work was shared with Dr. Dick Theye and related to patients with extensive burns. They then expanded this work to include models of denervated muscle and muscle disuse atrophy.
Along the way, Gerry became interested in malignant hyperthermia (MH). He worked extensively with MH-susceptible pigs and published the specialty’s most significant paper to date on MH in 1980 in Anesthesiology. He was very involved in the early evolution of the Malignant Hyperthermia Association of the United States (MHAUS) Hot Line, as were Drs. Denise Wedel and Margaret Weglinski subsequently.
Gerry left Mayo Clinic in 1986, moving for the University of California, Davis. He worked at that institution until retiring in 1999. He passed away on February 7, 2020 in Eugene, Oregon (Gerald Gronert Obituary (1933 - 2020) - Sacramento, CA - The Sacramento Bee (legacy.com).
Mystery Photos
Last week’s Mystery Photo is Curt Buck, R.R.T., CRNA.

Curt was born in Winona, MN but graduated high school at John Marshall in Rochester. He began his Mayo Clinic career at St. Marys Hospital in its front lobby as a “bellboy” (honest, that was the job title) in 1971. After high school, he completed a 2-year nursing degree at Rochester Junior College (currently the Rochester Community and Technical College). Curt worked in the existing 3rd Alfred Surgical ICU at St Marys Hospital for two years, then joined our nascent Mayo Respiratory Therapy program’s second class. He worked as a respiratory therapist at St. Marys Hospital until 1979 before matriculating into our Mayo Clinic Nurse Anesthesia program. He completed his anesthesia training in 1981.
Curt spent most of his 11 years in our operating rooms in the old General Section (currently the Multispecialty Division) at St. Marys Hospital. Contemporaries in the General Section at the time included nurse anesthetists John Ahle, Christine Hendricks, Mary Marienau, Don Nelson, John Carter, Dan Schnell, Gloria Davis, Jack Hostak, Jan Miller, Margaret Sinclair, Bev Ondler, Pauline Bisel, Linda Buck, and many others. In 1992, Bernie Gillis, our director of Respiratory Therapy and a great nurse anesthetist, was severely injured in a car accident. Given Curt’s background as an RT, he was asked to temporarily fill in as director of Respiratory Therapy. As with many “temporary” Mayo appointments, this one turned out to be permanent. Curt held the position for 22 years. During those 22 years he worked with colleague intensivists such as Drs. Brad Narr, Mike Murray, Dan Brown, Rolf Hubmayr, Dan Diedrich, and many others.
Our Rochester Respiratory Therapy Division excelled under Curt’s vision and leadership. Curt and Dr. David Warner expanded our department’s small Perioperative Outcomes Group and created our robust Anesthesia Clinical Research Unit (now part of our Perioperative Information Management, Implementation, and Analytics Program, PRIISM). Brad Narr and Curt worked together to integrate our respiratory therapists into our new Preoperative Evaluation Clinic. Under Curt’s leadership, our respiratory therapists advanced the practice of respiratory care by first implementing therapist-driven ventilation protocols and then independent management of ventilation for many patients. Our Respiratory Care Division is now considered one of the most active and progressive in the country, with full credit to Curt and his respiratory therapy colleagues for their remarkably successful and innovative clinical initiatives and growth.
Last week’s contest winner was Lori Hanson.
Here is this week’s Mystery Photo.
Please email your response at warner.mark@mayo.edu within 3 days of this update. I will also need your name and contact information. All correct responses will be placed into a Monday morning drawing for a $10 Starbucks card. Only one winner per individual over the 80 weeks of Mystery Photos. If you win a weekly drawing, however, please keep submitting your responses. An overall winner (with the most correct responses in the series of 80 Updates) will receive a $100 Starbucks card.

Photograph: Ron J. Frost, M.D., undated.
Remarkable Educators: This Week’s Feature on Dr. Ron Faust
The department, institution-wide, has been blessed with outstanding educators and leaders during its first 100 years. In the coming months, we’ll highlight a number of those leaders. These will include anesthesiologists who have led national and internal graduate medical education schools and initiatives (e.g., Alan Sessler, Mark Warner, and Steve Rose in their roles as Dean, Mayo Clinic School of Graduate Medical Education); nurse anesthetists who have been legendary leaders in education, program directors, and the nurse anesthesia program’s medical directors (e.g., Alice Magaw, Florence McQuillen, Ed Thompson, Bob Johnson, Mary Marienau, Erin Martin; Virginia Hartridge, and Beth Elliott); and anesthesiology residency program directors (e.g., Alan Sessler, Ron Faust, Leslie Milde, Steve Rose, Tim Long, Renee Caswell, Marie DeRuyter, and others).
This week we are featuring Dr. Ron Faust. For those who were residents in my generation, Ron was an outstanding program director and wonderful colleague. Ron was the son of a New Orleans anesthesiologist. He attended the Louisiana State University Medical School, graduating in 1969. What was to follow for the next four years is best described by Ron:
“I signed up with the Navy while a student at LSU Medical School in New Orleans in the class of 1969. My father, a physician, had signed up with the Navy the day after Pearl Harbor was attacked. An older brother of mine, an attorney in the Navy, was on a carrier in the late ’60’s.
Active duty for me started July 1970 at the end of my rotating internship at Charity Hospital. When my orders came, I was very surprised to read that I would be going to the 1st Marine Division; they were in Vietnam. The Navy Medical Corps provided all medical support to the Marine Corps. By July 26, 1970, I was on the ground as a ”Battalion Surgeon” in the 1st Marine Division in what was to later become South Vietnam. The area was still a combat zone and my Battalion Aid Station consisted of two small rooms under sandbags near the village of An Hoa. This was a rural base about 30 miles south of Da Nang. When a big Battalion operation was in progress, I would rotate out to camp on a hilltop called “371” in support of the Battalion Command. My tour of duty in that country ended in late March 1971.
For my second year of active duty, I served at Oakland Naval Hospital as a general medical officer in their out-patient “drop in” clinic. We saw Navy personnel and their family members. I completed my second year of active duty there in June 1972.
Advancing into inactive Naval Reserve, I returned to Charity Hospital in New Orleans that summer. I started first-year residency in general surgery on the LSU service. A year later I ‘saw the light’ and transferred to anesthesia residency at Mayo in July 1973.”
Ron worked clinically primarily in our Division of Neuroanesthesiology with colleagues such as Jack Michenfelder, Joe Messick, Roy Cucchiara, Leslie Milde, Bill Lanier, Don Muzzi, Tom Lasasso, Margaret Weglinski, Bill Perkins, and others. He dedicated much of his attention to our residency program. During his time as program director, 248 residents and fellows trained in our programs and the annual number of residents grew from 26 to 62. Ron was a national leader in anesthesiology education and served as president of the Society for Education in Anesthesia in 1991-1992. His book, Anesthesiology Review, is one of the specialty’s most successful and widely read texts. It was initially published in 1991; the 6th edition is now entitled, Faust’s Anesthesiology Review, with Editor-In-Chief Dr. Terry Trentman, former chair of our department in Mayo Clinic Arizona. More than 100 department members have contributed chapters to the series of the book’s editions.
In recognition of his outstanding contributions to education at Mayo Clinic, Ron was recognized with Mayo Clinic’s Distinguished Educator Award in 2000. Others in the department who have earned that recognition are:
- 2000: Ron Faust
- 2009: Beth Elliott
- 2015: Renee Caswell
- 2017: Mark Warner
- 2022: Beth Ladlie
- 2022: Steve Rose
Ron has a passion for cars. He wrote an article describing this passion for Peter Southorn in our May 2026 department newsletter titled “My Automotive Avocation May 2006”. Ron and his wife, Claire, have two daughters and a son. His son, Jonathan, is an anesthesiologist alumni of our department and currently practices in the Twin Cities area.
Mystery Photos
Last week’s Mystery Photo is Gary Sieck, Ph.D.
Gary was born in Seward, Nebraska, and together with his twin brother Jerry, they were the first in the family to attend college. Gary is a University of Nebraska Corn Husker through and through, earning his undergraduate degree in Lincoln and PhD in Physiology & Biophysics in Omaha. After a postdoctoral fellowship at the UCLA Brain Research Institute, Gary was appointed to the faculty in the Department of Anatomy & Cell Biology at UCLA and the Department of Pulmonary Medicine at City of Hope Medical Center. In 1987, Gary transitioned to the faculty in Biomedical Engineering at the University of Southern California.
He finally saw the light and returned to the Midwest, coming to Rochester in 1990 and joining our department as well as the Mayo Clinic’s Department of Physiology & Biomedical Engineering. From 1991-2002, Gary served as our Vice-Chair for Research. In 2002, he became Chair of the Department of Physiology & Biomedical Engineering, serving in that role until 2014.
Gary’s research focuses on cardiopulmonary physiology with an emphasis on neural control of breathing muscles. His research has been continuously funded by NIH grants since 1976. He has published extensively. Throughout his career, Gary has been incredibly active in education and mentorship. He has mentored more than 350 students and fellows. Many of his trainees have gone on to successful careers in biomedical research. In fact, two of his former PhD trainees are currently department chairs in our institution, Y.S. Prakash in Physiology & Biomedical Engineering and Carlos Mantilla in, of course, Anesthesiology & Perioperative Medicine.
Gary has received numerous honors for his research accomplishments, including recognition as a named professor and a Distinguished Mayo Investigator. Outside of Mayo, he has received the Rodarte Award for Scientific Distinction from the American Thoracic Society (ATS), the Distinguished Service Award from the Association of Chairs of Departments of Physiology (ACDP), the Distinguished Alumnus Award from the University of Nebraska Medical Center, and the Distinguished Advocate Award from the American Institute of Medical and Biological Engineering (AIMBE).
He has served as a member of the ATS Board of Directors, a member of the National Council of the American Lung Association, President of the American Physiological Society (APS) and President of the Association of Chairs of Departments of Physiology. He is currently a member of the Executive Committee of the International Union of Physiological Sciences (IUPS). In his spare time (ha!), Gary has served as Editor-in-Chief of both the Journal of Applied Physiology and of Physiology.
Here is this week’s Mystery Photo.

Please email your response at warner.mark@mayo.edu within 3 days of this update. I will also need your name and contact information. All correct responses will be placed into a Monday morning drawing for a $10 Starbucks card. Only one winner per individual over the 80 weeks of Mystery Photos. If you win a weekly drawing, however, please keep submitting your responses. An overall winner (with the most correct responses in the series of 80 Updates) will receive a $100 Starbucks card.
Photograph: Alan D. Sessler, M.D., undated
The Department of Anesthesiology and the Creation and Evolution of the Foundation for Anesthesia Education and Research (FAER)
While the professional societies of the ASA and AANA have played major roles in advances in the specialty, a big boost to these advances came in 1984 when the ASA established and funded unique foundations to promote new knowledge in anesthesiology and patient safety. These two new foundations became known as the Foundation for Anesthesia Education and Research (FAER; Foundation for Anesthesia Education and Research (FAER) (asahq.org) and the Anesthesia Patient Safety Foundation (APSF; Anesthesia Patient Safety Foundation - That no one shall be harmed by anesthesia care. (apsf.org), respectively. The ASA has not wavered in its commitment to these foundations, supporting them with more than $80 million in today’s dollars in funding over the past 4 decades.
Many of the specialty’s finest researchers, including many in our department, have benefitted from FAER and APSF grants early in their careers. The dollars have been well spent. The early career investigators who received these grants have produced far more than their value in federal research funds and led to new knowledge that has resulted in advances such as the understanding of basic physiologic responses in disease processes, development of anesthesia simulation, improvements in perioperative blood management, reduction of postoperative hypothermia, diminished risk of postoperative neuropathies and vision loss, and other major safety improvements.
In a 2007 article from our department newsletter FAER and Mayo Anesthesiology, Peter Southorn and Alan Sessler describe the early development and evolution of FAER. Alan played major roles in establishing FAER and leading the foundation to one of the major contributors to the development of early career scientists in anesthesiology.
Mystery Photos
Last week’s Mystery Photo is Dr. Sait Tarhan.

Sait was born in Crimea in 1927 and at age 4 years he and his family immigrated to Turkey and settled in Izmir. He graduated from the Istanbul Medical School and trained in pulmonary medicine. After completing his training, he served in the Turkish Army on the country’s eastern front. After completing two years of service, he moved to the U.S. in 1958 and worked as a pulmonologist in the Cincinnati, Ohio area for 4 years. He then moved to Rochester, trained in our department, and joined the staff in 1965. He spent most of his career working in our cardiac anesthesiology section and also served as our St. Marys Hospital Division chair from 1975-1983.
Sait became one of the world leaders in cardiac anesthesia. Joining forces with Drs. Emerson Moffit, he published a seminal paper on myocardial infarction after general anesthesia. This JAMA paper led to an understanding of the impact of patient risk on perioperative outcomes and in decisions about scheduling patients for elective surgery. For more than 3 decades, this paper and a subsequent confirmatory paper by Petter Steen and Sait guided the world on surgical decision-making and perioperative management of patients with previously documented myocardial infarctions.
For his remarkable contributions to our understanding of patient risk factors and perioperative outcomes, Sait was recognized around the globe with honorary memberships in national societies (e.g., the Japanese Society of Anesthesiologists, the Association of Anaesthesiologists and Reanimatologists of the Republic of Kazakhstan). He received numerous awards, including the Recognition Award for Outstanding Contributions as a Pioneer of Cardiovascular Anesthesia by the World Association of Cardio-Thoracic and Vascular Anesthesia.
Sait never met anyone that he didn’t befriend and welcome. He was revered outside of the institution and admired within it. He received the Mayo Clinic’s Distinguished Clinician Award in 1993 in recognition of his lifetime of outstanding clinical care and his role in attracting and caring for many international patients who came to Mayo Clinic.
Here is this week’s Mystery Photo.

Please email your response at warner.mark@mayo.edu within 3 days of this update. I will also need your name and contact information. All correct responses will be placed into a Monday morning drawing for a $10 Starbucks card. Only one winner per individual over the 80 weeks of Mystery Photos. If you win a weekly drawing, however, please keep submitting your responses. An overall winner (with the most correct responses in the series of 80 Updates) will receive a $100 Starbucks card.

Photograph: Richard G. Belatti, M.D., undated
Sioux Falls, South Dakota: “Mayo Clinic West” in Anesthesiology
Dr. William Mayo was occasionally asked if he regretted making education such an important part of Mayo Clinic. For most of us who trained at Mayo, the question seems odd, and we ponder why anyone would have asked it. Education has always played an important role at Mayo Clinic. In fact, the Mayo brothers believed so strongly in the training of the next generation of health care providers that they donated a fair portion of their wealth to an endowment that sustains our educational programs even today. It turns out that people asked Will this question because they couldn’t understand why he and Charlie would train their future competitors. For the brothers, was not an issue that concerned them. They believed that many patients did not have access to excellent care and, therefore, they should help increase the quantity and quality of health care providers.
Their education initiatives extended beyond the training of new physicians. They consistently evaluated their practices, envisioned the types of health care providers that would be needed in the future, and created educational programs to train them. Examples of the health care fields that they started are nurse anesthesia, physical therapy, surgical assistants and technicians, and histology assistants. Their successors continued by developing the country’s first training programs for cardiac perfusionists, electro-neurodiagnostic technicians, and echocardiographic technicians. All in all, an impressive set of innovative new health care provider fields.
In many training programs, graduates leave our sites and go on to establish strong departments and groups elsewhere. Recognizing the quality of training that they received at Mayo, they subsequently reach back to our institutional programs and seek to recruit additional graduates to join them. These recruitment “pipelines” exist for many of our educational programs. Our best example in Rochester may be the pipeline of recruitment that led to anesthesia practices in Sioux Falls, South Dakota being labeled as “Mayo Clinic West.”
In 1979, Dr. Richard “Dick” Belatti completed his training in Rochester and moved to Sioux Falls where he joined Dr. Ed Daw, a 1960 graduate of our anesthesiology residency program, at Sioux Valley Hospital. Starting in 1983, Dick recruited Bill Horner (1983) to join him . . . and a cascade of Rochester anesthesiology resident graduates followed. Over time, a few of our graduates joined the anesthesia practice at McKennan Hospital (now Avera McKennan), the second Sioux Falls Hospital, and by 1995, more than 90% of the anesthesiologists in Sioux Falls were Mayo graduates. Today, 36 Mayo residency graduates have either worked or are now working in the anesthesiology practices of Sioux Falls. These include:
Sioux Valley Hospital (now part of Sanford Health)
- Ed Daw
- Dick Belatti
- Bill Horner
- Les Steidl
- Gary Halma
- Doug Bell
- Scott Atchison
- Steve Kunkel
- Arne Sorenson
- Tom Christopherson
- Kevin Ronan
- RJ Lunn
- Jack Gaspari
- Bob Grady
- Mac Sanders
- Mike Johnson
- Greg Hieb
- Barry Hein
- Casey Husser
- Marshall Holifield
- Steph Knight
- Loc Nguyen
- Brady Stocklin
- Matt Ulrich
- Ryan Rowberry
- Seri Carney
- Dan Thum
- Kelly Doolittle
Avera McKennan Hospital
- John Gray
- Scott Lockwood
- David Munce
- Dean Dewald
- Joel Farmer
- Dusty Thorpe
- Matt Naatjes
- Andy Mortensen
- Emily Fowler
Mystery Photos
Last week’s Mystery Photo is Dr. Tim Lamer.

Tim was born and raised in a small paper mill town in north central Wisconsin. After college and medical school at the University of Wisconsin, he moved to Rochester in 1983 to start our residency training program. He completed his residency as well as a Pain Medicine fellowship in Rochester and has been in the department ever since. He first split his time between the Pain Medicine Clinic and the operating rooms in Rochester. In 1991, Dr. Jim Harper recruited Tim to move to Jacksonville and help develop our Mayo Clinic Florida Pain Medicine practice and a fellowship program.
Tim was a leader in our Florida department during his 16 years in Jacksonville, starting as chair of the Pain Medicine Division and Director of the Pain Medicine fellowship program. In 1997 at the conclusion of Jim Harper’s term as department chair, Tim stepped into that role and served as chair until 2001. During that time period, Tim led the integration of the St. Luke’s private practice anesthesiology group into the Mayo department, opened an outpatient surgical center, and started what is now one of the country’s largest and most successful liver transplant anesthesia teams. He subsequently dedicated his remaining time in Jacksonville to the growth of our pain medicine practice, expansion of our fellowship program, and study of innovative techniques in pain medicine. The Pain Medicine Division became the Department of Pain Medicine in 2004 with Tim as its chair.
In 2007, Tim returned to Rochester and has dedicated his professional efforts to Pain Medicine both internally and externally. Tim has served on the editorial boards of Pain Medicine, the Pain Physician, and Clinical Journal of Pain. For the former, he is the current Section Editor on Neuromodulation and Minimally Invasive Surgery. He is a past president (2019-2020) of the American Academy of Pain Medicine. In addition, Tim has received numerous Teacher of the Year awards and was recognized in 1990 as our Rochester department’s Distinguished Clinician.
Last week’s contest winner was Michelle Ewy.
Here are this week’s Mystery Photos. With this Update #29, we will begin featuring two individuals each week for the Updates. To be placed into the Mystery Photo Starbucks contest, you will need to correctly guess at least one of the featured individuals. If you identify both of them, you will double your chances of having your name drawn.


Please email your response at warner.mark@mayo.edu within 3 days of this update. I will also need your name and contact information. All correct responses will be placed into a Monday morning drawing for a $10 Starbucks card. Only one winner per individual over the 80 weeks of Mystery Photos. If you win a weekly drawing, however, please keep submitting your responses. An overall winner (with the most correct responses in the series of 80 Updates) will receive a $100 Starbucks card.

Photograph: John Silas Lundy, M.D., 1950.
John Lundy’s Clinical Anesthesia Textbook: Unique, Controversial, and War-Worthy
John Lundy wrote one of the country’s definitive anesthesia textbooks, Clinical Anesthesia, in 1942. It remained a major educational text in the specialty for three decades. However, it was not without controversy as his writing was based primarily on his observations in clinical practice. It was not well-referenced and contained ideas that were not universally accepted. In the excerpt below, Doug Bacon has summarized the textbook, its controversies, and its important value to the men and women who shouldered much of the anesthesia care in war zones and elsewhere during World War II.
In the late 1930s there was a clear need for an updated, “modern,” comprehensive textbook of anesthesiology. In discussion between Anaesthetists’ Travel Club members Drs. Emery A. Rovenstine and Arthur Guedel, the need was clearly acknowledged. The dilemma was over who would write such a book. Guedel was concerned that he was too old and out of touch. His good friend Dr. Ralph Waters, whose department at the University of Wisconsin could surely produce a “cutting edge” tome, had neither the time nor the interest to write. Guedel urged Rovenstine, the driving force behind academic physician anesthesia in New York City to write it. Emery demurred, procrastinated and when he was starting to compose the book, W. B. Saunders published Clinical Anesthesia. John Lundy had “scooped them all.” Did Lundy know of Guedel and Rovenstine’s plans? Was there discussion about a textbook at the Travel Club Meetings in Rochester, Minnesota (1938), New York City (1939) or Boston (1940)? What part did the conflict in Europe and eventually the world play in Lundy’s decision to write?
The 1942 publication is fascinating. The forward is written by William J. Mayo, M.D. who died in July 28, 1939. Thus, the book had to be well underway in 1938 or early 1939. Dr. Mayo writes, “In this book, Dr. Lundy presents in a practical form the place of anesthesia in modern surgery.” Realizing that the reader would know that Dr. Mayo had died, Lundy inserted a small footnote, “Dr. Mayo was much interested in preparation of the manuscript of this book. He wrote the forward after one of the many conversations with the author.” In the preface Lundy describes his method for creating the book, basing it largely on clinical cases. He built in redundancy so that busy military physicians could easily find the necessary material without consulting the index.
As the 90-day courses for physicians in anesthesiology rolled out during World War II, Clinical Anesthesia was touted as the textbook to study. Clearly clinically-aimed without considerable theoretical discussions, the book was comprehensive enough for the novice. Regional anesthesia was extensively covered, an inclusion that proved to be a lifesaver in combat anesthesia. But at 771 pages, it might well have been difficult to transport for physicians near the front.
Perhaps the March 1943 review of the book in Anesthesiology by editor-in chief and fellow Travel Club member Dr. Henry Ruth best sums the book’s importance. It is remarkable for its polite but valid notations of potential controversial statements in the textbook, which Henry S. Ruth, M.D., comments on in a book review. He noted that Clinical Anesthesia was essentially a unique compilation of the personal experiences of a clinician with a wide and varied practice. Ruth also noted that there were few illustrations and references. Thus, the book was not structured or written in the format of the modern academic textbook. It never had a second edition and had one post-war second printing.
Mystery Photos
Last week’s Mystery Photos were Burdette (Bud) Polk, CRNA and John T. (Tom) Martin, M.D.

Bud Polk was our first nurse anesthesia supervisor in Jacksonville when he moved from Rochester in 1986. Bud was born in Independence, Iowa. He completed his nurse anesthesia training in Rochester in 1968. After one year working in LaCrosse, Wisconsin at Gunderson Lutheran Hospital, he was recruited back to Rochester by Dr. Emerson Moffitt, chair of our Division of Cardiac Anesthesia. He served as the supervisor for our cardiac practice, working closely with Emerson and others in the operating rooms and on research projects. Things were soon to change for Bud, though.
Our intensive care units (St. Marys Hospital and Rochester Methodist Hospital ICUs) were established in 1966 by Dr. Albert Falconer (chair of the department from 1955-1969). Dr. Paul Didier, with Renee Caspersen, CRNA, developed the Methodist Hospital ICU and Dr. Alan Sessler, with Bernie Gilles, CRNA, developed the St. Marys Hospital ICU. Bud joined the expanding Section on Intensive Care in 1972 as the new supervisor of our intensive care services at RMH. Other key members supporting the growing number of intensivists and critically ill patients included Myron Ricks, CRNA (1970), Lester Clapp, RT (1971), and Tom Holtackers, PT (1972).
In 1982, Bud transitioned back to the operating rooms, working closely with Steve Schmidt. Four years later, he decided to move to Jacksonville. He was joined by colleagues Drs. Jim Harper and Tim Shine and nurse anesthetists Linda Buck, Alicia Cassabar, and Phil Klineschmidt. These six individuals provided the anesthesia care for the Mayo Clinic patients who were receiving their care at St. Luke’s Hospital in south Jacksonville. They were joined by others in 1987 and, by 1988, they were appointed as a group to be the Department of Anesthesiology at Mayo Clinic in Jacksonville. Jim Harper served as the department’s first chair. Parenthetically, the department cooperatively worked with the pre-existing private practice anesthesia group at St. Luke’s Hospital for a decade until the department took over full provision of anesthesia services for all patients in 1996. Bud served as the supervisor for the new department during its first 5 years before Linda Buck, CRNA succeeded him in the role in 1991. From 1991 through 2003, Bud provided care for cardiac patients and joined the nascent liver transplant service.
Bud retired in 2003 and lives today in Palm Coast, Florida. Palm Coast has 26 miles of saltwater canals connecting to the ocean, fitting Bud’s love for boating. In fact, he was a yacht broker for a period of time after his anesthesia career.

Tom Martin was the first mentor that Mary Ellen and I had when he was chair of the Department of Anesthesiology at the Medical College of Ohio in Toledo. It was Tom who sent us to Rochester for our ASA Medical Student Preceptorships in 1978 and introduced us to Drs. Alan Sessler, Duane Rorie, Jim Prentice, Ted Janossy, Mark Sperry, Gary Baggenstoss, Charley Rich, and so many others great anesthesiologists and residents. Ann Brumm, Jane Post, and Donna Baxter worked in the department offices at that time and made sure we knew how to get to our daily assignments. In those assignments, nurse anesthetists such as Alice Johnson, Jeanne Tiemans, John Carter, Mary Marienau, Jack Hostak, and others graciously tolerated our ineptitude and lack of knowledge and taught us how anesthesia care was provided at Mayo Clinic.
Tom was born in Cleveland, Ohio but grew up primarily in the Cincinnati area. His mother, Clara Martin, worked at Miami University in Oxford, Ohio and started the student boarding system and food services in that institution. Today, Martin Hall is one of the university’s primary dining halls and one that I used my first year at Miami. Tom met Marion, his wife of 59 years, in high school and they became a dynamic couple on the music scene during their time in Rochester (1958-1972). Marion was a master pianist and Tom was extraordinary as a trombonist. Tom was a member of the Mayo Clinic Notochords stage band, the Rochester Symphany Orchestra, and the Rochester Park Band. He also served as president of the Rochester Civic Music organization.
Tom was drafted into the military in 1944 and was the first graduating US. Air Force anesthesiology resident at Lackland Air Force Base (Wilford Hall) in 1948. Tom served as the Air Force’s residency program’s director until moving in 1958 to Rochester to join our department. He was the division chair downtown when the Rochester Methodist Hospital was being built and designed many of the elements in the hospital’s new operating rooms. The hospital opened in 1966. In 1972, Tom moved to New Orleans as chair of the Ochsner Clinic’s Department of Anesthesiology. After a short 2-year stint in that role, he moved to the Medical College of Ohio (MCO), joining Dr. Lucien Morris and colleagues. At MCO, he succeeded Dr. Morris as chair, served as medical director of intensive care and president of the MCO Faculty Senate.
Tom gained international recognition for his reports, presentations, and book dedicated to patient positioning. His text, “Positioning in Anesthesia,” was the primary authority of patient positioning during surgical procedures for more than 3 decades. Tom also was very involved in pre-hospital care training. He was the medical director of the northwest Ohio emergency medical technician program and paramedic training. He continued our department’s leadership of the International Anesthesia Research Society by serving as president of its Board of Trustees from 1979-1981. He was an editor of Anesthesia & Analgesia from 1966-1977. Tom passed away in 2005 in Toledo, Ohio. I was honored to speak at his funeral.
Mystery Photo Contest Winner
Last week’s contest winner was Tom Murphy.
Here are this week’s Mystery Photos.
Reminder: We are now featuring two individuals each week for the Updates. To be placed into the Mystery Photo Starbucks contest, you will need to correctly guess at least one of the featured individuals. If you identify both of them, you will double your chances of having your name drawn.


Please email your response at warner.mark@mayo.edu within 3 days of this update. I will also need your name and contact information. All correct responses will be placed into a Monday morning drawing for a $10 Starbucks card. Only one winner per individual over the 80 weeks of Mystery Photos. If you win a weekly drawing, however, please keep submitting your responses. An overall winner (with the most correct responses in the series of 80 Updates) will receive a $100 Starbucks card.








Photograph 1: Brad Narr, M.D., 2015. Photograph 2: Natalie Caine, undated. Photograph 3: James Hebl, M.D., undated. Photograph 4: Marlea Judd, APRN, CRNA, DNP, undated. Photograph 5: Carlos Mantilla, M.D., undated. Photograph 6: Pam Bowman, MBA, undated. Photograph 7: Jams Ottevaere II, M.D., undated. Photograph 8: Darlene Bannon, RN, CRNA, undated.
Mayo Clinic Expands in the Midwest . . . and the Department of Anesthesiology in the Midwest Grows Dramatically
In the late 1980s and early 1990s, managed care gained momentum as a preferred health care model in the Upper Midwest, specifically in the Twin Cities area. In 1993, the Hiliary Clinton-led “Task Force on National Health Care Reform,” advocated strongly for managed care models. Although the Clinton Health Care Reform recommendations ultimately failed to advance through Congress, the task force’s advocacy for managed care increased enthusiasm for this model of care. Managed care models in the Twin Cities of Minneapolis and St. Paul led to many mergers of independent providers into rapidly growing health care systems such as Allina Health and Health Partners. This consolidation of practices and limitations on patients who wished to get their health care outside of their health systems restricted patient choice in the Minnesota market and raised the specter of reduced Rochester visits from Minnesota patients. In addition, the Clinton Health Care Reform proposed barriers between states, potentially reducing inter-state competition, an action that would have negatively impacted the number of potential patients who could travel to Rochester by choice.
In response, Mayo Clinic formed its own health system in 1992, initially called the Mayo Health System. The name changed in 2011 to its current Mayo Clinic Health System. I had the privilege of serving on the initial institutional committee that considered opportunities to secure our Midwest future by forming our own health care system. Led by Dr. Michael O’Sullivan (Department of Laboratory Medicine & Pathology), the committee discussed which hospitals and practices within 150 mile radius of Rochester might best augment our Mayo missions, benefit from Mayo Clinic support and resources, and protect our referral interests. I specifically mention our Mayo missions as our clinical schools (i.e., medical school, graduate medical education school, and health sciences school) were growing and more clinical experiences were needed for the increased number of trainees. A summary of the growth of the Mayo Clinic Health System can be found at Mayo Clinic Health System - Wikipedia and in a Mayo Clinic Proceedings article from 2003.
There initially was no mandate or even encouragement for hospital-based departments such as anesthesiology and radiology to engage with our growing new partners in the health system. However, over time our department began providing support for our anesthesia colleagues in Austin, Albert Lea, Red Wing, and other sites. Our electronic ICU practice started to provide services across the system. Preferential referrals for pain medicine followed. In February 2014, Dr. Brad Narr created a Division of Community Anesthesiology within the department. Dr. Jim Hebl was appointed as chair of the division and Marlea Judd, CRNA was appointed as the division’s nurse anesthesia director. Mirroring the overall health system, the Division of Community Anesthesiology organized into 4 regions.
- The Northwest Wisconsin Region was overseen by Dr. Richard Belmont and Gram Cotton, CRNA
- The Southwest Wisconsin Region was overseen by Dr. Peter Schams and Michael (Jake) Jacobson, CRNA
- The Southeast Minnesota Region was overseen by Dr. Jennifer Goins; Ryan Sportel, CRNA (River Corridor) and Alice Schrad, CRNA (I-90 Corridor)
- The Southwest Minnesota Region was overseen by Dr. Tim Murray and Steve Ydstie, CRNA
The Division of Community Anesthesiology was initially comprised of 46 anesthesiologist and 108 nurse anesthetists. The division sought to evolve to implement a single operational and strategic structure that would align with the remainder of the institution-wide Department of Anesthesiology, including major initiatives and clinical protocols involving quality and patient safety and outcomes. Integration was a major challenge at times. As one example, in 2015/2016, we had 18 unique paper anesthesia records in the health system sites as we sought to transition to a single electronic record system.
Dr. Sandy Kopp succeeded Jim Hebl as division chair in 2015. Jim became the Regional Vice-President of the Southwestern Region of the overall health system and is based in Mankato. Today, the division has 66 anesthesiologists and 129 nurse anesthetists. An additional 9 anesthesiologists in Rochester support the community practices. Dr. Jim Ottevaere of Eau Claire currently chairs the division. Darlene Bannon, CRNA, becomes the division’s CRNA director this month.
The anesthesiology sites in the health system create many opportunities for educating our many trainees. All four regions train student nurse anesthetists from our Rochester and LaCrosse programs. Mankato and Eau Claire have resident rotations at this time. Most of our sites teach paramedic and EMT students from local community schools as well as nurse practitioner and physician assistant students. Without our sites in the Mayo Clinic Health System, we would fall short of our educational needs in our Rochester anesthesiology residency and two nurse anesthesia training programs. All of our division anesthesiologists and CRNA leaders hold academic rank in the Mayo Clinic College of Medicine and Science.
The 2014 leadership of the Department of Anesthesiology in Rochester and its Division of Community Anesthesiology: Brad Narr, department chair; Natalie Caine, department administrator; Jim Hebl, division chair; and Marlea Judd, CRNA director.
The 2024 leadership of the Department of Anesthesiology in Rochester and its Division of Community Anesthesiology: Dr. Carlos Mantilla, department chair; Pam Bowman, department administrator; Jim Ottevaere, division chair; and Darlene Bannon, CRNA director.
Mystery Photos
Last week’s Mystery Photos were Steve Rose, M.D. and Karen Hammell.

Steve Rose was born in St. Paul, Minnesota. He graduated from “the most prestigious public high school” in Valley City, North Dakota (population 6,000+). Our own Drs. Niki Dietz and Kami Anderson are also graduates of Valley City High School. Steve moved on to Concordia College in Moorhead, Minnesota and Mayo Medical School before completing his anesthesiology residency at Mayo Clinic. With help from Dr. Martin Abel, Steve spent a year as a Senior Registrar at Groote Schuur Hospital in Cape Town, South Africa and several months in London, England as a Mayo Foundation Scholar before joining the Mayo faculty in 1985.
Steve was an outstanding athlete in high school, a talent that paid dividends during his training. He played as an all-star on various intramural, departmental, and community flag football and broomball teams. In one of the most shining successes in his training, he resuscitated a fellow broomball player from a cardiac arrest on the ice. Today, he and his wife, Dr. Beth Elliott, continue to participate in sports as avid, expert downhill skiers and frequent swimmers.
The focus of Steve’s non-clinical career has been medical education. He served as residency program director from 1994-2007 and as the department’s Vice Chair for Education from 1994-2009. He was the Mayo Clinic School of Graduate Medical Education’s (MCSGME’s) Associate Dean for Surgery and Surgical Specialties from 2003-2009; Vice Dean from 2007-2012; and Dean from 2012-2021. He also was the school’s Designated Institutional Official (DIO) from 2007-2022. As DIO, he oversaw and governed nearly 200 accredited residency and fellowship programs that trained more than 1,900 residents and fellows annually.
Steve was appointed to the national Accreditation Council for Graduate Medical Education’s (ACGME’s) Institutional Review Committee in 2017 as served as its chair from 2020-2023. This is one of the country’s most important leadership roles in graduate medical education. He is the first Mayo physician to serve in the role since an earlier version of it was established by Dr. Louis Wilson, one of Mayo Clinic’s pioneers in pathology and education. In 2022, Steve received two of the highest honors for a physician in education, the Mayo Clinic Distinguished Educator Award and the ASA’s Excellence in Education Award. This article summarizes his many educational accomplishments.
Three of six MCSGME Deans have been members of the Department of Anesthesiology. Dr. Alan D. Sessler was the inaugural Dean. He served as a mentor to Dr. Mark A. Warner and to Steve (the second and third department members, respectively, to serve in this position).
In clinical practice, Steve works in our Central Division at St. Marys Hospital, caring for patients undergoing complex orthopedic, spine, and thoracic procedures.

Karen Hammell was born in Rochester and attended school in Chatfield. After completing studies as an administrative secretary, Karen joined Mayo Clinic, working with the Mayo Clinic School of Graduate Medical Education (MCSGME) for 5 years. She subsequently worked within our institution’s Legal Department before joining our department in 1991 as the Education Program Coordinator for our residency. Her program director partners during her 31 years of stellar time as the residency coordinator have been Drs. Leslie Milde, Steve Rose, Tim Long, and Bridget Pulos.
Karen has been a primary contact for our trainees during her three decades with the residency program in Rochester. She’s been remarkably successful and respected. She was recognized in 2017 with the MCSGME Education Program Coordinator Award in Surgery and Surgical Specialties, the institution’s highest recognition for that position. In 2023, she was recognized by the Mayo Fellows Association with its Fellow Award. The award is given to exceptional individuals who are extraordinarily committed to our residency and fellowship programs and their success.
Karen will retire in June this year after more than 3 decades of service to our residency program in Rochester. She has 7 grandkids in the St. Charles and Plainview areas who will benefit from her new-found time. Best wishes, Karen!
Mystery Photo Contest Winner
Last week’s contest winner was Karen Nase.
Here are this week’s Mystery Photos. Reminder: We are now featuring two individuals each week for the Updates. To be placed into the Mystery Photo Starbucks contest, you will need to correctly guess at least one of the featured individuals. If you identify both of them, you will double your chances of having your name drawn.

Please email your response at warner.mark@mayo.edu within 3 days of this update. I will also need your name and contact information. All correct responses will be placed into a Monday morning drawing for a $10 Starbucks card. Only one winner per individual over the 80 weeks of Mystery Photos. If you win a weekly drawing, however, please keep submitting your responses. An overall winner (with the most correct responses in the series of 80 Updates) will receive a $100 Starbucks card.









Photograph 1: Gary Boeke, M.D., undated. Photograph 2: Phil Boyle, M.D., undated. Photograph 3: Lorrie Bennett, CRNA, undated. Photograph 4: Tom Spackman, M.D., undated. Photograph 5: Jack Bagby, M.D., undated. Photograph 6: Richard Olson, M.D., undated. Photograph 7: Jill Hardy, CRNA, undated. Photograph 8: John Gray, M.D., undated. Photograph 9: Matt Ritter, M.D., undated. Photograph 10: Chris Martin, undated. Photograph 11: Cathy Cook, CRNA, undated. Photograph 12: Tera Wenzel, CRNA, undated.
Department of Anesthesiology: Exemplary Humanitarian Efforts
In Update #6 (October 12, 2023) we read about humanitarian medical efforts led by Drs. David Byer and Kelly McQueen. In this Update, Anesthesiology alumni Gary Boeke (1983) and Phil Boyle (1984), as well as Plastic Surgery alumnus Paul Schultz (1985), provide a summary of their efforts and many other Mayo physicians, nurse anesthetists, and operating room personnel in Guatemala for more than the last three decades. As a department, we are blessed that many of our colleagues are involved in humanitarian medical efforts. This summary provides an excellent example of many of our alumni and staff coming together in a sustained effort to help others.
“Guatemala is a beautiful country known as the “Land of Eternal Spring.” The indigenous Mayan people have a rich heritage. From 1960 until the peace accord in 1996, Guatemala was embroiled in a civil war. As a result of war and poverty, HELPS International was organized as a relief/development organization dedicated to assisting the indigenous population. An integral part of this effort has been to bring medical-surgical teams to the needy.
Central Minnesota was the first HELPS medical team to volunteer in Guatemala in 1988 and 1989. Mayo alumni on those teams were Drs. Gary Boeke (Anesthesiology 1983), Philip Boyle (Anesthesiology 1984), Paul Schultz (Plastic Surgery 1985), Paul Heath (Plastic Surgery 1983) and James Smith (Plastic Surgery 1983). Subsequently, other medical teams were established over the years from around the US. For the year 2024 there are 9 medical teams scheduled to serve. The original 1988 team only had 7 volunteers; several of the current teams have 80-90 volunteers. The teams and the care they provide are self-funded. Central Minnesota has continued to field 2 teams per year for the last 36 years. Most medical teams provide 3-4 surgical sites along with medical clinic and dental staffing. The most frequent operations performed are hernia repairs, cleft lip and palate repairs, cholecystectomies, burn scar revisions, and gynecological surgeries. Ophthalmological services may also be provided when available. Lack of basic medical care in Guatemala makes for challenging cases. Most teams perform 130-180 surgical cases during their trips.
Other Mayo Clinic alumni have volunteered and continue to serve on HELPS teams over the 36 years of the program. They include Drs. Tom Spackman (Anesthesiology 1980), Jack Bagby (Anesthesiology 1983), Chris Martin (Anesthesiology 1994, Pain Medicine 1996), Dick Olson (Anesthesiology 1984), John Gray (Anesthesiology 1984) Matt Ritter (Anesthesiology 2005, Critical Care Medicine 2006), Chris Schmidt (Surgery 1992) and Mike Sarr (GI Surgery, 1980). Mayo volunteer nurse anesthetists include Lori Bennet, Jill Hardy, Tera (Cox) Wenzel, and Cathy Cook. Several Mayo Clinic nurses and OR technicians have also joined the teams.
HELPS is also involved with community development. This involves providing stoves (over 300,000 installed), a corn micro-loan program, water filters and educational sponsorship. The medical experience in Guatemala has been very rewarding for the many involved. Quality care is given, and gratitude returned. Instead of monetary remuneration, hearts are filled. The opportunity has often allowed families of team members to be involved and share in the joy of medicine and serving. The experiences have impacted the vocations of many. Lives are changed, both the people served and the people serving.”
Mystery Photos
Last week’s Mystery Photos were Beth Elliott, M.D. and Allan Gould, M.D.

Beth Elliott was born and raised in Kentucky. After medical school at the University of Louisville in 1981, Beth moved to Rochester to begin her training in Anesthesiology. Her fellowship year in Rochester focused on Regional Anesthesia/Pain and Neuroanesthesia. She joined the staff in 1985, originally working at Rochester Methodist Hospital with the Vascular and Gynecologic surgeons. Beth eventually moved to St. Marys Hospital to join the Ortho Anesthesia group where she was integral to the development of the Acute Pain Service and the use of epidural analgesia for thoracic surgery patients. She also helped cover chronic pain consults at St. Marys Hospital, creating a busy block practice in addition to her work in the operating rooms. In 1995, Beth was named Division Chair of the Ortho Anesthesia group where she promptly led an effort to rename it the Central Division. She continued in this leadership role until 2005. She was awarded the Clinician of the Year award by her peers in 2007.
As a visiting medical student in 1980, Beth had the serendipitous opportunity to care for Dr. Virginia Hartridge as one of her first patients. Dr. Hartridge was the longtime medical director for the Nurse Anesthesia program at Mayo. This led to her initial interest in the nurse anesthesia program, triggering an educational pursuit that became a major part of her stellar career. Beth succeeded Dr. Bob Lennon as medical director for the nurse anesthesia program in 1991 and has held it to this day. Along with her CRNA colleagues, program directors Ed Thompson, CRNA and Mary Marienau, CRNA, she helped guide the program over the ensuing decades in the transitions from a Certificate program to a master’s degree program to the Doctor of Nurse Anesthesia program that it is today. In recognition of her long-term commitment and contributions to the education, Beth was awarded the Distinguished Educator Award from Mayo Clinic in 2009. This award is Mayo Clinic’s highest recognition in education.
Anyone who sees Beth away from the OR (meaning not wearing scrubs) knows that she loves scarves and can be seen wearing one almost every day. Her collection of Hermes scarves goes back many years, adding to her travel adventures and making friends across the USA and Europe.
In addition to her scarves, Beth enjoys quilting and needlepoint. She and her husband of 33 years, Steve Rose, are avid skiers and still spend several weeks a year chasing the perfect powder day at Vail. Beth holds a unique distinction of having not just one . . . but three (!) holes-in-one on various golf courses around Minnesota. She is as skilled on the golf course as she is in clinical practice and education.
Dr. Allan Gould was born in Buffalo, NY and grew up in Piqua, Ohio. After college at Ohio State University, he attended Jefferson Medical College in Philadelphia, graduating in 1952. Within a week of graduating, he married Marilyn Buxton, his wife of 52 years. He served in the U.S. Army after an internship in Philadelphia and the first year of his anesthesiology residency training at Mayo Clinic in Rochester. He joined the Korean conflict as a physician in a Mobile Army Surgical Hospital (MASH) unit. He often chuckled at the humor and simultaneously shook his head in disbelief at the way movies and television shows depicted MASH units. He described his time in Korea in a department newsletter article written in 2003.
After the conflict, Allan returned to Rochester to complete his anesthesia training and joined the staff in 1958. He had a distinguished career as a remarkable clinician. In his retirement year of 1991, Allan was recognized by his colleagues with the department’s Distinguished Clinician Award. For 8 years from 1972 through 1980, he chaired the Section of Anesthesia at the Rochester Methodist Hospital. Extramurally, Allan served as an ABA oral examiner, an editor of the ASA Newsletter, chair of the ASA Annual Meeting (twice!), and a member of the ASA’s Board of Governors. He also was president of the Minnesota Society of Anesthesiologists.
Allan was widely admired by his colleagues. He and Marilyn enjoyed their five children, 8 grandkids, and 5 great grandkids during their retirement. They found great joy in working with the walnut trees they planted on their Fillmore County farm in southeast Minnesota and watching birds. Allan passed away on October 14, 2014.
Mystery Photo Contest Winner
Last week’s contest winner was Dr. Joe Messick.
Here are this week’s Mystery Photos.
Reminder: We are now featuring two individuals each week for the Updates. To be placed into the Mystery Photo Starbucks contest, you will need to correctly guess at least one of the featured individuals. If you identify both of them, you will double your chances of having your name drawn.

Please email your response at warner.mark@mayo.edu within 3 days of this update. I will also need your name and contact information. All correct responses will be placed into a Monday morning drawing for a $10 Starbucks card. Only one winner per individual over the 80 weeks of Mystery Photos. If you win a weekly drawing, however, please keep submitting your responses. An overall winner (with the most correct responses in the series of 80 Updates) will receive a $100 Starbucks card.
Photograph: James C. Eisenach, M.D.
Department of Anesthesiology Alumnus: The Outstanding Dr. Jim Eisenach
There are few alumni who have been at the forefront of anesthesiology research and advances in the specialty more than Dr. James C. (Jim) Eisenach. Jim graduated from the University of California, San Francisco School of Medicine in 1982. After an internship in that city, he came to Rochester for his residency training, entering what was to be the graduating class of 1985 with future academicians such as Brad Narr, Beth Elliott, and Tim Shine. A great summary of Jim’s time in Rochester is found in Reminiscences, his short story written for our May 2005 department newsletter.
Jim left Rochester in 1985 and served one year as a fellow in obstetric anesthesia at Wake Forest University in North Carolina. He had left Mayo with a newly written NIH proposal in hand . . . and the start of nearly 40 years of continuous NIH funding in which he systematically studied selective spinal analgesics. He is a rare recipient of an NIH MERIT Award. He quickly rose to professor rank and holds the Francis M. James, III, M.D. Professorship of Anesthesiology. Jim was very involved in the American Society of Regional Anesthesia (ASRA) leadership and served at the ASRA president in 2003. ASRA recognized his contributions with its 2005 John J. Bonica Award, its 2008 Gaston Labat Award, and its 2012 Distinguished Service Award.
Jim’s excellence in research put him on a path that led to his becoming one of the most influential anesthesiologists in the country. Jim served as Editor-in-Chief of Anesthesiology from 2007-2016 and president of the Foundation for Anesthesia Education and Research from 2016-2023. He was inducted into the National Academy of Medicine in 2015, received the American Society of Anesthesiologists’ Excellence in Research Award in 2013, and gave the ASA’s Emery Rovenstine Lecture in 2015 and its John Severinghaus Lecture in Translational Science in 2021.
Best of all, Jim is a really great person and a strong advocate for Mayo Clinic. Congratulations, and thank you for all you’ve done for the specialty, Jim.
Mystery Photos
Last week’s Mystery Photos were Dan Cole, M.D. and Albert Faulconer, M.D.
Dan Cole was born in Washington, D.C. and raised in Michigan. After graduating from Andrews University in Berrien Springs, Michigan (20 miles northwest of South Bend, Indiana), he earned his M.D. from Loma Linda University, 60 miles east Los Angeles. He also completed his anesthesiology training there. Dan subsequently was a neuroanesthesiology fellow at the University of California, San Diego. Dan was a faculty member at Loma Linda University from 1986 through 2003. During his time in California, he rose within the California Society of Anesthesiologists’ leadership, serving as president in 2001-2002. He also was president of the Society of Neuroscience in Anesthesiology and Critical Care from 2001-2002. It was obviously a very busy year.
Dan moved to Phoenix in 2003 and became chair of our Mayo Clinic Arizona Department of Anesthesiology. During that period, he worked with Dr. Renee Caswell and started our residency program and led a time of departmental growth which included the addition of a cardiac transplant and assist device program, and expansion of non-operating room anesthesia. He also served as the Vice-Dean of our Mayo Clinic School of Continuous Professional Development. Dan moved to the University of California, Los Angeles in 2013 as vice-chair of its Department of Anesthesiology. A prolific author and investigator, he currently is Professor of Anesthesiology at UCLA.
Dan is one of only 17 anesthesiologists who have served as president of both the American Society of Anesthesiologists and the American Board of Anesthesiology. While with the ABA, Dan was its Executive Director of Professional Affairs for 4 years. He also has been a director of the Foundation for Anesthesia Education and Research. In 2021, Dan became president of the Anesthesia Patient Safety Foundation and holds that position currently. Dan initiated the ASA’s Perioperative Brain Health, one of the specialty’s major initiatives to improve patient safety in the past 4 decades. He was recognized in 2020 by the ASA with its Distinguished Service Award, joining 6 other Mayo Clinic colleagues as a recipient of that award.
Dan and his wife, Cristine, have two sons (Steven and Andrew) and live in San Monica, California.
Addendum: Although Dan has experienced many memorable events over the years, I am pleased to report that one of the better ones occurred during a summer visit to Rochester when I invited him to speak to our local colleagues and residents. Since it was a social event, I took Dan to lunch with a small group and we sat outside at Famous Dave’s restaurant. Yes, I was being frugal with our Mayo budget. Unfortunately, Dan sat in a large dollop of the restaurant’s famous BBQ sauce. His light tan pants were colorful, to say the least. Knowing that he had an upcoming presentation in the later afternoon, we rushed to my home to wash his pants. Dan is fit, in shape, and weighs less than two-thirds of what I do, so the substitute gym shorts I could provide as a temporary substitute were a little on the large size. A nice piece of rope as a belt fortunately saved the day until the dryer had completed its task. To be fair to Dan, I am not sharing any of the funny photos from that afternoon.

Albert Faulconer was born in Arkansas City, Kansas, south of Wichita near the Oklahoma border. He graduated from the University of Kansas Medical School in 1936. After a general internship and medicine residency, plus several years in clinical practice, he came to Rochester in 1943 as part of the 90-day “short course” anesthesia training for physicians who would subsequently play a major role in caring for injured soldiers/seaman/marines during WWII. After the war, he returned to Rochester, joining the anesthesia staff after only 6 months of clinical anesthesia training during his abbreviated residency. He was an exceptional research talent, developing an acoustic gas analyzer as part of his master’s degree thesis. The department almost lost him to Boston’s Harvard programs but a reportedly impassioned plea by Dr. John Lundy to the Mayo Board of Governors resulted in him being hired as a consultant before completing his training.
Albert became a major force in anesthesiology research during his career. An excellent summary of his career and legacy has been published by our own Drs. Peter Southorn, Mary Ellen Warner, Alan Sessler, and Kai Rehder. He used EEG techniques to determine the impact of both inhaled and intravenous anesthetics on the cerebral cortex. He demonstrated that nitrous oxide worked as an anesthetic . . . an assumption that was not universally accepted in the late 1940s and early 1950s. At that time, there was a prevailing wisdom that nitrous oxide worked through diffusion anoxia of the brain. He used a pressure chamber to give percentages of nitrous oxide greater than 80% but ensuring sufficient oxygen to volunteers who were in 2 atmospheres of pressure. He used EEG monitoring of the brain to detect changes depicting levels of anesthesia but not cerebral hypoxia.
His experience with EEG techniques led him to the concept of intraoperative cerebral monitoring to estimate depth of anesthesia. From that and work he did to show that anesthetics, especially intravenous anesthetics, lost their cerebral effects by distribution to other tissues in the body, he developed a computer-activated model to predict uptake and distribution of anesthetics. This then led him to use the model to test a servo-controlled anesthetic machine and a similar intravenous anesthetic infusion device. He soon found that a “closed-loop” computer approach to delivering anesthesia was not going to be successful without the input of trained anesthesia personnel. However, his work formed the basis of today’s processed cerebral monitors to estimate depth of anesthesia.
Albert’s outstanding and novel research earned him a position for 11 years (1950-1961) on the National Research Council’s Committee on Anesthesia. The Research Council was and continues to be the operational arm of the National Academy of Sciences. He was a founder of the Association of University Anesthesiologists and its president in 1956. He also was a director and president of the American Board of Anesthesiology during the 1955-1969 period. In 1953, he was appointed as chair of our Section of Anesthesiology and Intravenous Therapy. He led the section through several name changes, including 1970 when it was renamed as the Department of Anesthesiology. He stepped down as department chair in early 1971. He was a member of the Mayo Clinic Board of Governors from 1963 through 1969. Albert died on December 10, 1985.
Mystery Photo Contest Winner
Last week’s contest winner was Dr. Marie DeRuyter.
Here are this week’s Mystery Photos.
Reminder: We are now featuring two individuals each week for the Updates. To be placed into the Mystery Photo Starbucks contest, you will need to correctly guess at least one of the featured individuals. If you identify both of them, you will double your chances of having your name drawn.


Please email your response at warner.mark@mayo.edu within 3 days of this update. I will also need your name and contact information. All correct responses will be placed into a Monday morning drawing for a $10 Starbucks card. Only one winner per individual over the 80 weeks of Mystery Photos. If you win a weekly drawing, however, please keep submitting your responses. An overall winner (with the most correct responses in the series of 80 Updates) will receive a $100 Starbucks card.

Photograph: Hugo Raimundo, M.D., undated.
Department of Anesthesiology Innovations: The Anatomy Laboratory
Dr. John Lundy came to Mayo Clinic in 1924 with a vision for the specialty’s evolution. Far ahead of nearly all other early leaders of the specialty, he looked into the future and dreamed of ways that he and the colleagues he would recruit could have a positive impact in medicine beyond the operating rooms. One of his first steps was to expand the scope of anesthesia through the education of surgical (and subsequently anesthesia) fellows in anesthetic as well as surgical techniques. With the support of Drs. Will and Charlie Mayo, he developed an anatomy laboratory in which trainees could perform procedures and dissections on cadavers, in essence establishing one of the country’s first simulated surgical programs. His anatomy laboratory evolved into today’s Department of Anatomy at Mayo Clinic and its two major programs, the Microsurgery Training Center and the Clinical Anatomy Lab. His concept of anatomic training (i.e., cadaveric simulation) has been widely adopted in health science programs, medical schools, and graduate medical education across the U.S. and internationally.
Our own Drs. Terry Ellis and Doug Bacon summarized Lundy’s remarkable vision and actions in establishing the anatomy laboratory in their excellent 2003 Mayo Clinic Proceedings article.
The Passing of Dr. Hugo Raimundo
Although the Centennial Updates are written to provide historical information and context on the development of our department and the important innovations and leadership roles of department members, it seems appropriate to use the Updates to share news that will match with the interests of many of our Update readers.
In this instance, it is the passing of Hugo Raimundo. He was a major contributor to the strong and successful pediatric cardiac surgical program in Rochester. The following is taken from an obituary dedicated to him.
“Dr. Raimundo died peacefully in his Phoenix home near the Mayo Clinic Hospital on March 7, 2024 following a courageous battle with idiopathic pulmonary fibrosis.
Hugo was born in 1937, in Panaji, Goa, India, which at the time was a Portuguese Colony. At the age of 17 he left Goa, traveling by boat across the Arabian Sea and through the Suez Canal to Portugal. He settled in Oporto where he went to medical school and interned at Hospital de Sao Joao from 1954-1961. He served mandatory time in the Portuguese Armed Forces as a medical officer from 1961 – 1965 and was in the horrific fighting within the jungles of Angola for much of that time. In 1965, Portugal remained under the dictatorship of Antonio Salazar and it was necessary for him to arrange travel to the United States, under cover, where he arrived with one suitcase containing all of his earthly belongings. He interned at Robert Packer Hospital, Guthrie Clinic in Sayre, Pennsylvania from 1965 – 1966. - He entered the Mayo Graduate School as a resident in general surgery in January 1967 and transferred to anesthesiology in 1969. He was appointed Consultant, Department of Anesthesiology, Mayo Clinic Rochester in 1972, specializing in cardiac anesthesia, with a special interest in pediatric cardiac anesthesia. He retired on December 31, 1999.”
Mystery Photos
Last week’s Mystery Photos were Duane Rorie, M.D. and Emerson Moffitt, M.D.

Duane Rorie was born in Yellville in the north central region of Arkansas in 1936. He completed his undergraduate and M.D. degrees at the University of Arkansas, then earned a Ph.D. in anatomy from the University of Mississippi. He subsequently moved to Rochester for his anesthesiology residency and joined the staff in 1970. With the initial class of the new Mayo Medical School entering in 1972, Duane became the school’s first anatomist and taught clinical anatomy for 10 years as well as working in our department and obtaining his first NIH grant in 1977. He continued his success with a string of NIH grants until 1999. His grants focused on understanding the mechanisms and impact of anesthetics on norepinephrine and other neuropeptides, specifically how anesthetics attenuate sympathetic vasoconstriction. His clinical research was directed towards the anatomic considerations of regional anesthetic techniques.
Duane served as the chair of our department’s Division of Anesthesiology at Rochester Methodist Hospital from 1980 through 1991. He advanced to chair of the department and continued in that role until 1999. He was an examiner of the American Board of Anesthesiology and a member of multiple honorary societies within the specialty. His excellence in research and education was recognized by the institution when he was appointed as its Reuben Eisenberg Professor in 1991. He is one of only 4 department members to be recognized as a named professor. Upon completing his role as department chair, Duane was asked to serve as the medical director of Mayo Clinic’s Procedural Skills Laboratory. His appointment brought the department full circle as the anatomy laboratory was first started by our own Dr. John Lundy in 1925 (see section above on the anatomy laboratory’s origin). Duane’s return to clinical anatomy leadership was defined by his refinement and expansion of the Procedural Skills Lab (Clinical Anatomy Lab – RST (mayo.edu) as well as his advocacy for a new Microsurgery Training Center Microsurgery Training Center (mayo.edu).
On rare instances, Duane would tell of the start of his rise within the Mayo Clinic hierarchy. He delighted in telling the story of his first committee role at Mayo . . . and as its chair, no less. He was asked to lead the institution’s Meal Policy Committee by Dr. Gene Mayberry, chair of our Board of Governors at the time. Candidly, there are only a handful of committees lower on the rung of Mayo’s committee ladder. One of those is the Surgical Scrub Suit Policy Committee . . . which was my first committee assignment as a chair (thank you, Bob Waller, successor to Gene Mayberry). Both chair roles were challenging (and a little painful) because few personnel affected by the policies of these two committees are happy about them. Duane and I shared more than a few laughs at how these assignments launched our careers, nearly derailing them right from the start.
Duane passed away on March 7, 2014. His obituary in the Rochester Post-Bulletin may be found at Dr. Duane K. Rorie — Rochester - Post Bulletin | Rochester Minnesota news, weather, sports. Dr. Stephen Carmichael, emeritus professor of anatomy, wrote a tribute about Duane’s contributions to Mayo Clinic. Duane had a wonderful wife of 50 years, Carolyn, and two daughters.

Emerson Moffitt was born in New Brunswick, Canada in 1924. He went to the University of New Brunswick in Fredericton, although his undergraduate studies were interrupted by WWII and service in the Canadian Royal Navy Fleet, Air Arm. He graduated from Dalhousie Medical School in Halifax, Nova Scotia in 1950 and entered general practice in North Sydney, Nova Scotia near Cape Breton Island. During his three years in general practice, he delivered hundreds of general and spinal anesthetics, triggering his desire to pursue further anesthesia training. In 1954 he moved to Rochester as a new resident working with John Lundy and others. He became very interested in the launch of the institution’s first cardiopulmonary bypass use in March 1955. Under the mentorship of Dr. Jeremy Swan (of Swan-Ganz catheter fame) and working with colleagues such as Drs. John Kirklin (CV Surgery), Earl Wood (Physiology), and Bob Patrick (Anesthesiology), he studied the physiologic effects of cardiopulmonary bypass and the management of anesthesia, anticoagulation, transfusion, and electrolytes during bypass. His work at that time, augmented by further studies with fellow anesthesiologists Drs. Dick Theye, Bob Devloo, Alan Sessler, and Dick Lundborg, led to the specialty’s fundamental understanding of cardiopulmonary bypass and management of cardiac surgical patients. Our own Drs. Adam Jacob, Doug Bacon, and Hugh Smith wrote an outstanding, well-referenced summary of Emerson’s contributions in 2007. Dr. Peter Southorn also wrote a wonderful, more personal story in 2004 about Emerson’s time at Mayo Clinic in our department newsletter.
Emerson chaired the department’s Division of Anesthesiology at St. Marys Hospital from 1966 through 1971. In 1971, Dick Theye was chosen to succeed Dr. Albert Faulconer as chair of the newly renamed Department of Anesthesiology. Two other valued candidates for that position were Emerson and Dr. John (Tom) Martin. That transition, coupled with the early death of Emerson’s wife in 1972, triggered Emerson to decide to return with his two daughters to Nova Scotia. He was offered and accepted a position as chair of his medical school alma mater’s Department of Anesthesiology. His work in Nova Scotia and his ascent as Dean of Clinica Affairs at Dalhousie are well documented in David Shephard’s excellent summary.
Here are this week’s Mystery Photos.
Reminder: We are now featuring two individuals each week for the Updates. To be placed into the Mystery Photo Starbucks contest, you will need to correctly guess at least one of the featured individuals. If you identify both of them, you will double your chances of having your name drawn.


Please email your response at warner.mark@mayo.edu within 3 days of this update. I will also need your name and contact information. All correct responses will be placed into a Monday morning drawing for a $10 Starbucks card. Only one winner per individual over the 80 weeks of Mystery Photos. If you win a weekly drawing, however, please keep submitting your responses. An overall winner (with the most correct responses in the series of 80 Updates) will receive a $100 Starbucks card.
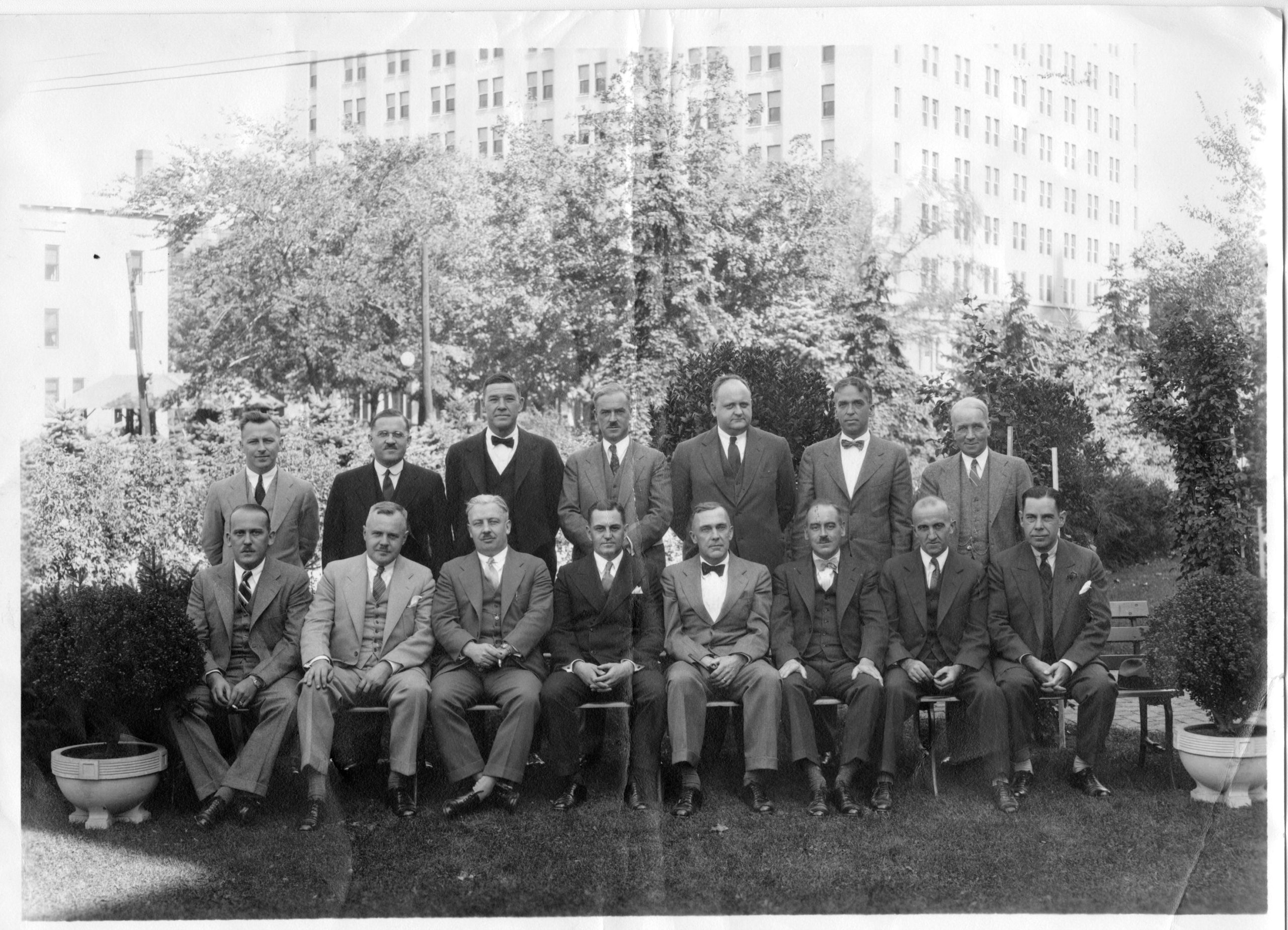
Photograph: Anesthetists' Travel Club, 1933.
The Department of Anesthesiology: The Start of the Anesthetists’ Travel Club and the Evolution of the Specialty
In 1929, Dr. John Lundy invited leading anesthesiologists from the U.S. and Canada to Rochester to form the Anesthetists’ Travel Club. This club would meet annually until the start of WWII. The founders shared ideas and clinical practices. Most became leaders in their national organizations and greatly influenced the evolution of the specialty. Our own Drs. Ron Mackenzie and Doug Bacon wrote about the influence of Drs. Will and Charlie Mayo on the organization of the Travel Club. The article provides remarkable insights into the influence wielded by Will and Charlie in U.S. surgery and by John Lundy and his Mayo colleagues (i.e., Charles McCuskey and Ralph Tovell) on U.S. and Canadian anesthesia.
Mystery Photos
Last week’s Mystery Photos were Ralph Tovell, M.D. and Theresa (Terre) Horlocker, M.D.

Ralph Tovell was born in Sydenham, Ontario, Canada in 1901. He earned his M.D. degree from the Queen’s University in Kingston, Ontario in 1926. He immediately moved to Rochester as one of Dr. John Lundy’s first fellows. He remained in Rochester until moving in 1939 to become the chief of anesthesiology at Hartford (CT) Hospital. Several wonderful, brief summaries of Ralph’s contributions to the specialty’s development may be found at Ralph M. Tovell, M.D.* - Wood Library-Museum of Anesthesiology (woodlibrarymuseum.org) and Dr Ralph Moore Tovell | The Royal College of Anaesthetists (rcoa.ac.uk). For brevity, let me summarize several of his remarkable key accomplishments:
- 1938: Helped found the American Board of Anesthesiology.
- 1939: Chief of Anesthesia, Hartford (CT) Hospital, remaining in that role until 1963.
- 1940: Became a U.S. citizen.
- 1940: Appointed as Associate Editor, Anesthesiology, a position he held until 1955, becoming Editor-In-Chief at that time.
- 1941: President, American Society of Anesthesiologists.
- 1942: Appointed as Senior Consultant in Anesthesia for the U.S. Army, European Theatre of War, discharged at the rank of Colonel.
- 1947: President, American Board of Anesthesiology.
- 1948: Chair, AMA Section on Anesthesia.
- 1951: Recipient, ASA Distinguished Service Award.
- 1955: President, Academy of Anesthesiology
Two examples of Ralph’s contributions are his advocacy that led to the adoption of the Pin-Index safety system for gas cylinders and his contributions to developing safer anesthesia care during WWII.
He died on January 7, 1967. Dr. David Little, another early leader in the specialty, wrote his obituary in Anesthesiology.

Terese (Terre) Horlocker is a native of Rochester, born in St. Marys Hospital on April 2, 1959. She likely has the lowest Mayo Clinic number of any active member of our staff. Terre graduated from the University of Minnesota and Mayo Medical School and then completed her training in anesthesiology here in Rochester in 1989. Classmates in her residency class who worked on staff in the department included Mark Ereth, Bob Friedhoff, Mike Johnson, Tom Losasso, Bill Perkins, Kevin Ronan, and Margaret Weglinski.
Terre has become one of the leading anesthesiologists in the world in regional anesthesia, with special recognition for her work in understanding the risks of anticoagulants and the use of neuraxial anesthetic techniques. Soon after joining our staff in 1989, she began working closely with Dr. Denise Wedel on projects to define the risks of regional anesthesia and especially neuraxial anesthesia. Early papers with Denise and hematologist Dr. John Heit led to our understanding of anticoagulation risks and her leadership in developing guidelines for their use with regional anesthesia. These guidelines have been used worldwide for more than a quarter of a century, a remarkable testimony to their value and appropriateness.
Terre has been a leader in regional anesthesia and the department and institution. Examples of her leadership roles and awards include:
- 1998: Chair, FDA Anesthesia and Life Support Drugs Advisory Committee
- 2000: Chair, Division of Methodist North Anesthesia
- 2003: Chair, ASA Committee on Regional Anesthesia
- 2004: Section Editor (Regional Anesthesia), Anesthesia and Analgesia
- 2005: President, American Society of Regional Anesthesia (ASRA)
- 2008: Chair, Mayo Space and Remodeling Committee
- 2009: Recipient, ASRA Distinguished Service Award
- 2011: Recipient, ASRA Gaston Labat Award
- 2011: Recipient, Minnesota Society of Anesthesiologists’ John Lundy Award
- 2020: Recipient, ASRA Trailblazer Award
An excellent story about Terre, told by her, is found in the 2020 ASRA Newsletter about Women in Regional Anesthesia.
Terre will retire this May. Her humor, stories, wit, and knowledge will be sorely missed.
Mystery Photo Contest Winner
Last week’s contest winner was Tibor Mohácsi.
Here are this week’s Mystery Photos. Reminder: We are now featuring two individuals each week for the Updates. To be placed into the Mystery Photo Starbucks contest, you will need to correctly guess at least one of the featured individuals. If you identify both of them, you will double your chances of having your name drawn.


Please email your response at warner.mark@mayo.edu within 3 days of this update. I will also need your name and contact information. All correct responses will be placed into a Monday morning drawing for a $10 Starbucks card. Only one winner per individual over the 80 weeks of Mystery Photos. If you win a weekly drawing, however, please keep submitting your responses. An overall winner (with the most correct responses in the series of 80 Updates) will receive a $100 Starbucks card.
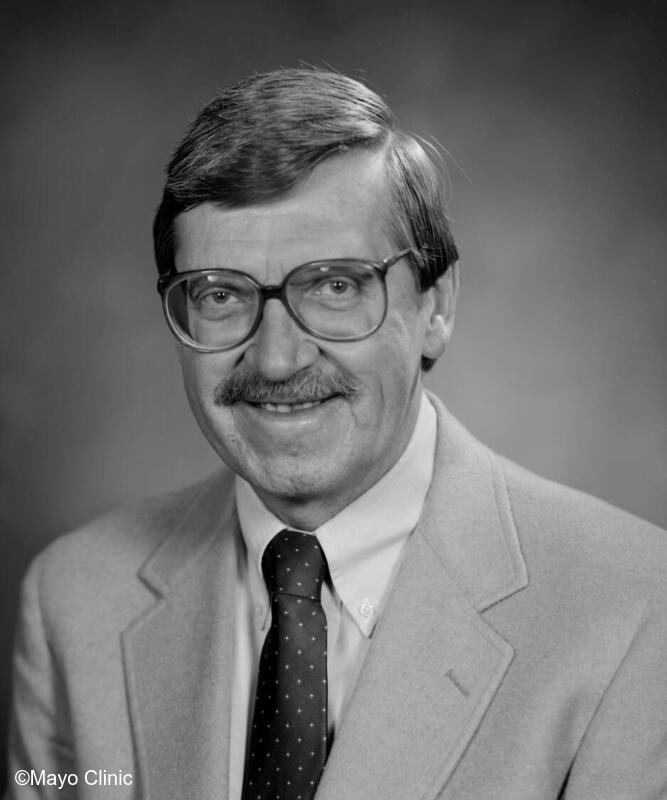
Photograph: Roger D. White, M.D., undated.
The Department of Anesthesiology: The Miraculous Superhero Professor Roger White
Few people have made a greater impact on medicine that Dr. Roger White. His expertise in cardiac anesthesia, understanding of cardiac rhythms, treatment of cardiac arrest, and leadership of Emergency Medical Services have resulted in numerous awards. More importantly, they have saved many lives.
Roger was born in 1939 in Ontonagon, Michigan. A neat trivia question about Ontonagon: What incorporated U.S. town or city is the furthest west of any that use the Eastern Time Zone? It is just east of the Porcupine Mountains Wilderness State Park along Lake Superior and an hour’s drive SW of Houghton, Michigan in the Upper Peninsula. It’s remarkable that a young man from Ontonagon has become one of the world’s most recognizable names in cardiac resuscitation.
Roger graduated from the University of Michigan and its medical school. After an internship at Henry Ford Hospital in Detroit in 1965, he moved to Rochester to start as a resident in Internal Medicine. His residency was interrupted by a 2 year tour of duty with the U.S. Army during which time he received on-the-job training in anesthesiology. It was a career-changing event as he returned to Rochester and switched his residency training to our specialty. It was our win and Internal Medicine’s loss. He went on to start working in cardiac anesthesia, a subspecialty in which he has worked for 54 years on the Mayo Clinic staff . . . and counting as he still continues to work clinically as well as on research projects.
This description in the October 2, 1970, Mayovox announces the start of his time on staff in Rochester:
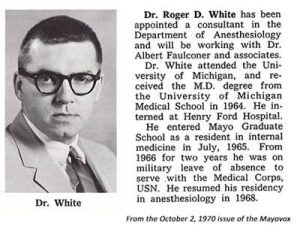
During his career, Roger has advocated for emergency medical services. He played a major role in establishing Rochester and southeast Minnesota’s emergency medical services. During his second year on staff, he wrote an excellent article describing the importance of physicians as leaders in pre-hospital emergency care. He became deeply involved in introducing advanced cardiac life support training into our Mayo Clinic hospitals and emergency medical services and instituting cardiac telemetry, radio communications between emergency services and physicians, and the use of resuscitation intravenous medications in pre-hospital settings.
Examples of Roger’s incredible contributions to emergency medical services include the 1990 introduction of early defibrillation in Rochester (defibrillators in fire trucks, ambulances, and police cars). At that time, the program reported the highest survival rates in the U.S. from out-of-hospital cardiac arrest and ventricular fibrillation. In 2008, Roger and 5 colleagues authored the American Heart Association’s recommendations on “hand-only” (“chest compressions-only”) cardiopulmonary resuscitation techniques. In 2011, Roger oversaw the 96-minute resuscitation of a man in cardiac arrest in Goodhue, Minnesota. He survived neurologically intact; it is believed to be the world’s longest successful resuscitation from cardiac arrest. Here you can read a case report and watch a video about this resuscitation. In recognition of his contributions, Roger was inducted into the Emergency Medical Services (EMS) World Hall of Fame in May 2022. Mayo’s Discovery Edge (Winter 2012) turned Roger and his team into superheroes in their description of their work . . . perhaps the best way to describe hyper-achievers.
There is so much more that can be said about Roger. He taught many of us who are left-handed how to cannulate the right internal jugular vein before ultrasound was introduced into routine practice. He led many Rochester department members annually through modified CPR training and dazzling us as he taught us how to recognize common as well as rare rhythms. Nearly every Rochester department member reached out to Roger for advice on how to interpret ECGs in the perioperative period. Less known is his classic ambulance collection.
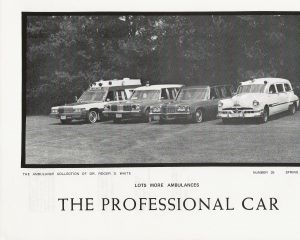
An excellent video documentary about Gold Cross Ambulance, featuring Roger’s narrative, will be posted online at the National Emergency Medical Services Museum later this month (Virtual National EMS Museum - EMS Museum). Here is a photo from that video:
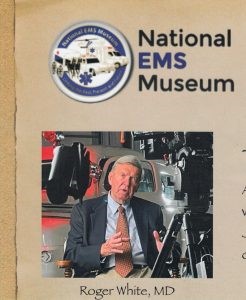
Congratulations, Roger, on an outstanding career. And for many more years that we can lean on your expertise.
Mystery Photos
Last week’s Mystery Photos were Joseph Messick, M.D. and Michael Geisler, CRNA.

Joe Messick was born in Wilmington, Delaware in 1935. After college at Wesleyan University in Middletown, Connecticut, he earned his M.D. degree from the University of Virginia School of Medicine. He was a resident in anesthesiology at the Presbyterian Hospital in Philadelphia, one of several hospitals affiliated with the University of Pennsylvania, from 1961 through 1964. He then spent two years in the U.S. Navy. Upon completion of his military duties, Joe moved to Rochester for additional training in anesthesiology and earned his Master’s degree from the University of Minnesota. His mentors for his thesis were Drs. Dick Theye, Albert Faulconer, Ward Fowler, and Jack Michenfelder, a pretty star-studded group. His thesis was directed towards understanding the impact of common anesthetics and adjuvant drugs on whole body and cerebral oxygen consumption rates.
Joe was integrated into what was then, and was to remain, one of the most productive and visible neuroanesthesia groups in the world. He joined colleagues such as Drs. Jack Michenfelder, Kai Rehder, and Gerry Gronert. He was initially assigned to the cardiac group, but when Gerry was drafted into the Army, he was asked to transition to neuroanesthesia. Drs. Roy Cucchiara, and Ron Faust soon followed as members of the group, as did Drs. Leslie Milde and Bill Lanier. It was a remarkable period of discovery in neuroanesthesia. Drs. Thor Sundt, Ed Law, Frank Sharbrough, and others in neurosurgery and neurology contributed. Joe chaired the Section on Neuroanesthesia from 1978 through 1984. During that period he led the introduction of routine use of mass spectrometry into neuroanesthesia in Rochester, a project he and Dr. Duane Rorie expanded to all Rochester operating rooms during the mid-1980s when they chaired the Divisions of St. Marys Hospital Anesthesiology and Rochester Methodist Hospital Anesthesiology, respectively. Their strong support for mass spectrometry and the installation of pulse oximeters into every operating room during their division chair tenures led to advanced intraoperative monitoring that transformed the specialty and patient safety at Mayo Clinic.
Joe served as chair of the Division of St. Marys Hospital Anesthesiology from 1984 through 1988. He earned Teacher of the Year recognition in 1988 as he transitioned his clinical activities and leadership to the management of in-hospital pain. He was indefatigable in that role, starting a pain medicine fellowship and in-patient services at both Rochester hospitals. He chaired the Division of Pain Medicine until his retirement in 1997. He retired as a Professor Emeritus.
It is worth noting that Joe was a wonderful and gentle soul with an amazingly gracious bedside manner. That characteristic served him well throughout his career, whether in patient care or administrative leadership roles. He was president of the Minnesota Society of Anesthesiologists in 1977-1978. He currently resides in Rochester.

Mike Geisler completed his nurse anesthesia education at the Mayo School of Health Related Science in 1984. Before that, he worked at Rochester Methodist Hospital as an RN in the old "11-1 Unit" (Respiratory ICU) and then as the Head Nurse of the Plastic Surgery Unit. Mike's father served our country as a member of the Defense Intelligence Agency of the US Army, which influenced Mike's childhood by living in numerous places around the world. He and his family lived in Tehran, Iran, for three years, in Bangkok, Thailand, for four years, and in Frankfurt and Stuttgart, Germany, for eight years. He spent most of his childhood in other countries, exposed to various cultures and languages. Mike was fluent in Thai as a toddler.
Mike and his family returned to the US in time for him to complete his senior year of high school in Southern Pines, North Carolina. Two years after graduating from high school, in 1972, Mike received his military draft notice. He enlisted in the US Navy and served as a Corpsman with the US Marine Corps. As a corpsman, he became aware of the profession of nurse anesthesia by watching Navy CRNAs at work in the operating room. This exposure led him down his professional career path, which he enjoyed for 38 years.
In 1997, Mike was asked by Dr. Jeffry Steers, a Liver Transplant surgeon in Rochester, to assist him in organizing and educating a new Liver Transplant team for Mayo Jacksonville. Mike was an integral part of the Rochester anesthesia team and participated, along with Dr. Steve Rettke, in the first liver transplant in Rochester. When Dr. Steers approached Mike about relocating to Jacksonville, the Mayo Department of Anesthesiology in Jacksonville was comprised of approximately 10 CRNA's and 8 anesthesiologists. A short time after the formulation of the Liver Transplant Team, he was asked by Dr. Tim Lamer, Chair of the Department of Anesthesiology, to assume the position of Chief CRNA. As a result of the Mayo Jacksonville Liver Transplant program and subsequent heart and lung transplantation, the nurse anesthesia component of the Anesthesia Care Team grew to approximately 34 CRNAs. Mayo Jacksonville’s Liver Transplant Program evolved into the nation's most extensive and successful liver transplant program.
Mike has been recognized for his clinical expertise and contributions beyond the boundaries of Mayo Clinic. In 1999, he was awarded the American Association of Nurse Anesthetists’ Clinical Practitioner of the Year Award. Mike remained in the Chief CRNA position in Jacksonville until 2002. He subsequently followed his desire to return to clinical practice, retired from the Chief position, and returned as a staff member in the department. He retired from Mayo in 2007 but not from the practice of nurse anesthesia. In 2007, Mike and his wife Deb formed an anesthesia staffing group that provided anesthesia services to local surgery centers, oral surgery groups, and hospitals. In recognition of Guedel's teachings, the group was named "Stage II Anesthesia."
Mike continued providing anesthesia services until his retirement in 2022. He currently lives in Jacksonville, FL, on the Intracoastal Waterway within view of the Mayo Clinic campus. He enjoys fishing, sailing, playing guitar, and spending time with family, including three lovely grandchildren.
Mystery Photo Contest Winner
Last week’s contest winner was Sandy Simonson.
Here are this week’s Mystery Photos. Reminder: We are now featuring two individuals each week for the Updates. To be placed into the Mystery Photo Starbucks contest, you will need to correctly guess at least one of the featured individuals. If you identify both of them, you will double your chances of having your name drawn.
Please email your response at warner.mark@mayo.edu within 3 days of this update. I will also need your name and contact information. All correct responses will be placed into a Monday morning drawing for a $10 Starbucks card. Only one winner per individual over the 80 weeks of Mystery Photos. If you win a weekly drawing, however, please keep submitting your responses. An overall winner (with the most correct responses in the series of 80 Updates) will receive a $100 Starbucks card.

Photograph: Jeff Korsmo, M.D., undated.
The Department of Anesthesiology: Our Administrators
The Mayo Clinic partnership between physicians, nurses, and other providers in leadership teams with administrators has proven to be a key reason for the institution’s long-term success. In essence, our medical leaders develop ideas to improve clinical care, education, research, and patient safety and satisfaction, sharing these ideas with our administrative partners. Our partners, with their broad wealth of knowledge about practices, personnel and financial issues, and healthcare delivery, bring their insights and projections to these developing proposals and work collaboratively to finalize them. Once approved, our administrative colleagues partner with our medical leaders to garner the appropriate resources and implement the proposals. The bonds our medical leaders form with our administrative partners often last a lifetime and spur others to work together.
Examples of key administrative leaders who have achieved the highest administrative roles in the institution after their time in our department include:
Jeff Korsmo. Jeff went on to serve as the Chief Financial Officer for Mayo Clinic Florida, executive director of the Mayo Clinic Health Policy Center, and Mayo Clinic’s Chief Administrative Officer, partnering with Dr. Denis Cortese in this latter role.

Bob Brigham. Bob went on to serve as the Chief Administrative Officer for Mayo Clinic Florida, partnering with Dr. George Bartley in this role.

Steve Jorgensen. Steve went on to serve as the Director and Chair of Education Administration, partnering with Mark Warner in his Executive Dean role.

Gwen Amstutz. Gwen continues to serve the institution, has been the administrative leader of the institution’s Surgical and Procedural Committee partnering with Dr. Brad Narr, chair of the Division of Surgical Administration, secretary of the institution’s Clinical Practice Committee, and currently is the administrative leader of the Harwick Project.

Natalie Caine. Natalie continues to serve the institution, has been chair of administration for the Department of Internal Medicine and currently is the Chief Administrative Officer in Rochester, partnering with Dr. Gianrico Farrugia.

Roshy Didehban. Roshy continues to serve the institution, has been chair of Practice Administration for the institution and currently is the Chief Administrative Officer in Arizona, partnering with Dr. Richard Gray.

Ajani (AJ) Dunn. AJ continues to serve the institution and currently is Chief Administrative Officer in Florida, partnering with Dr. Kent Thielen.

Mystery Photos
Last week’s Mystery Photos were David L. Brown, M.D. and Jeffrey J. Lunn, M.D.

David Brown, M.D. was born in Ames, Iowa and raised in Wayne, Nebraska. He received an appointment to the U.S. Military Academy to play football but turned that opportunity down to attend Iowa State University. It was clearly a good decision as Dave met his wife, Kath, while at Iowa State. He subsequently graduated from the University of Minnesota Medical School in 1978. He did his residency at Wilford Hall U.S. Air Force Medical Center in San Antonio and spent 11 years in the Air Force. During part of that period, he served as a flight surgeon with 319th Bombardment Wing of the Strategic Air Command in Grand Forks, North Dakota.
After his time in the Air Force, he joined the Virginia Mason Clinic in Seattle, Washington where he became chair in 1987 until he left in 1990 to join the Mayo Clinic. He spent seven years in Rochester and practiced both in the pain clinic and orthopedic group at Methodist Hospital. He left our institution in 1997 to become Professor and Chair of Anesthesia at the University of Iowa. During that time he rebuilt the department with additional staff and renewed energy in education and research. The same pattern occurred when he left the University of Iowa in 2004 to become Edward Rotan Distinguished Professor and Chair of the Department of Anesthesiology and Pain Medicine at the University of Texas, MD Anderson Cancer Center in Houston. Rebuilding academic anesthesia programs was in , and the pattern repeated again in 2008 when he accepted his final Chair position as the Professor of Anesthesiology, Cleveland Clinic Lerner College of Medicine, Cleveland, Ohio. After reflecting on his institutional leadership changes, he came to believe what he enjoyed was the excitement of turning a department around.
During his academic time, Dave completed a number of books, one of which, Atlas of Regional Anesthesia, was awarded the Anesthesia Foundation book award in 1994; it is now in its 7th Edition. His research focused primarily on pancreatic cancer pain control, and he spent five years as Editor in Chief of Regional Anesthesia and Pain Medicine. ASRA also provided him opportunity as its president, and awarded him the Labat Award, and Distinguished Service Award. He also served in leadership roles for the American Board of Anesthesiology, the ACGME, the RRC for Anesthesiology, the Association of University Anesthesiologists, and FAER.
He retired clinically and academically in 2015 from the Cleveland Clinic to form a healthcare startup, Curadux. This provided individuals with advanced illness the benefit of a physician care guide walking alongside their consequential health decisions. The firm closed in 2020.
He and his wife, Kath, split their time between a small ranch in Texas, and the lake in Hayward, Wisconsin. He currently spends time addressing substance misuse on a local Ojibwe reservation and leads a small home church – Solid Rock Church.

Jeff Lunn, M.D. was born in 1952 in Bismarck, North Dakota. His primary interest in high school at Bismarck High related to sports. Jeff went to the National Junior Olympics in Knoxville, Tennessee in 1968 and ran in the 100-yard dash (yes, he is in an age group that came before track in the U.S. switched to the metric system). He also earned athletic recognition in football and basketball. Despite his obsession with sports in high school, he did graduate and go on to North Dakota State University, graduating in 1974. After completing medical school at the University of North Dakota and a surgical internship at the University of South Dakota, Jeff moved to Rochester and was an anesthesiology resident from 1980 through 1982. He then spent a year working with Dr. Duane Rorie as a Special Clinical Fellow in Duane’s lab. In addition to being certified in anesthesiology, he also holds a certificate in critical care medicine.
Jeff joined our staff in Rochester in 1983 and then subsequently joined Mayo Clinic in Arizona in 1992. From 1992 through 1998, Jeff served as the chair of the Department of Anesthesiology during its transition from working at Shea North Memorial Hospital (currently HonorHealth Scottsdale Shea Medical Center) to the new Mayo Clinic Hospital on the Phoenix campus. He also served as the chair of the Department of Critical Care Medicine at Mayo Clinic Arizona from 1996 through 1998. During his time in these leadership roles, Jeff and colleagues established our Preoperative Evaluation Clinic (1995) and the Department of Critical Care Medicine (1996). For the latter effort, he partnered closely with Dr. Joel Larson, his best “wing man” ever. While in Phoenix, Jeff was chair of the Mayo Clinic Arizona Clinical Practice Committee from 1994 through 1997.
In 2007, Jeff moved to Kingman, Arizona and joined the Kingman Regional Medical Center. It serves as the primary center for northwest Arizona and was one of the first medical centers to join the Mayo Clinic Care Network thanks to Jeff and his partnership with Jim Anderson, one of our leading administrators in Mayo Clinic Arizona at the time. While at Kingman, Jeff helped start the hospital’s cardiac surgical program and served in multiple leadership roles, including as Chair of Surgery, Vice Chief of Staff, and Chief Medical Officer. Jeff theoretically “retired” in January 2023 but still works intermittently in critical care medicine on contract.
Jeff and colleagues from Kingman Regional Medical Center formed a non-profit foundation in 2010. “Live Now.” This foundation provided surgical services at multiple locations in Tanzania. In addition, they became involved in the area near Lake Eyasi, Tanzania located at the southern border of Serengeti National Park and immediately southwest of the Ngorongoro Crater. Live Now has helped built a medical center and other facilities for members of the indigenous Hadzabe, Datoga, and Maasai people of that area.
Jeff and his wife, Barb, have finally returned to a lake home in northern Minnesota.
Mystery Photo Contest Winner
Last week’s contest winner was Marcia Belau.
Here are this week’s Mystery Photos. Reminder: We are now featuring two individuals each week for the Updates. To be placed into the Mystery Photo Starbucks contest, you will need to correctly guess at least one of the featured individuals. If you identify both of them, you will double your chances of having your name drawn.
Please email your response at warner.mark@mayo.edu within 3 days of this update. I will also need your name and contact information. All correct responses will be placed into a Monday morning drawing for a $10 Starbucks card. Only one winner per individual over the 80 weeks of Mystery Photos. If you win a weekly drawing, however, please keep submitting your responses. An overall winner (with the most correct responses in the series of 80 Updates) will receive a $100 Starbucks card.
Photograph of Robert Chantigian, M.D., undated.
Mayo Fellows Association Teachers of the Year Hall of Fame
The Mayo Fellows Association began to select Teachers of the Year for all Rochester-based departments in mid-1970s. In 1986, the association created a Teachers Hall of Fame to recognize the most outstanding of the excellent teachers and their sustained efforts. To enter the Hall of Fame, individuals need to be selected four or more times by the Mayo Fellows Association as Teachers of the Year. The Mayo Fellows Associations in Florida and Arizona started in the early 1990s but created a Teachers Hall of Fame recently in 2021. For this reason, no anesthesiologists in these two sites have yet reached their respective Halls of Fame.
In Rochester, only five of the more than 400 current or former anesthesiologists on our staff since the mid-1970s have reached the Teachers Hall of Fame. These are Drs. Bob Chantigian, Brian McGlinch, Jeff Pasternak, Rick Rho, and Paul Warner. These colleagues deserve our recognition and immense gratitude for the significant time and effort commitments they have made to didactic, group, and one-on-one teaching.
Mayo Clinic (Rochester) Nurse Anesthesia Program: Teachers of the Year with Multiple Recognitions
The Nurse Anesthesia Program in Rochester selects three Teachers of the Year annually. One is the Physician Teacher of the Year and the other two are Nurse Anesthetist Teachers of the Year (one who works primarily at Rochester Methodist Hospital and the other at St. Mary's Hospital). Since 2003, only seven individuals have received multiple Teacher of the Year awards from the program. These are Drs. Jeff Pasternak and Bob Chantigian and nurse anesthetists Jay Bergner, Lisa Dearborn, Jay Martin, Francie Lovejoy, and Joan Njus. As with the members of the Mayo Fellows Association’s Teachers Hall of Fame, congratulations to each for their remarkable dedication to the education of our trainees.
The History of the Mayo Clinic Ambulance Program in Rochester
Centennial Update # 36 (May 9, 2024) highlighted the contributions of Dr. Roger White to the development of the field of emergency medical services. The Mayo Clinic Heritage Program has just this week summarized key activities over nearly 100 years of the institution’s ambulance service. It is a quick read. I believe you may find it to be very interesting. Please note that all Mayo campuses were illuminated last evening, Wednesday, May 22nd in blue and white light in recognition of National Emergency Medical Services week.
Mystery Photos
Last week’s Mystery Photos were Thomas N. Spackman, M.D. and Brian Dawson, M.D.

Tom Spackman, M.D. was born in Edmonton, Alberta in 1949. He attended undergraduate school at both Brigham Young University and the University of Alberta. He earned his M.D. degree in 1976 from the University of Alberta. He worked in general practice in Cardston, Alberta until 1978 when he moved to Rochester as a resident in anesthesiology. After graduating in 1980, Tom moved to Pocatello, Idaho and joined a private practice, returning to Mayo Clinic in Rochester in 1982. In 1993, he received a Master of Science degree in Administrative Medicine from the University of Wisconsin in Madison.
Tom chaired our Rochester Division of Cardiovascular/Thoracic Anesthesiology from 1988 through 1996, then transitioned to serve as department Vice-Chair for our Midwest Regional Anesthesiology practices. In that role he served as a member of the Board of Trustees for both the Albert Lea and Austin (MN) medical centers. Tom was very involved in the Minnesota Medical Association from 2000 through 2008, leading several reference committees at the association’s annual meetings.
In February 2009, Tom moved to Jacksonville and served as chair of our Mayo Clinic Florida Department of Anesthesiology until 2013. During his tenure as chair, the department grew, especially its exceptional solid organ transplant program and neuroanesthesia practice. Tom retired in 2014 but continued for several years as a supplemental consultant in Jacksonville. Many of his colleagues remember Tom as a gracious, humble, and unflappable colleague. Tom and his wife, Susan, have five children.
Brian Dawson, M.D. was born in 1927 in Staplecross, Sussex, England. He received both his Bachelor (1951) and Medical (1954) degrees from the University College in London. After residency training in anesthesiology at the University College Hospital in London, Brian moved to Rochester and completed our training program in 1959. After 15 years on staff in Rochester, he moved to Phoenix, Arizona and spent 6 years in private practice at the Phoenix Surgi Center, the country’s first dedicated free-standing ambulatory surgical center (please link to Ambulatory Surgical Centers History here). Brian returned to Rochester in 1981 and became an extraordinarily effective teacher of pediatric anesthesia. He chaired the Section on General Anesthesia at St. Mary's Hospital from 1981 through 1985. In that role, he became one of the institution’s leading advocates for expanding outpatient surgical practices. He was beloved by his colleagues and the entire department.
In responses I’ve had to the Mystery Photo contest, I’ve gotten comments ranging from how he would bring fresh trout into staff after a successful day of fishing the streams of SE Minnesota and NE Iowa to how he would use his gold-plated laryngoscope (which is still in my office) for intubating the most difficult airways. Dr. David Hatch, world-renowned pediatric anesthesiologist at Great Ormond Street Children’s Hospital in London, tells the following story, “Brian and Sonia (his wife) were very close, another couple who made me so welcome in Rochester. In early 1969 Brian took me from snow-bound Rochester to my first major pediatric anesthesia conference in Los Angeles, where I met Drs. Digby Leigh and Jackson Rees, the latter over from the UK. On the way, we stopped off in Las Vegas. I remember Brian telling me that it is better to be snowed out of Rochester than snowed in!!”
Brian passed away after a motor vehicle accident on October 31, 1981. Dr. Paul Stensrud was an intern working in the emergency room at St. Mary's Hospital that afternoon and I was the anesthesiologist who responded to the emergency room when Brian was brought in. It is a day that neither of us will ever forget and incredibly heart-breaking. A mass was held in the St. Mary's chapel to recognize Brian’s humanity and graciousness, especially in caring for children. The nurses of the St. Mary's Hospital pre and postoperative units named the preoperative pediatric area in his honor and dedicated a plaque in his name. Brian is survived by his wife, Sonja. She currently resides in the Charter House just to the north of Rochester Methodist Hospital. Sonja designed the institution’s 3-shield emblem as described in Centennial Update #8 (October 26, 2023).
Mystery Photo Contest Winner
Last week’s contest winner was Glenn Fromme.
Here are this week’s Mystery Photos. Reminder: We are now featuring two individuals each week for the Updates. To be placed into the Mystery Photo Starbucks contest, you will need to correctly guess at least one of the featured individuals. If you identify both of them, you will double your chances of having your name drawn.

Photograph: Bertha Davis Clark, undated.
The Mayo Clinic Department of Anesthesiology: Bertha Margaret (Davis) Clark, M.D., Our First Female Anesthesiology Resident
Drs. Doug Bacon and Rob Strickland have written previously about our first Mayo Clinic female anesthesiologist, Dr. Isabella Herb (Centennial Update #12; November 23, 2023). Today, Doug provides a wonderful summary of Dr. Bertha (“Bert”) Davis Clark, the first woman physician to train in our department. A special thank you to Doug for this contribution.
Bertha Maragret Davis-Clark, nicknamed “Bert,” was an anesthesiology resident in our department from October 1, 1935, until April 1, 1940. She was one of the first residency-trained anesthesiologists in Jackson, Mississippi and Houston, Texas. Bertha played a major role in establishing anesthesiology departments in both of these cities. Her move to Houston was prompted by a change in practice by her husband, surgeon Lee Clark, M.D. after World War II. While she helped establish a busy anesthesia department in Houston at Hermann Hospital (now Memorial Hermann- Texas Medical Center), he became the first permanent director of MD Anderson Cancer Center.
Born Bertha Margaret Davis in Asheville, North Carolina on January 16, 1908, she attended the Medical College of Virginia where she was the only woman in the class. Bert was a scholar, graduating salutatorian of the medical college in 1932; her soon-to-be husband was the class valedictorian. Talk about a dynamic couple! On June 11, 1932, she married Lee, and they began a rotating internship at Garfield Hospital in Washington, DC. She would start a general practice in the area for a year until the young couple went to Paris, France for further training. While in Paris, Bert took additional courses in obstetrics.
On October 1, 1935, Bert and Lee arrived in Rochester. Lee entered surgical training. Initially, Bert started in the clinic’s pathology training program. She subsequently switched to anesthesiology, although the reasons for this change are unknown. She would finish training on April 1, 1940, having spent 4 months in surgical pathology, 3 months in hospital medicine, 3 months in pediatrics, 6 months in gynecology, and 23.5 months in anesthesiology. During her training, she and Lee had two children. This was a remarkable and unusual situation during that time period for three reasons: (1) there were few physician couples, (2) there were few physician couples training concomitantly, and (3) there were few woman physicians who had children during their residency training. Bert and Lee’s daughter Jo Lynn “Reba” Clark was born on June 16, 1937, during her training. A son, Randolph Lee Clark, III would follow on May 14, 1939.
Upon completing their training in 1940, Lee and Bert began practice in Jackson, Mississippi. Bert was the first residency-trained anesthesiologist in the state and Lee had a very busy surgical practice. Very early in her time in Jackson, Bert befriended a young general practitioner, Dr. John Pender. She convinced him to go to the Mayo Clinic to train in anesthesiology. Dr. John Lundy, who admired Bert and considered her to be one of his favorite residents, quickly accepted Dr. Pender upon Bert’s recommendation. Dr. Pender became one of our Rochester staff anesthesiologists in 1946 after serving in the U.S. Navy reserve during an interruption of his training. Dr. Pender went on to become the chair of the Department of Anesthesiology at the Palo Alto (California) Medical Clinic, an associate editor of Anesthesiology (1956-1965), president of the Academy of Anesthesiology (1965), and trustee of the Wood Library Museum of Anesthesiology and the Audio-Digest Foundation.
In 1942, Lee was assigned to the United States Army Air Corp and rose to the rank of major. In 1944, he was assigned Wright-Patterson Airfield in Dayton, Ohio where he was Chief of Experimental Surgical Unit. Bert and the family were with Lee in Dayton. They subsequently moved to Lee’s last posting at Brooke Hospital Center (now San Antonio Military Medical Center) in San Antonio. At the conclusion of the war, Lee, Bert, and the kids moved to Houston, Texas. Bert would work at the Hermann Hospital for the remainder of her career. She died on December 7, 1993, from complications of Alzheimer’s disease.
Mystery Photos
Last week’s Mystery Photos were Adrian W. Gelb, M.B.Ch.B. and John P. Abenstein, M.D.

Adrian Gelb, M.B. Ch.B. earned his medical degree from the University of Cape Town, South Africa in 1972. After an internship at Groote Schuur Hospital in Cape Town, he was a surgical resident at Addington Hospital in Durban, South Africa for a year. He then moved to Bath, England and was a resident in anesthesiology for a single year before moving again, this time to the University of Western Ontario (now Western University) in London, Ontario. After completing his anesthesia residency training, he moved to Toronto for a year of Critical Care Medicine training. In 1979, Adrian moved to Rochester where he worked closely with Kai Rehder, Peter Southorn, and Paul Didier as a Mayo Clinic research fellow. His work during his one year at Mayo resulted in two publications, one in Lung (DOI: 10.1007/BF02713915) and the other in the British J of Anaesthesia. Adrian’s year in our department was the first year of training for Drs. Bob Chantigian, Steve Rettke, Mary Ellen Warner, and me.
Adrian returned to London, Ontario in 1980, progressing and becoming chair of the University of Western Ontario’s department from 1991 through 2004. His academic career skyrocketed while at Western as he earned professor rank in Anesthesiology, Clinical Neurological Science, Pharmacology & Toxicology, Kinesiology, and Clinical Pharmacology. In 2004, he moved to the U.S. west coast and joined the Department of Anesthesiology at the University of California, San Fransisco. He remains there today as Professor of Anesthesiology.
A remarkable visionary, Adrian has served as president of the Society of Neurosurgical Anesthesiology and Critical Care (SNACC; 1995), the International Society for Anesthetic Pharmacology (ISAP; 2003); and the World Federation of Societies of Anaesthesiologists (WFSA; 2020). He also has been chair of the Board of Trustees of the International Anesthesia Research Society (IARS; 2003). In the science of anesthesiology, he has served on the editorial boards of the Journal of Neurosurgical Anesthesiology, the Chinese Journal of Anesthesiology, the Canadian Journal of Anesthesia, Anesthesia & Analgesia, Current Opinions in Anesthesiology, the Korean Journal of Anesthesiology, the Romanian Journal of Anesthesiology, the Brazilian Journal of Anesthesia, and the Journal of Neuroanesthesiology and Critical Care of India. Truth is, Adrian rarely sleeps and with his extensive travels, I suspect his world clock is wound pretty tightly.
With all of his international activities, Adrian has taken a worldwide lead on global health and, specifically, anesthesia patient safety. He has chaired the Patient Safety and Quality Committee of the WFSA and was the leader of the development of “the World Health Organization-WFSA International Standards for a Safe Practice of Anesthesia.” In recognition of his passion and enduring contributions to improving anesthesia care worldwide, the ASA will bestow its Nicholas M. Greene, M.D. Award for Outstanding Humanitarian Contribution on Adrian at its October 2024 Annual Meeting in Philadelphia.

John P. (JP) Abenstein, M.D. was raised in Chicago and graduated in 1976 from Duke University. He subsequently earned his MSEE (Electrical and Computer Engineering) from the University of Wisconsin. His engineering knowledge has played a major role in his career as he has become one of the country’s leading authorities in health care technology. He obtained his medical degree at the Loyola University & Stritch School of Medicine, then served as a resident in anesthesiology and a fellow in cardiovascular anesthesiology at Michael Reese Hospital, all in Chicago. JP then entered the U.S. Navy, with his primary assignment to the U.S. Naval Hospital in Oakland, California. During his military experience, he served in 1986 on the U.S.S. Tarawa on the Surgical Team 9 team.
JP moved to Rochester in 1988 and joined our staff. For the majority of his career, he was a stalwart member of our Division of Cardiothoracic Anesthesiology. He has been the institution’s leading advocate for perioperative monitoring and integrated clinical systems for his entire Mayo career. As a member of the Mayo’s Clinical Practice Committee in Rochester, he served as chair of its Computer, Equipment, and Products Subcommittee and also its Information Technology Prioritization and Review Committee. For the institution, he has been a long-time member of Mayo Integrated Clinical Systems. In that role, he has chaired the Electronic Environment and Workstation Oversight Group, the Technology Oversight Group, the Admissions/Re-admissions Remote Patient Monitoring Group, and the PICIS Project Group. Within our department, he has led the Anesthesia Electronic Medical Record Steering Group and been our authority on equipment/technology/monitoring since he first arrived.
Outside of Mayo Clinic, JP has been a leader within Minnesota and nationally. He has been president of the Minnesota Society of Anesthesiologists. For the state of Minnesota, he has been appointed by various governors to serve on healthcare committees such as the Medical Education and Research Costs Committee, the Healthcare Technology Committee, and the Blue Cross Blue Shield Medical Policy Committee. He chaired the former two committees. In 2002, JP earned certification as a parliamentarian. This certification served him well as he became Vice Speaker and then Speaker of the ASA House of Delegates, roles he held for more than a decade. In 2014, JP was elected as President of the ASA.
JP has influenced many national healthcare technology policies and practices. For example, JP and our own Dr. Brad Narr wrote an editorial in which they advocated in Anesthesiology for the expansion of monitoring during the postoperative period. This editorial has been used by many anesthesia leaders in facilities across the nation as they have advocated locally for expanded bedside monitoring. JP’s opinion on the Bispectral Index System (BIS) monitoring persuasively argued against the cost-effectiveness of BIS monitoring and impacted its use nationally. He has become a leading and highly respected authority on healthcare technology in the U.S..
JP and his wife, Sandy, live in Oronoco. They have two children. He continues to work clinically, assigned primarily to the Eisenberg (Rochester Methodist Hospital) and Gonda Building practices.
Mystery Photo Contest Winner

Last week’s contest winner was Terry Egbers.
Here are this week’s Mystery Photos. Reminder: We are now featuring two individuals each week for the Updates. To be placed into the Mystery Photo Starbucks contest, you will need to correctly guess at least one of the featured individuals. If you identify both of them, you will double your chances of having your name drawn.
Please email your response at warner.mark@mayo.edu within 3 days of this update. I will also need your name and contact information. All correct responses will be placed into a Monday morning drawing for a $10 Starbucks card. Only one winner per individual over the 80 weeks of Mystery Photos. If you win a weekly drawing, however, please keep submitting your responses. An overall winner (with the most correct responses in the series of 80 Updates) will receive a $100 Starbucks card.

Photograph: Department group photograph, 2016.
The Mayo Clinic Department of Anesthesiology Centennial Project: Halfway Through the 18 Months of Celebration
Please note that today’s Update is #40, halfway through the 80 weekly Updates that will be part of the department’s Centennial Project. During the first 40 Updates, we have learned about major contributions of our department to the development of perioperative care and the specialty in general. In recap of the first 40 Updates, the following timeline showcases those unique contributions that we’ve presented thus far. Many more will be added by the end of our Centennial Project in April 2025.
Each and every one of these contributions is an amazing achievement. To have them listed together risks any one of them of them and its value to the specialty being under-appreciated. We are blessed to have such a remarkable history in the department.
1904: Alice Magaw publishes a series of 14,000 anesthetics without an intraoperative death, a remarkable and almost unfathomable achievement at that time.

1920: Gaston Labat joins Mayo Clinic and becomes the country’s leading advocate for the use of regional anesthesia and a founder of the original American Society of Regional Anesthesia.

1925: John Lundy develops the Mayo Clinic’s Section on Anatomy, using dissections to teach regional anesthesia techniques.
1926: Lundy coins the term “balanced anesthesia” and advocates for its use.
1929: Lundy pulls together 15 leading academic anesthesiologists from the U.S. and Canada; the Anesthetists’ Travel Club is formed.
1933: Lundy establishes the Mayo Clinic’s intravenous fluid, blood, and medication service.

1934: Lundy and Charlie Adams publish on cold storage of citrated blood; the nation’s first blood bank is established.
1935: Lundy reports the successful trial of sodium pentothal and advocates for its use; it becomes the leading anesthetic induction agent for more than 5 decades.
1935: Lundy and Charlie Adams promote a hemoglobin transfusion trigger of 10 mg/dl; although debatable, this value stands the test of time for more than the next half century.
1938: Lundy plays a leading role in founding the American Board of Anesthesiology, a sub-board of the American Board of Surgery at its founding.
1940: Lundy is the country’s leading advocate for the successful establishment of a Section on Anesthesia within the American Medical Association.
1942: Lundy starts the Mayo Clinic’s first post-anesthetic care unit (PACU) and advocates for PACU development across the U.S. and Canada.
1942: Lundy starts one of the nation’s “90-Day Wonders” training courses for new physicians to learn anesthesia during WWII.
1944: Ed Tuohy introduces the epidural catheter technique.

1948: Florence McQuillen, the Mayo Clinic supervisor of nurse anesthetists, joins the AANA and serves 22 years as the association’s executive director.

1950: David Massa produces the world’s first intravenous catheter, an innovation considered to be one of the greatest advances in medicine in the 20th century.

1955: Bob Patrick, Albert Faulconer, and Emerson Moffitt are part of the Mayo Clinic team that perfect the Mayo-Gibbons heart-lung machine and advance cardiac surgery.
1967: Kai Rehder discovers the metabolism of halothane and its connection to halothane hepatitis.

1968: John (Jack) Michenfelder coins the subspecialty name, “neuroanesthesia,” and leads advances in the field.

1972: Sait Tarhan describes the risks of perioperative myocardial infarction (MI) and advocates for 6 months between MI and general anesthesia for elective procedures.

1973: Gerry Gronert discovers the association between succinylcholine and hyperkalemia when used in patients who have burns, disuse atrophy, and neurologic disorders.

1979: Joe Wang and Lee Nauss report on the first use of intrathecal narcotics.
1980: Gerry Gronert highlights triggers and treatment for malignant hyperthermia.

1985: Alan Sessler is a founder of the Foundation for Anesthesia Education and Research (FAER).

1985: John (Jack) Michenfelder is a founder of the Anesthesia Patient Safety Foundation (APSF).

1996: Roger White gets defibrillators into the vehicles of first responders, leading to Rochester having the world’s best survival results of ventricular fibrillation/cardiac arrest at that time.
1998: Denise Wedel and Terre Horlocker lead the development of guidelines on the use of anticoagulants in patients receiving regional anesthetics.
There are many other remarkable advances associated with our Department of Anesthesiology. In the next 10 months we will highlight these and they will be added to this current list. In addition, we will report on many more of our outstanding colleagues who have made significant, positive impacts on Mayo Clinic, the department, anesthesia and perioperative care, patient safety, and the specialty.
For now, halfway through our centennial celebration, congratulations to:
- The more than 3,500 alumni of our department’s anesthesiology, nurse anesthesia, and respiratory care training programs
- Our more than 2,100 current department members across the institution, and
- The 500 unique individuals who hold academic rank in anesthesiology at this time.
Mystery Photos
Last week’s Mystery Photos were Terrence L. Trentman, M.D. and Frank J. Villamaria, M.D.

Terrence (Terry) L. Trentman, M.D. was born in San Diego, California in 1962. He obtained his undergraduate degree from Brigham Young University and earned his M.D. degree in 1990 from Tulane University in New Orleans. During medical school he participated in the U.S. Air Force’s Health Professions Scholarship Program. From 1990-1995 he and his young family lived in Rochester, MN where he completed an internship, Anesthesiology residency, and pain fellowship. He and Dr. Gil Wong were the first 2 pain fellows in our newly accredited pain fellowship. After completion of his training, Terry and his family returned to the South to fulfill his Air Force payback commitment. He was stationed at Keesler USAF Medical Center, Biloxi, Mississippi for 3 years.
In 1998, Terry joined the staff of Mayo Clinic Arizona. In the subsequent years, he served in various clinical and administrative roles. Among others, he worked part-time in the chronic Pain Clinic, was a member of the Anesthesiology liver transplant team for 20 years and helped to bring ultrasound-guided regional anesthesia to MCA. He served as Division Chair of Pain Medicine, Medical Director of Surgical Services, Department Vice Chair for 10 years under Dr. Dan Cole, and Department Chair for an additional 9 years. Simultaneously, he also served as our institution-wide Anesthesiology Specialty Council Chair, was Vice-Chair of the Mayo Clinic Arizona Personnel Committee, and was promoted to professor rank in 2017.
Since rotating out as Department Chair in 2022, he has continued to work in the operating room but also increased his time in the Preoperative Evaluation Clinic. He currently serves as the Mayo Clinic Arizona Medical Director of Leadership Development and Chair of the Mayo Clinic Medication Diversion Prevention Subcommittee, following in the footsteps of our own Drs. Halena Gazelka and Keith Berge. He and his wife, Laralee, have 4 children and 7 grandchildren.

Frank J. Villamaria, M.D. was born in Frontenac, Kansas (far southeast Kansas) in 1955. He attended undergraduate school at Pittsburg State University in Pittsburg, Kansas. After completing medical school and a surgical internship at the University of Kansas, he was commissioned into the US Navy and attended flight surgery training in Pensacola, Florida. His first assignment was with the First Marine Air Wing in Okinawa, Japan. From there he deployed to multiple islands in the Pacific as well as to South Korea, the Philippines, and Australia. After completing a second tour of duty at the Navy’s Jet Training Command in Kingsville, Texas he moved to Rochester in 1984 as a resident in anesthesiology. He graduated in 1986 and stayed on another year as a cardiac anesthesiology fellow with his good friend, the late Dr. Bill Oliver.
Frank joined our staff in Rochester in 1987. In 1989 he moved to Temple, Texas where he joined the Scott & White Clinic (now Baylor Scott & White Health). He has spent his career at Scott & White, rising to the highest levels of leadership in the organization. He has held multiple positions in the Department of Anesthesiology, including chief of cardiac anesthesia, department vice-chair, and department chair. He has served in many positions at the institutional level, including being a member of the Scott & White Clinic Board of Directors and the medical director for quality and safety. He is currently Clinical Professor of Anesthesiology in the Baylor College of Medicine and vice-chair of anesthesiology for the Baylor Scott & White central Texas region. Like so many other large health systems, Scott & White Clinic merged with a large health system. The chosen partner was the Baylor Health System, resulting in a renewed organizational structure as Baylor Scott & White Health. It is the largest healthcare network in Texas.
Always a leader, Frank was very involved in the Texas Medical Association from 2008-2016, serving as a member of Council of Scientific Affairs and later serving as the inaugural chair of its Council on Healthcare Quality.
While at Mayo Clinic and Scott & White Clinic, Frank remained active in the U.S. Naval Reserve. He was recalled to active duty during Operation Desert Storm. While his children were young during the late 1990’s and early 2000’s, Frank transitioned to an inactive reserve status. However, he returned to the Active Reserve in 2014 once the kids had moved from home, retiring from the Navy as a Captain with over 30 years of service in May 2022. Throughout his service in the Navy, Frank retained both roles as an anesthesiologist and a Naval flight surgeon. He especially enjoyed his assignments as a flight surgeon because it allowed him to be assigned to Navy and Marine Corps Flight Squadrons and interact closely with pilots and aircrew. His duties sent him to many places worldwide and gave him the opportunity to fly in multiple military aircraft.
Frank and his wife, Maureen, married while he was a resident at Mayo. They met in Washington, DC during his Mayo Clinic-sponsored pediatric anesthesia rotation at D.C. Children's Hospital. Frank and Maureen have five children, three of whom are physicians. Emma is beginning her first year in dermatology residency at Mayo Clinic in Rochester next month. Charlie and Luke, in anesthesiology and orthopedic surgery residencies respectively, will serve as U.S. Air Force physicians on completing their training. Their other two girls, Maggie and Sara, are thriving in business in Austin, Texas. Frank and Maureen reside on a small farm outside of Belton, Texas.
Mystery Photo Contest Winner

Here are this week’s Mystery Photos. Reminder: We are now featuring two individuals each week for the Updates. To be placed into the Mystery Photo Starbucks contest, you will need to correctly guess at least one of the featured individuals. If you identify both of them, you will double your chances of having your name drawn.
Please email your response at warner.mark@mayo.edu within 3 days of this update. I will also need your name and contact information. All correct responses will be placed into a Monday morning drawing for a $10 Starbucks card. Only one winner per individual over the 80 weeks of Mystery Photos. If you win a weekly drawing, however, please keep submitting your responses. An overall winner (with the most correct responses in the series of 80 Updates) will receive a $100 Starbucks card.

Photograph: Virginia B. Hartridge, M.D., undated
The Mayo Clinic Department of Anesthesiology: Educators Internally, Leaders in Education Everywhere
The Department of Anesthesiology has played a major role within the institution in the Education Shield as well as in extramural education societies, on anesthesia-related boards, and in education regulatory organizations. In the next four Updates, I will describe the history and development of our department’s education programs and the contributions of our department members to institutional and national leadership in anesthesia and respiratory care education. Specifically,
- This week we will highlight the Rochester education programs in nurse anesthesia and respiratory care.
- In the coming week we will focus on the LaCrosse, Wisconsin nurse anesthesia program and the anesthesiology residency and fellowship programs in Florida and Arizona.
- In the third week we will describe the Rochester anesthesiology residency and fellowship programs.
- In the final week we will showcase department members who have played major education leadership roles within in the institution and nationally.
Nurse Anesthesia in Rochester
Edith Graham, soon to be Mrs. Charlie Mayo, trained good friend Alice Magaw in 1893 to deliver anesthesia. Alice subsequently trained 20 nurses, including colleague Florence Henderson, over two decades. These nurse anesthetists would provide anesthesia for the great majority of patients early in the institution’s first 35 years. Most of these nurses were trained “on the job.” As the field of anesthesiology evolved in the 1920s and 1930s, physicians such as Dr. John Lundy and nurse anesthetists such as Florence McQuillen advanced the training for nurses and developed a didactic curriculum. Florence would go on to become the first executive director of the American Association of Nurse Anesthetists and play a major role in developing training and certification standards for nurse anesthetists.
Dr. Lundy was the first director of the nurse anesthesia training program in his role as chair of the Section on Regional Anesthesia (and subsequent department designations). In 1940, he designated Dr. R. Charles (Charlie) Adams as the program director. Charles worked closely with Florence McQuillen to solidify the training program and curriculum for nurse anesthetists. Nearly all of the anesthesiologists in the 1940s participated in classroom instruction and nurses in training attended seminars and conferences given by the residents. Dr. Adams was followed in the director role over the subsequent 15 years by Drs. Harry (Tom) Seldon, John Osborn, Roger Ridley, and John Paulson.
The program blossomed in 1956 when Dr. Virginia Hartridge was appointed as education director. She organized a comprehensive curriculum and ensured that all trainees attended seminars and classes. Most importantly, in 1957 she recruited Robert (Bob) Johnson, CRNA to assist in providing nurse anesthesia education. After several years of building a more complete training program, Virginia and Bob formed a Nurse Anesthesia Education Committee in 1964. By 1970, Bob had been appointed as the nurse anesthetist director of the program. The dynamic duo of Virginia and Bob led the program together until 1974.
Here is a list of the outstanding anesthesiologists and nurse anesthetists who have served as medical and education directors of the nurse anesthesia training program since 1970:
- Medical Directors

1956-1974: Dr. Virginia Hartridge

1974-1984: Dr. Donald R. Krabill
1984-1987: Dr. Lawrence B. Perry
1987-1991: Dr. Robert L. Lennon

1991-Present: Dr. Beth A. Elliott
- Education Directors

1970-1988: Robert Johnson, CRNA
1988-1997: Edward Thompson, CRNA, MS

1997-2020: Mary Mariena, CRNA, PhD

2020-Present: Erin Martin, CRNA
Respiratory Care
The department’s current Respiratory Care program started in 1972 as the Inhalation Therapy program. It was proposed by Drs. Paul Didier, Alan Sessler, Frederic Helmholz, Ken Makinen, and Gerald Needham. They advocated for an associate degree program sponsored by the Rochester Junior College. The proposal received funding through a Minnesota education grant. The first class entered the two-year program in 1972. In 1975, the program received initial accreditation by the American Medical Association’s Council on Medical Education and Joint Review Committee for Respiratory Therapy Education. While most clinical rotations occurred in the Mayo-related hospitals in Rochester, an off-campus rotation at the Rochester State Hospital for airway management was arranged from 1972 through 1981 when the state hospital closed. Today, the state hospital campus is the site of the Federal Medical Center.
Upon accreditation, the program changed its name to the Respiratory Therapy Program. Key milestones in its development include increasing its scope of training in 1988 to include cardiovascular stress testing, pulmonary function testing, and participation in sleep medicine. In 1999, the program transitioned to a baccalaureate degree-granting program in partnership with the Mayo Clinic School of Health Sciences and the General College of the University of Minnesota. This relationship was further strengthened in 2011 when the University of Minnesota Rochester established its Bachelor of Science in Health Professions degree. Graduates who earn this degree also receive a certificate from the Mayo Clinic School of Health Sciences in Respiratory Care.
Leaders of the Respiratory Care Program include:
- Medical Directors

1972-1987: Dr. E. Paul Didier

1987-2003: Dr. David J. Plevak

2003-2021: Dr. James Y. Findlay

2021-Present: Dr. Brendan Wanta
- Education Directors

1972-1976: Bernard Gilles, CRNA, RRT

1976-2006: Jeffrey J. Ward, RRT

2006-2022: Vanessa L. King, RRT

2022-Present: Stephanie J. Holst, RRT
Mystery Photos:
Last week’s Mystery Photos were Harold Michael Marsh, M.D. and Bradly J. Narr, M.D.

- Michael (Mike) Marsh, M.D. was born in Australia on March 7, 1939. He graduated from the medical school at the University of Sydney in 1964. In doing so, he followed his grandfather (1912), his father (1936), and his uncle (1938) as alumni of that school. He subsequently trained in anesthesia at the medical school’s Royal Prince Alfred Hospital.
In 1968, Mike was advised by Dr. Tim Cartmill, a Mayo-trained Australian cardiac surgeon, to go to Rochester. He applied and received a Mayo scholarship to travel to Rochester and study Critical Care and Respiratory Care under the supervision of Dr. Alan Sessler. After arriving in 1969, he also met and worked closely with Drs. Kai Rehder and Paul Didier and Bernard Gilles CRNA and Myron Ricks CRNA. This team of newfound colleagues worked together clinically in the ICUs and also studied the effects of anesthesia, muscle relaxation, and gravity on pulmonary function and ventilation-perfusion matching during mechanical ventilation. The research program was directed by Kai, with collaboration from Drs. Ward Fowler, Fred Helmholtz, and Robert Hyatt.
Mike returned to Sydney in 1972 after a 6-month fellowship in cardiac anesthesia at Toronto’s Western Hospital, using that fellowship to accumulate enough money to pay for his return trip home. The Mayo scholarship that supported his travel to Rochester did not provide funding for a return ticket. Sounds like a good recruitment process, doesn’t it?
Upon his return to Sydney, he was made director of intensive care and charged to establish a general ICU. Building, equipping and staffing a 5-bed unit for this 1,000 bed-hospital took him eighteen months. During that time, he provided consultative services to all patients requiring intubation and mechanical ventilation for respiratory failure. These patients were being cared for on open wards by non-specialized nursing personnel. During that ICU’s first 18 month period using a Mayo-style practice, the 30 day mortality rate for its patients was reduced by 50%.
Mike returned to Rochester and Mayo Clinic in 1974. Dr. Dick Theye invited him to join Alan Sessler, Paul Didier, and colleagues in the ICUs. During the next 15 years his activities at Mayo included a mixture of clinical practice, research, education and administrative roles. While at Mayo, Mike became an oral examiner for the ABA, was very involved in a number of national societies, and developed our ACGME-approved anesthesiology fellowship in critical care medicine. He was the program’s first director.
In 1989 Mike was recruited to Detroit, Michigan’s Henry Ford Health System as chair of the system’s Department of Anesthesiology. His primary task was to apply for ACGME approval for renewal of the institution’s residency program. The previous program had ceased in 1975 and his work entailed starting a research program and developing educational experiences in critical care and pain medicine. For the research program, he started by recruiting our own Russell Van Dyke, Ph.D. The Henry Ford residency program was approved in 1990 and has continued from that time. To this day Mike still provides a half-day teaching session for the program’s residents at each level of training. During all of this, Mike became president of the Wayne County Medical Society and a board director in the Michigan State Medical Society. He also served on the Michigan State medical Board for several years., rising to President and from there to board Membership on the Michigan State Medical Society Board for several Years.
In 1998 Mike transitioned to chair of the Department of Anesthesiology at Wayne State University. The challenge for him was to bring together disparate elements within the Detroit Medical Center, a loose amalgamation of hospitals and anesthesia practices, and revitalize another failed residency program. He supposedly retired in 2012 when our own Dr. Doug Bacon succeeded him. By the way, the program continues but struggles at Wayne State as Detroit Medical Center is now under the management of Venture Capital, a for-profit entity. Neither Mike nor Doug are associated with Wayne State any longer.
In fact, Mike did not retire in 2012. Instead, at Doug’s request, they moved together to St Joseph Mercy Hospital, Oakland in Pontiac, Michigan. Here they started another residency training program, now Mike’s third in Detroit. He served as the new program’s director for a period before stepping down. He worked clinically part-time, primarily at St. Joseph Mercy Hospital, until November 23, 2023, completing a full 60 years of clinical practice and leadership.
Mike’s beloved wife, Eleanor passed away several years ago. They had three children. Now at age 85 years, Mike enjoys watching his five grandchildren as they make their way to their future and meaningful careers and lives.
In Mike’s own words, “Being allowed to practice Medicine in any community is a profound privilege. It places one in a sacred position of trust with intimate access to the lives and confidences of other individuals. The Mayo philosophy and culture places emphasis on honesty, integrity, respect and accountability in serving the best interests of one’s patients, through practice, research and education. It was my great privilege to be accepted to train for two years at Mayo Rochester and then to be invited to return to serve as a Consultant in Anesthesiology and Critical Care Medicine for a further fifteen years in my mid-career.”

Bradly J. Narr, M.D. was born July 26, 1954 in Neosho, Missouri while his father was in the U.S. Army. By the time he was 6 months old, the family had moved to Minnesota where he was raised and educated. He earned his Bachelor of Science degree in Biochemistry at the University of Minnesota before completing medical school at the same institution in 1980. He came to train at the world-famous Mayo Clinic in Internal Medicine (1980-83) before switching career trajectories in 1983, chiefly because his YMCA basketball friends raved about their respective careers in Anesthesiology. After Dr. Alan Sessler took him to breakfast in the Methodist Hospital Cafeteria in 1985, Brad was invited to join the Anesthesiology consulting staff where, for the first part of his career, he divided his clinical responsibilities between critical care and the operating theaters.
Brad rose to positions of leadership within the department and at Mayo, holding the Department of Anesthesiology chair role for 11 ½ years as well as serving as the vice-chair and chair of the Surgical and Procedural Committee between 2007 and 2021. He is the only non-surgeon to chair this crucial Mayo committee. Brad was also the first medical director of the 10-1 ICU at Methodist Hospital and the first medical director of the 7 MB DE ICUs at St. Mary’s Hospital, both units envisioned and built under his direction. He also pioneered the creation of the Department of Anesthesiology Preoperative Evaluation Clinic which opened its doors in 1996.
Within Mayo Clinic but outside the department, Brad has a distinguished career. While serving as a member of Mayo Clinic’s Executive Operations Team, Mayo President and Chief Executive Officer Dr. John Noseworthy tasked Brad with solidifying Mayo Clinic’s US News and World Report #1 ranking . . . a remarkably successful and satisfying mission for Brad that led to more than a decade of the institution holding the top spot before the magazine switched its operational definitions and stopped awarding #1 positions. Brad also led key efforts within Mayo Clinic, in the city of Rochester, and in the Minnesota Legislature to designate Mayo Clinic/Rochester as a Destination Medical Center in the state of Minnesota. This designation will ultimately bring nearly $600 million of state investment into Rochester’s infrastructure needs as the Destination Medical Center’s $5 billion, 20-year plan and the city’s growth during that period come to fruition.
As he starts his 40th year as a consulting staff at Mayo, Brad continues to practice in the Preoperative Evaluation Clinic that he helped establish. His Internal Medicine and ICU backgrounds, coupled with his intimate knowledge of the Mayo surgical and procedural practice, help to facilitate patient access to the best surgical, procedural, and anesthetic care available anywhere in the world. He recently was elected as a board member of the Anesthesia Foundation (The Anesthesia Foundation® – Helping Anesthesiologists Succeed).
Brad and his wife, Terry, have 4 sons and many grandchildren, all in MN. He subscribes to the William Mayo quote; “there is no fun like work,” but his joy in life also revolves around his family. He is an amazing physician and colleague.
Mystery Photo Contest Winner
Last week’s contest winner was Mindy Woodward.

This Week's Mystery Photos:
Reminder: We are now featuring two individuals each week for the Updates. To be placed into the Mystery Photo Starbucks contest, you will need to correctly guess at least one of the featured individuals. If you identify both of them, you will double your chances of having your name drawn.
Please email your response at warner.mark@mayo.edu within 3 days of this update. I will also need your name and contact information. All correct responses will be placed into a Monday morning drawing for a $10 Starbucks card. Only one winner per individual over the 80 weeks of Mystery Photos. If you win a weekly drawing, however, please keep submitting your responses. An overall winner (with the most correct responses in the series of 80 Updates) will receive a $100 Starbucks card.
Photograph: Thomas J. Grau, M.D., undated
The Mayo Clinic Department of Anesthesiology: Educators Internally, Leaders in Education Everywhere
The Department of Anesthesiology has played a major role within the institution in the Education Shield as well as in extramural education societies, on anesthesia-related boards, and in education regulatory organizations. In the next four Updates, I will describe the history and development of our department’s education programs and the contributions of our department members to institutional and national leadership in anesthesia and respiratory care education. Specifically,
- Last week we highlighted the Rochester education programs in nurse anesthesia and respiratory care.
- This week we will focus on the La Crosse, Wisconsin nurse anesthesia program and the anesthesiology residency and fellowship programs in Florida and Arizona.
- In the third week we will describe the Rochester anesthesiology residency and fellowship programs.
- In the final week we will showcase department members who have played major education leadership roles within in the institution and nationally.
The Department of Anesthesiology and Educational Programs: La Crosse Nurse Anesthesia Program and Florida and Arizona Residency and Fellowship Programs
Nurse Anesthesia in La Crosse, Wisconsin
The Franciscan Healthcare School of Anesthesia within the Mayo Clinic Health System currently has 40 students in its three-year training program. The program is affiliated with the University of Wisconsin-La Crosse and its Biology Program and the Viterbo University School of Nursing. Students receive much of their clinical training within the Mayo Clinic Health System, with the majority of that training in La Crosse but also in Eau Claire and Mankato. Students began going to the Mayo Clinic Health System site in Eau Claire in 2020 and in Mankato in 2022. Students may pursue subspecialty training (e.g., pediatric) in other specialty hospitals, primarily in Wisconsin. Upon completion of their training, graduates receive Master degrees in Biology from the University of Wisconsin – La Crosse and Doctor of Nurse Practice degrees from Viterbo University.
The School of Anesthesia was started by Franciscan Sister Yvonne Jenn in 1942 in response to a tremendous need for anesthesia providers in La Crosse and the surrounding areas of Wisconsin, Minnesota, and Iowa. From inception through 1987, the program was hospital-based within St. Francis Hospital. When the Council on Accreditation of Nurse Anesthesia Educational Programs required Master degrees for its graduates of nurse anesthesia schools in 1987, the St. Francis program aligned with the University of Wisconsin – La Crosse and added a Master degree in biology. In 2017, the Council of Accreditation further advanced degree requirements for educational program graduates and the school affiliated with Viterbo University and its School of Nursing to grant Doctor of Nurse Practice degrees.
To date, there have been 620 alumni of the La Crosse School of Nurse Anesthesia.
Here is a list of the outstanding anesthesiologists and nurse anesthetists who have served as medical and education directors of the nurse anesthesia program:
Medical Directors
- 1988 – 2014 Dr. Thomas J. Grau
- 2014 – 2017 Dr. Peter J. Schams

- 2017 – 2024 Drs. Peter J. Schams, John Merfeld, and Theodore W. Van Der Horst
- 2024 - present Drs. Theodore W. Van Der Horst and Jason Beckerman
Education Directors
- 1942 – 1981 Sister Yvonne Jenn, RN
- 1981 - 1982 John Garde, CRNA
- 1982 – 2017 Barbara Jochman, CRNA

- 2017 – present Jessica J. Peterson, CRNA, PhD

Mayo Clinic Florida: Residency and Fellowships
In 1988, our Rochester resident training program began rotating residents who wished to participate to Mayo Clinic in Florida (Jacksonville) as part of their overall 3-year anesthesia training. Dr. Mark Ereth was the first Rochester resident to rotate to Jacksonville. The relatively new Accreditation Council on Graduate Medical Education (ACGME) considered Mayo Clinic to have an integrated residency program between Rochester (home site), Jacksonville, and Scottsdale (Phoenix) from that time through 1997 and residents in Rochester would periodically rotate to both Jacksonville and Scottsdale. The ACGME changed its course in 1997 and the program was no longer considered to be integrated.
During the 1993 – 2000 period, our anesthesiologists in Jacksonville established a number of fellowship programs. The programs and their initial program directors were:
- 1993: Pain Medicine; Dr. Tim J. Lamer

- 1994: Pediatric Anesthesiology (at Wolfson Children’s Hospital); Dr. Stefanie F. Schrum

- 1994: Critical Care Medicine; Dr. Gavin D. Divertie

- 2000: Obstetric Anesthesiology; Dr. Chris F. James
- 2000: Cardiothoracic Anesthesiology; Dr. Monica Mordecai

- 2008: Regional Anesthesiology; Dr. Roy A. Greengrass

At this time, the active fellowships are Pain Medicine, Pediatric Anesthesiology, and Regional Anesthesiology.
In 2000, Dr. Marie L. DeRuyter started the application process to establish an independent Mayo Clinic Florida residency in anesthesiology. She was supported by our Jacksonville department chair, Dr. Michael J. (Mike) Murray. The program was accredited in 2002 and the first class of four residents was recruited and started in July 2003. Marie was the initial program director and remained in that role through 2013. At that time, Dr. Bruce J. Leone became program director through 2015. Since 2015, Dr. Beth L. Ladlie has served as our program director.
Since the first graduating class of residents in 2006, 77 anesthesiologists have completed their residency training in Jacksonville.
Mayo Clinic Arizona: Residency and Fellowships
As with our resident rotations in Jacksonville that started in 1988, residents began to go to our Scottsdale campus and other affiliated sites in Phoenix in 1989. Approximately 14-20 residents each year between 1990 and 2007 rotated from Rochester (and a few from Jacksonville in the latter part of that period) for clinical experiences in our Mayo Clinic sites in Scottsdale and Phoenix.
In 1998, our Arizona colleagues established a fellowship program in Pain Medicine. Dr. Jesse Muir was the program’s initial director. Program directors for the fellowship have included:
- 1998 – 2002 Dr. Jesse J. Muir
- 2002 -2013 Dr. David P. Seamans

- 2014 – 2019 Dr. John A. Freeman

- 2019-2023 Dr. Christopher S. Wie

- 2023 – present Dr. Jillian A. Maloney

In 2000, Dr. Renee E. Caswell started the application process to establish an independent Mayo Clinic Florida residency in anesthesiology. She was supported by our Arizona department chair, Dr. Daniel (Dan) J. Cole. The program was accredited in 2005 and the first class of three residents was recruited and started in July 2007. Dan was the initial program director and remained in that role through 2009. At that time, Renee became program director through 2016. She was succeeded by Dr. Andrew (Andy) Gorlin who served until 2022. Since 2022, Dr. Monica W. Harbell has served as our program director.
Since the first graduating class of residents in 2010, 42 anesthesiologists have completed their residency training in Phoenix.
Mystery Photos
Last week’s Mystery Photos were Harold Michael (Mike) J. Joyner, M.D. and Gurinder (Gary) M. Vasdev, M.D.

Michael (Mike) Joyner, M.D. was born in Lafayette, Louisiana in 1958 and was raised in Tucson, Arizona. He earned both his undergraduate and medical degrees from the University of Arizona. Mike was an outstanding member of the university’s track team as an undergraduate. During that time, he became involved in human physiology research. He continued this research during medical school, graduating from the University of Arizona College of Medicine in 1987.
Mike joined our Mayo Clinic Department of Anesthesiology in Rochester as a resident in 1987. His classmates included Maria DeCastro, Paul Stensrud, Mary Weber, Doug Dubbink, David Cook, Jeff Jax, and others. Maria and many others, including me, distinctly remember our surprise when Mike asked several complex questions of our visiting professor in July of Mike’s intern year. It was clear at that moment that Mike was going to have a unique and illustrious academic career.
Mike was motivated to be at Mayo Clinic in part by the opportunity to do both clinical training and work with Dr. John Shepherd, a noted physiologist in Rochester. Dr. Shepherd was the first dean of Mayo Medical School, a president of the American Heart Association, and a giant in blood pressure regulation. Mike earned his first NIH grant in 1992 while still a resident and joined our staff in 1993.
He has had many institutional roles on Mayo’s Research Committee, has been involved in leadership teams directing major center grants, and has run a large lab that has been continuously funded by the NIH since 1992. Mike now serves as the department’s Vice Chair for Research. He currently holds a prestigious NIH Outstanding Investigator R35 award. He also is one of the world’s most widely quoted anesthesiologists in the media.
More than 30 fellows have received training in the “Joyner Lab” and many of his Ph.D. fellows now direct independent research programs at major research universities. More than 100 undergraduate and medical students have spent time in his lab, including more than ten current staff members. He is a collegial and caring mentor and facilitator to an incredibly diverse group of mentees and colleagues.
Mike’s research group has made major contributions to our understanding of:
- How blood flow to muscle is regulated
- Sex differences and blood pressure
- Hypoxia
- The physiology of human athletic performance
In March of 2020, early in the COVID-19 pandemic, the US Government asked him to lead an expanded access program for convalescent plasma to treat COVID-19. Mike repurposed his research program and, with his collaborators from around the world, showed that convalescent plasma given early in the course of disease reduced mortality. As the pandemic progressed, he showed that it was especially useful in immunocompromised patients.
Mike and his wife, Teri, have two boys along with Mike’s two daughters.

Gurinder (Gary) Vasdev, M.D. was born in Nairobi, Kenya in 1962. He attended medical school in London at the Middlesex Hospital Medical School and earned his MBBS in 1985. The school is part of the University of London, England. Gary completed his general training in anaesthesia at Addenbrokes Hospital, Cambridge, England. He subsequently was awarded the Fellowship of the Royal College of Anaesthetists in both England and Ireland. It was at his graduation ceremony in Dublin in 1990 that Gary first met Dr. Alan Sessler who was bestowed an honorary fellowship at the same time. It truly is a small world!
With Alan’s encouragement, Gary moved to Rochester in 1991 as a fellow in obstetric anesthesiology. He completed that fellowship as well as a critical care fellowship. From 1993 through 1994, he served as a Mayo Clinic Special Clinical Fellow in liver transplant anesthesia.
After completing his advanced training in Rochester, Gary moved to Hartford, Connecticut and joined the University of Connecticut for a short period. He returned to Mayo Clinic in Rochester in March1995. In 1992, he received a Zuspan Award from the Society of Obstetric Anesthesia and Perinatology (SOAP). This award led to what was the beginning of his national rise in OB anesthesiology. In 2007, he became our first Mayo physician to be President of SOAP.
Gary has served our department as director of OB anesthesiology and various other committees. He currently is our department’s vice-chair for Diversity, Equity, and Inclusion. He continues to support Mayo Clinic's national exposure and will soon become President of the North American Sikh Doctors and Dentists Association (NASMDA). Gary has been instrumental in his outreach work with international anesthesiology societies as they develop CME education programs. He has been an advocate for helping his colleagues gain valuable presentation experiences internationally. Gary is a fun travel companion and has done much to bring people together both within our department and the institution.
Gary and his wife, Billie, an outstanding Rochester dentist, have 3 children. Amrit is an anesthesiology resident at Mayo Clinic in Rochester; Ranveer is a urology resident also here in Rochester; and Tanveer is a dental student at the University of Iowa.
Mystery Photo Contest Winner

Last week’s contest winner was David Seamans.
Here are this week’s Mystery Photos. Reminder: We are now featuring two individuals each week for the Updates. To be placed into the Mystery Photo Starbucks contest, you will need to correctly guess at least one of the featured individuals. If you identify both of them, you will double your chances of having your name drawn.
Please email your response at warner.mark@mayo.edu within 3 days of this update. I will also need your name and contact information. All correct responses will be placed into a Monday morning drawing for a $10 Starbucks card. Only one winner per individual over the 80 weeks of Mystery Photos. If you win a weekly drawing, however, please keep submitting your responses. An overall winner (with the most correct responses in the series of 80 Updates) will receive a $100 Starbucks card.

The Mayo Clinic Department of Anesthesiology: Educators Internally, Leaders in Education Everywhere
The Department of Anesthesiology has played a major role within the institution in the Education Shield as well as in extramural education societies, on anesthesia-related boards, and in education regulatory organizations. In this early summer series of four Updates, I will describe the history and development of our department’s education programs and the contributions of our department members to institutional and national leadership in anesthesia and respiratory care education. Specifically,
- In the initial week we highlighted the Rochester education programs in nurse anesthesia and respiratory care.
- This past week we focused on the LaCrosse, Wisconsin nurse anesthesia program and the anesthesiology residency and fellowship programs in Florida and Arizona.
- This third week we will describe the Rochester anesthesiology residency and fellowship programs.
- In the final week we will showcase department members who have played major education leadership roles within the institution and nationally.
The Department of Anesthesiology and Educational Programs: The Residency and Fellowship Programs in Rochester
Mayo Clinic was one of the first U.S. medical centers to have a residency program in anesthesiology. Although “informal” anesthesia training of young physicians occurred at Mayo Clinic before 1924 (e.g., Drs. Gaston Labat and Bill Meeker trained surgical residents in the use of regional anesthesia in the early 1920s), it wasn’t until the arrival of Dr. John Lundy in 1924 that an effort was started to introduce a formal education program in anesthesiology for physicians. Dr. Charles F. McCuskey began his training in 1925 and was the first to complete his anesthesia training in Dr. Lundy’s new program.
An interesting scenario occurred in 1926 when Dr. Ralph Waters moved from his private practice of primarily anesthesia in Sioux City, Iowa to Madison, Wisconsin to establish in 1927 at the University of Wisconsin what was to become known as the country’s first official residency program in anesthesia. As part of Dr. Waters’ 1926 move, he stopped in Rochester for 3 months to work as an assistant with Dr. Lundy and learn regional anesthesia. While in Rochester, he was enrolled in the nascent Mayo Clinic School of Graduate Medical Education and was graded by Dr. Lundy for his 3 months of efforts. His grade card is still retained by the school.
By the late 1920s, Dr. Lundy developed a 3-year training curriculum in anesthesia that included 15 months of experience in clinical anesthesia, 3 months in anatomy, and 18 months in research. Although never fully implemented and the idea of 3 years of training in anesthesia did not become the norm in the specialty until 1985, many of the program’s early trainees did, indeed, spend 3 years in training. Eleven of the 24 residents from 1925 through 1941 earned Master of Science degrees from the University of Minnesota.
Program directors for the more than 850 anesthesiologists who have completed their residency training in Rochester since 1925 include:
- 1924-1953: John S. Lundy, M.D.
- 1953-1959: Robert T. Patrick, M.D.
- 1959-1966: John T. (Tom) Martin, M.D.
- 1966-1976: Alan D. Sessler, M.D.
- 1976-1991: Ronald J. Faust, M.D.
- 1991-1994: Leslie N. Milde, M.D.
- 1994-2007: Steven, H. Rose, M.D.
- 2007-2023: Timothy R. Long, M.D.
- 2023-present: Bridget P. Pulos, M.D.
Subspecialty Fellowships.
As the specialty expanded dramatically in the 1970s and 1980s and anesthesiologists began to subspecialize, the need for advanced training in the subspecialties arose. Fellowships (post-residency education programs) gained popularity. Many of these fellowships were clinically-oriented, but others were primarily focused on research. In general, these fellowships were uniquely designed to match the needs of the individual fellows. There were no strong guidelines or regulations that determined the content of these self-determined fellowships.
Prior to 1981 and the creation of the Accreditation Council for Graduate Medical Education (ACGME), there was no regulatory oversight of graduate medical fellowships. As these subspecialty fellowships and the subspecialty fields themselves matured, subspecialty societies began to recommend the curriculums and experiences that fellows should expect in their training. Standardization of fellowships began to grow. With standardized subspecialty fellowships ensuring full spectrums of subspecialty training, the American Board of Anesthesiology felt more confident in the consistency of the training programs and began to certify anesthesiologists in the subspecialties. The first of these was Critical Care Medicine in 1986. Pain Medicine certification started in 1993, followed by Pediatric Anesthesiology in 2013 and Adult Cardiothoracic Anesthesiology in 2023.
At this time, it is not clear when our department began to have fellowships in the various subspecialties. It is clear that the department had unaccredited subspecialty fellowships prior to 1981. It also is clear that many unaccredited subspecialty fellowships continued after ACGME accreditation became available. This discrepancy began to change in 2005 when Drs. Mark Warner and Steve Rose, in their roles as the leaders of the Mayo Clinic School of Graduate Medical Education, began to require that all graduate medical education fellowships that were accreditable by the ACGME must become accredited.
Over the years, there have been nine subspecialties with fellowships in the Rochester department. Of these, all but a fellowship in Transplant Anesthesiology continues. After an extensive search of the Mayo Clinic School of Graduate Medical Education, paperwork available within the department, and recollections of senior staff members and individuals who were fellows, I believe that the “official” start dates and the initial program directors for each of the accredited fellowships and the Transplant fellowship include:
- 1989: Critical Care Medicine in Anesthesiology; Dr. David J. Plevak
- 1993: Pain Medicine; Dr. Joseph M. Messick, Jr.
- 1994: Transplant Anesthesiology; Dr. Steven H. Rose
- 2004: Pediatric Anesthesiology; Dr. Randall Flick
- 2007: Adult Cardiothoracic Anesthesiology; Dr. David J. Cook
- 2013: Clinical Informatics; Dr. Brian W. Pickering
- 2015: Neuroanesthesiology; Dr. Jeffrey J. Pasternak
- 2017: Regional Anesthesiology; Dr. Adam D. Niesen
- 2018: Obstetric Anesthesiology; Dr. Katherine W. Arendt
In the coming year, we will collect complete data on who led our fellowships and who trained in them . . . in all of our Mayo Clinic sites. The collection of this information will take extensive reviews of department minutes, Mayo Clinic records, and visits with individuals who were involved in the subspecialty fellowship programs. Once collected, the information will be displayed in our department history repository, Anesthesiology Department | Mayo Clinic | History and Heritage. The wonder of the site is that corrections and modifications may be easily made. Please contact me if you have any errors that you identify.
Summary of the Rochester Residency and Fellowship Programs
At the end of June this year, the Rochester residency and fellowship programs will have graduated nearly 1,100 anesthesiologists. Eight-five of these graduates have become academic department chairs in the U.S. and outside the country, creating a strong link between Mayo Clinic and the development of the specialty around the world. In addition, the Rochester residency and fellowship programs have produced former trainees who have play major specialty leadership roles during their careers. These roles have included:
- Nine presidents of the American Society of Anesthesiologists
- Eleven presidents of the American Board of Anesthesiology
- Seven chairs of the Board of Trustees of the International Anesthesia Research Society
- Presidents of the three primary ASA foundations (Foundation for Anesthesia Education and Research, Anesthesia Patient Safety Foundation, and Wood Library Museum of Anesthesiology)
- Presidents of six of the eight primary subspecialty societies in the U.S.
- One president of the American Association of Nurse Anesthetists
- One executive director of the American Association of Nurse Anesthetists
Mystery Photos
Last week’s Mystery Photos were Robert T. Patrick, M.D. and Mary Ellen Warner, M.D.

Robert (Bob) T. Patrick, M.D. is from Des Moines, Iowa and was born on August 29, 1920. After graduating from Denison University in Granville, Ohio, he attended medical school at the University of Louisville, Kentucky, earning his M.D. in 1944. After a two year period in the U.S. Navy, he entered private practice in Norwalk, Ohio. By 1949, he decided to become a resident in anesthesiology. He came to Mayo Clinic and completed his training, joining the Mayo staff in 1952. While a fresh new consultant in Rochester, he was recalled to the Navy and spent much of 1953 and 1954 back in the service. He returned to Mayo Clinic in late 1954 and stayed until 1961 before leaving to a private practice in Casper, Wyoming. While in Wyoming, he was a member of the state’s medical board. He also became one of the few private practitioners at that time to be asked to serve as a director of the American Board of Anesthesiologists. He was a director of the ABA from 1967 through 1975, including a year as president of the ABA in 1971. More about his career may be found in a 1972 article in the Denison University Alumni Newsletter in which he was recognized by citation.
While at Mayo Clinic for 9 years, he had many remarkable achievements:
- Development of a Cardiopulmonary Bypass Machine. Team member of the Mayo cardiac innovators who tested and developed extracorporeal circulation, the “Mayo-Gibbons heart-lung machine.” Other team members included giants in medicine and physiology such as Drs. John Kirklan (cardiac surgery), Earl Wood and Jeremy Swan (physiology), James DuShane (pediatrics); and Richard Jones (biomedical engineering). An outstanding summary of the development of cardiopulmonary bypass and the first 50 years of cardiac surgery at Mayo Clinic was published in 2005 in Mayo Clinic Proceedings.
- Initial Clinical Trials of Cardiopulmonary Bypass. The primary Mayo Clinic anesthesiologist during the early clinical trials of cardiopulmonary bypass. Dr. Patrick provided the anesthetic care for the first 40 patients to undergo intracardiac surgery from March 22, 1955 through January 1956. This initial trial established the protocols used today for cardiopulmonary bypass and cardiac surgical volumes skyrocketed. The anesthesiologists involved in the team increased with the addition of Drs. Richard Theye, Robert Devloo, and Emerson Moffitt. An excellent story about one of the first children to undergo intracardiac surgery at Mayo Clinic (and in the world) may be found in Smithsonian Magazine at This 1950s Heart-Lung Machine Revolutionized Cardiac Surgery | Smithsonian (smithsonianmag.com).
- Building our Residency Training Program. Dr. Lundy implicitly trusted Dr. Patrick and handed over the role of residency program director to him in 1953. As noted above, he served in this role through 1959.
Dr. Patrick and his wife, Dorothy Ann, had six children. He passed away on August 30, 1999.

Mary Ellen Warner, M.D. was born in Chillicothe, Ohio on May 29, 1954. After graduating from the University of Florida in 1975, she entered the Medical College of Ohio (now the University of Toledo). While there, she met and married fellow classmate, Dr. Mark A. Warner. While at the Medical College of Ohio, they were mentored by Dr. John T. (Tom) Martin, former division chair and residency program director at Mayo Clinic and the chair of the Department of Anesthesiology at the medical college. Dr. Martin arranged for both Mary Ellen and Mark to be award medical student preceptorships from the American Society of Anesthesiologists. At Dr. Martin’s encouragement, they spent their preceptorships in Rochester. They were supervised by Drs. Duane Rorie and Alan Sessler. While there, they established great friendships with staff (e.g., Drs. Ron Faust, Jim Prentice, Bob Devloo, Paul Didier, Mike Marsh, and Matt Divertie) and residents (e.g., Drs. Ted Janossy, Mark Sperry, Charley Rich, Gary Baggenstoss, and John McMichan).
These preceptorships and their admiration for the parents of Dr. David Warner (pediatric anesthesiologists Drs. Jack and Louise Warner of Children’s Hospital in Columbus, Ohio) led them to seek residency training at Mayo Clinic upon graduation from the medical school in 1979. Mary Ellen completed her residency training in June 1983. First year classmates from that entering resident group in 1979 included her husband, Mark; Bob Chantigian; and Steve Rettke. These four colleagues continue their long-standing ties to the department with a cumulative 162 years of time as anesthesiologists in the institution.
Mary Ellen has held numerous leadership roles in the department and institution. In addition to serving as chair of the former “South” Division at Methodist Hospital, she also chaired the department’s Performance Improvement Committee for nearly two decades. In the institution, she has chaired its Conscious Sedation Task Force that implemented sedation and monitoring standards for the institution, chaired the Surgical Committee’s Procedural Practice Group, and been medical director for Rochester’s Outpatient Procedure Centers. In this latter role, she established new practice models that have been emulated around the world.
Her dedication to her patients, their safety, and the effectiveness of Mayo’s procedural practices resulted in her selection as a recipient of the Mayo Clinic Distinguished Clinician Award in Rochester in 2010. Only three anesthesiologists in Rochester have received this award. The other two are Sait Tahan (1993) and Martin Abel (2005). Two of our colleagues have received this award in Arizona, Joel Larson in 2005 and Terry Trentman in 2018. Roy Cucchiara earned the award in Florida in 2005.
Outside Mayo Clinic, Mary Ellen has been president of the Wood Library Museum of Anesthesiology, one of the world’s leading anesthesiology historical repositories. In 2023 she was the recipient of the WLM’s Distinguished Serve Award. She currently is vice-president of the Anesthesia Foundation.
Mary Ellen and her spouse, Mark, have four sons. They each continue to work clinically in the department.
Mystery Photo Contest Winner
Last week’s contest winner was Todd Witzeling.

Here are this week’s Mystery Photos. Reminder: We are now featuring two individuals each week for the Updates. To be placed into the Mystery Photo Starbucks contest, you will need to correctly guess at least one of the featured individuals. If you identify both of them, you will double your chances of having your name drawn.
Please email your response at warner.mark@mayo.edu within 3 days of this update. I will also need your name and contact information. All correct responses will be placed into a Monday morning drawing for a $10 Starbucks card. Only one winner per individual over the 80 weeks of Mystery Photos. If you win a weekly drawing, however, please keep submitting your responses. An overall winner (with the most correct responses in the series of 80 Updates) will receive a $100 Starbucks card.

Thank you for your readership and welcome to Update #44.
Happy July 4th to everyone, with special emphasis on those who have served our military over the years.
During this past month we have highlighted our department’s remarkable education programs. I had intended to focus this issue on our colleagues who have played major roles in education within the institution or outside of the organization.
However, since this Update landed on July 4th, I thought it would be fitting to focus on our colleagues who have served nobly in our U.S. military forces.
The Mayo Clinic and the Military
In a very real sense, Mayo Clinic was located in Rochester, Minnesota because of the military.
The Civil War and Dakota War of 1862: How They Impacted Mayo Clinic’s Location in Rochester.
As background, the Civil War was sparked on April 12, 1861, with the Battle of Fort Sumter. Minnesota’s governor, Alexander Ramsay, fortuitously was in Washington, D.C. on that day. On April 14th, he volunteered to supply the newly announced Union Army with 1,000 Minnesota volunteers. With the establishment of the 1st Minnesota Regiment, Minnesota became the first state to respond to President Lincoln’s request to raise a Union Army of 75,000 troops. During the war, the “1st Minnesota” became one of the most distinguished regiments in the Union Army. The regiment fought bravely at the 1st Battle of Bull Run, Antietam, Fredericksburg, and in 1863 in its final major battle, Gettysburg. It was at this final battle that the regiment suffered immense losses but held the wavering line at Cemetery Ridge against 1,200 charging Confederate soldiers and saved the Union Army from defeat.
While many able-bodied men from Minnesota were pulled eastward in the 1st Minnesota Regiment, changes were occurring back in the state that triggered the Dakota War on 1862 (Dakota War of 1862 - Wikipedia). In that year, Dr. William Worrell Mayo was living in Le Sueur, Minnesota along the Minnesota River. On August 19th, word of the start of what was to become the Dakota War reached Le Sueur. The 900-person town of New Ulm was under siege by members of the Dakota nation, specifically the Santee Sioux. A volunteer militia from Le Sueur and nearby St. Peter headed to New Ulm, arriving late on August 20th after the first day of the battle. Dr. Mayo and two other physicians were part of that volunteer group. They quickly opened two hospitals in the town and cared for the 5 settlers who were wounded in the opening skirmish of the preceding day. Over the next two days, the town swelled with settlers from the surrounding region. There were approximately 2,500 settlers and military/militia members in the town on August 23rd. The battle resumed on that day. The military reported 16 of its own killed and 24 wounded but there were many settlers also killed and wounded. Contemporary estimates for the killed or wounded, including members of the Dakota nation, range from 300 to 800. Dr. Mayo and his two physician colleagues served admirably. Surviving military participants escorted the remaining 2,000 settlers as they retreated east 20 miles for the safety of Mankato, evacuating New Ulm on August 25th.
After the New Ulm battle, it was determined that the safety of the recruitment office in Mankato for the 1st Minnesota Volunteer Army was in jeopardy and it was moved east 90 miles to Rochester. Dr. Mayo was asked to serve as the examining physician of the 1st Minnesota’s draft board. Dr. Mayo agreed and moved his family, including 2-year-old son Will, to Rochester. He started his position on April 24, 1863. Charlie was born in Rochester in 1865. Welcome to Rochester, Mayo family!
The World War I Impact on the Mayo Brothers and Mayo Clinic
The Mayo Brothers played a major role in World War I by developing field hospitals for the American Expeditionary Forces, vetting specialists to serve in the Army, and improving the quality of care provided by members of the U.S. Army Medical Reserve Corps. Of these tasks, perhaps the most important was that they worked for the Surgeon General of the U.S. Army as consultants to ensure that the volunteer surgical specialists were qualified. An excellent, comprehensive summary of their efforts and those of other Mayo Clinic personnel during WWI was written in 1994 by Dr. Oliver H. Beahrs, one of Mayo Clinic’s most famous surgeons.
The brothers took turns working in Washington, D.C. during the war, with one always in Washington and the other working back in Rochester. It was a very busy time for them, and they expended not only their time but a portion of their fortune to support their work, extensive travel back-and-forth, and expenses of Mayo physicians and nurses who cared for wounded troops in France. The brothers were recognized for their expertise and contributions, with each being promoted to Brigadier General in 1921.
The World War II Impact on the Mayo Clinic
Mayo Clinic responded to the call for medical assistance with a large number of its staff serving in the military during WW II. The clinic also provided “short course” training for many physicians, nurses, nurse anesthetists, and physical therapists in Rochester. Anesthesiology was one of the important specialties chosen for the short course training. The most notable of the Mayo Clinic efforts in WW II include:
- The Mayo Clinic field hospital in New Guinea.
- The Mayo Aero Medical Research Unit.
- The short-course training in several key specialties, including anesthesiology.
Mayo librarian Clark Nelson provided a short summary of Mayo Clinic’s WWII contributions.
For anesthesiology specifically, Lt. Colonel Ed Tuohy introduced continuous epidural/intrathecal administration of local anesthetics during the war. In addition, the previous advocacy for the use of pentothal and storage of cold blood by Dr. John Lundy and colleagues proved crucial to the survival of our wounded military members.
The Mayo Clinic, Our Military, and the Department of Anesthesiology
Many of our department members have served in the military. I would highly recommend that you go to Mayo Clinic | Anesthesiology | Mayo Clinic Military Anesthesia Statistics and view the contributions of many of our colleagues. The military webpage in our departmental historical website is not complete. In the coming year, we hope to populate it more completely. We will form a Mayo Anesthesiology Military History Work Group under the leadership of Dr. Steve Rettke and seek volunteers who can help grow the webpage. We have many past and current department members who are not currently represented on the webpage, especially those from our Florida and Arizona departments.
That said, we currently have many outstanding colleagues represented on the site. I hope that you take a few moments to open the webpage and learn more about their contributions.
Thank you from the Department: Celebrating the Centennial
Challenge coins are an iconic symbol in the military. You may read more about this history and symbolism at Challenge coin - Wikipedia. Historically, these coins are given as a token of appreciation, recognition, and pride for service members who have gone above and beyond their duty.
In this spirit, all 2,100+ staff members across the institution will be receiving Department of Anesthesiology and Perioperative Medicine centennial coins this coming week or two. These coins are designed to commemorate our first 100 years and recognize the remarkable contributes of founders such as Alice Magaw and Dr. John Lundy.
Thank you for your contributions that lead us to being one of the world’s leading anesthesiology departments.
Mystery Photos
Last week’s Mystery Photos were Charles F. McCuskey, M.D. and Daniel R. Brown, M.D.

Charles F. McCuskey, M.D. was born November 26, 1893 in Marshall County, West Virginia alongside the Ohio River 30 miles south of Wheeling. After college at Fairmont State College and West Virginia University, he attended medical school at the University of Tennessee, graduating in 1918. He subsequently served in the U.S. Navy Medical Corps in Charleston, South Carolina. After four years in general private practice in Tennessee, West Virginia, and Washington, D.C., he moved to Rochester and started his residency training on January 1, 1925. He was the first trainee of Dr. John Lundy to complete the residency and joined the Mayo staff on July 1, 1926.
Dr. McCuskey remained on the Mayo Clinic staff until 1933. At that time he moved to Los Angeles and joined the staff of the College of Medical Evangelists (now Loma Linda University’s School of Medicine). By 1938, he had a growing reputation in anesthesiology and was recruited to chair the newly formed department of anesthesiology at the University of Southern California (USC). He served as chair of that department from 1939 through 1961. In his first year at USC, he also served as the first president of the Pacific Coast Association of Anesthetists (to become the California Society of Anesthesiologists). His early years at USC were interrupted by WWII. From December 1941 through February 1946, he was an active leader in the U.S. Army’s Medical Corps. He ended his distinguished military career as consultant to the Pacific Ocean Area and the Central Pacific Area. He received a Bronze Star and retired as a lieutenant colonel, one of the few anesthesiologists to serve in both world wars.
He was one of just a handful of anesthesiologists in the U.S. to serve as president of his state society (1939), the American Society of Anesthesiologists (1948), the American Board of Anesthesiology (1948) and the Academy of Anesthesiology (1957). He also chaired the Section on Anesthesia of the American Medical Association in 1949. He received the ASA’s Distinguished Service Award in 1953 for his organization of state component societies and hosting the first ASA House of Delegates meeting while he was ASA president.
An excellent summary of his life was published in Anesthesia & Analgesia in 1968. Dr. McCuskey and his spouse, Gertrude, had two children. He died on January 24, 1980.

Daniel R. Brown, M.D., Ph.D. was born on May 2, 1964 in St. Paul, Minnesota. He grew up on a sheep farm in Woodbury, Minnesota. After graduating from Hamline University in St. Paul, he obtained his Ph.D. and M.D. degrees from the Medical College of Wisconsin. His Ph.D. in Respiratory Physiology formed the basis from which he learned anesthesia and critical care at Johns Hopkins University.
In 1998, wanting to get back to the Midwest, Dr. Brown joined the Mayo Clinic in Rochester. A strong proponent of critical care medicine, he played a lead role in expanding our department’s footprint in that crucial subspecialty across the institution. It was not easy. Dan led a dedicated group of 10 anesthesiologist intensivists in the early 2000s when he first became chair of the department’s Division of Intensive Care and Respiratory Care in 2001. These individuals spent the majority of their time and an immense number of hours providing care to critically ill patients in an increasing number of ICU units across the Rochester campus. During that period, Dan successfully recruited like-minded, dedicated anesthesiologist intensivists and grew the number of division members during his time as division chair (2001-2021) from 10 to more than 50 intensivists. The critical care anesthesiology group in Rochester is now the largest institutional critical care group in the country, with our department caring for the great majority of the most acutely ill patients in Rochester. Dan and Dr. Francis (Fran) X. Whalen, Jr. began the rapid response team (RRT) in Rochester, with both personally covering this practice until it became a stand-alone service under critical care. It is impossible to overstate the remarkable leadership skills and abilities that Dan brought to advancing Mayo Clinic’s critical care services during the first two decades of this century.
Dan’s efforts were recognized by the institution when he was selected to chair the Independent Multidisciplinary Group in Critical Care in Rochester. This group coordinates all Rochester ICU care. In that role, he also led the institution’s Critical Care Specialty Council. Dan has gone on to lead the institution’s Midwest Hospital Practice Subcommittee, charged with coordination and oversight of the Mayo hospitals in the upper Midwest of the U.S.
Dan is an outstanding clinician and teacher. He has received multiple Teacher of the Year and Clinician of the Year awards in the department and critical care medicine. An excellent educator, Dan is also a long-serving oral examiner of the American Board of Anesthesiology. The institution and a grateful patient’s family honored him by designating a named professorship on his behalf. The Walter and Lenore Annenberg Professor of Anesthesiology in Honor of Daniel R. Brown, M.D. is held by Dr. Mark A. Warner. It is the first named professorship honoring a Mayo Clinic anesthesiologist.
His outstanding professional and leadership efforts have been recognized nationally. Dan served 11 years as a member of the FDA’s Anesthesia and Respiratory Devices Panel. He was on the Board of the American Society of Critical Care Anesthesiologists, a society that evolved into today’s Society of Critical Care Anesthesiologists (SOCCA). He has been a representative to the AMA’s Relative Value Scale Update Committee (RUC), a group that advises Medicare on how to value a physician’s work. He was president of SOCCA from 2018 through 2020, leading the organization through the early days of the COVID pandemic. In 2023, SOCCA recognized Dan with its Lifetime Achievement Award. In 2016, the Hamline College of Liberal Arts named Dan its Outstanding Alumnus.
Dan and his spouse, Heidi, live on a farm in Chatfield where he can be found gardening, tending bees, and pursuing outdoor activities. They have three children.
Mystery Photo Contest Winner

Last week’s contest winner was Tanner Hill.
Here are this week’s Mystery Photos. Reminder: We are now featuring two individuals each week for the Updates. To be placed into the Mystery Photo Starbucks contest, you will need to correctly guess at least one of the featured individuals. If you identify both of them, you will double your chances of having your name drawn.
Please email your response at warner.mark@mayo.edu within 3 days of this update. I will also need your name and contact information. All correct responses will be placed into a Monday morning drawing for a $10 Starbucks card. Only one winner per individual over the 80 weeks of Mystery Photos. If you win a weekly drawing, however, please keep submitting your responses. An overall winner (with the most correct responses in the series of 80 Updates) will receive a $100 Starbucks card.

Photograph: Alan D. Sessler, M.D., undated
The Mayo Clinic Department of Anesthesiology: Educators Internally, Leaders in Education Everywhere
The Department of Anesthesiology has played a major role within the institution in the Education Shield as well as in extramural education societies, on anesthesia-related boards, and in education regulatory organizations. In this early summer series of four Updates, I will describe the history and development of our department’s education programs and the contributions of our department members to institutional and national leadership in anesthesia and respiratory care education. Specifically,
- In the initial week we highlighted the Rochester education programs in nurse anesthesia and respiratory care.
- In the second week we focused on the LaCrosse, Wisconsin nurse anesthesia program and the anesthesiology residency and fellowship programs in Florida and Arizona.
- In the third week we described the Rochester anesthesiology residency and fellowship programs.
- In this final week we will showcase department members who have played major education leadership roles within the institution and nationally.
The Department of Anesthesiology and Educational Programs: Leaders in the Mayo Clinic College of Medicine and Science and In Education Nationally
There are many opportunities to provide leadership in education within Mayo Clinic and in our specialty. In previous Centennial Updates I have highlighted colleagues in the past century who have served as directors of the American Board of Anesthesiology, earned Mayo Clinic’s Distinguished Educator Awards, and been recognized in the Mayo Clinic Fellows Association’s Teacher Hall of Fame. In this issue, I will highlight our anesthesiologists who have served as leaders of the schools within the Mayo Clinic College of Medicine and Science, as well as those who have been officers or chairs of major anesthesia education organizations or regulatory bodies. I have listed their primary education leadership role at Mayo Clinic in parentheses.
- Alan D. Sessler, M.D. (Dean, Mayo Clinic School of Graduate Medical Education). Alan was a life-long advocate for high quality education. In addition to being a Director of the ABA from 1977 through 1989 and its President in 1988, Alan served as an ASA Vice-President of Scientific Affairs. In this latter position, he oversaw the educational programs within the ASA. Alan was the Executive Secretary of the Foundation for Anesthesia Education and Research from 1995 through 2011. In that role, he founded the FAER Academy of Research Mentors and started the FAER Medical Student Anesthesia Research Fellowship program. He served as a member of the ACGME’s Residency Review Committee for Anesthesiology. Within Mayo Clinic, Alan was the Dean, Mayo Clinic School of Graduate Medical Education from 1988-1995. Memories of Alan’s dedication and advocacy for education may be found at two tributes, one written by Dr. Doug Bacon and the other by Dr. Mark Warner.
- Michael J. Murray, M.D. Dean, Mayo Clinic School of Health Sciences). Mike has been an advocate for education in many forums and positions. As a major leader in the evolution of Critical Care Medicine, he served on numerous education-related committees and provide oversight to programs and meetings. He played a key role in the development of our anesthesiology residency program when he was chair of the department in Jacksonville, encouraging Dr. Marie De Ruyter to apply for an accredited program. Mike served as editor of one of the Faust Anesthesiology Review books and has been a co-editor of many other books. He was a long-serving ABA oral examiner and member of the ABA’s Critical Care Medicine Examination Committee. In 2000, he was appointed as Dean, Mayo Clinic School of Health Sciences. Although only in the role for a little over a year as he moved to Jacksonville to chair our Mayo Clinic Florida Department of Anesthesiology, he made several major changes that improved a number of the health sciences training programs.
- William L. Lanier, M.D. (Editor-in-Chief, Mayo Clinic Proceedings). Bill has been a leading educator at Mayo Clinic and outside the institution. Within the department, he chaired the 1988 Task Force on Master’s Degrees in Nurse Anesthesia. He led our department’s institution-wide Academic Appointments & Promotions Committee for 20 years. For a decade, he organized our Rochester Grand Rounds and Visiting Professor programs, instituting exchange visiting professor programs with Duke University, the University of Pennsylvania, and Wake Forest University. Within Mayo Clinic, Bill has been the longest-serving and remarkably successful Editor-in-Chief of the Mayo Clinic Proceedings. During his 18 years of leadership, the Proceedings evolved from a parochial medical journal to the third largest circulation of biomedical journals. In his editor role, he also created Mayo Clinic Proceedings: Innovations, Quality and Outcomes. With that editor role, he was a major contributor to the success of the Mayo Clinic College of Medicine and Science and served on its Education Finance Committee. Outside of Mayo Clinic, Bill was an ABA oral examiner for 20 years, a member of several additional scientific editorial boards, and chair of the Society for Neurosurgical Anesthesia and Critical Care’s (SNACC’s) Education Committee. He was recognized in 2014 by SNACC as its Teacher of the Year. For 6 years, he led the short course for new journal editors for the prestigious Council of Scientific Editors.
- Mark A. Warner, M.D. (Dean, Mayo Clinic School of Graduate Medical Education and Executive Dean, Mayo Clinic College of Medicine and Science). Mark worked closely with Mayo medical students soon after joining staff and was recognized in 1988 with one of the school’s two annual Golden Apple Teaching Awards. He joined Dr. Duane Rorie as the only other Rochester department member to receive this award. His advocacy for medical education expanded from that fortunate start, culminating in 2005 with his selection to serve as Dean, Mayo Clinic School of Graduate Medical Education. His 7-year term as dean was successful primarily because of the efforts and vision of our own Dr. Steve Rose, Vice-Dean of the school. In 2012, Mark advanced to the Executive Dean role of the Mayo Clinic College of Medicine and Science, with oversight of all five Mayo Clinic schools and all education-related activities across the institution. He continued in that role until 2016. He was recognized by Mayo Clinic with one of its Distinguished Education Awards in 2017. Outside of Mayo Clinic, he served 12 years as a Director of the ABA and was its President in 2009. He was a member of the ACGME’s Residency Review Committee for Anesthesiology during a 6-year period and was its Chair from 2006 through 2008. He was also Chair of the ASA’s Section on Education and Research from 2004 through 2008.
- Steven H. Rose, M.D. (Dean, Mayo Clinic School of Graduate Medical Education). Steve has played a major role in our department educational programs throughout his career and is our department’s most highly awarded educator. From 1994 through 2007, Steve was our Rochester department’s residency program director. He also served as our department Vice-Chair for Education from 1994 through 2009. In 2003, he became Associate Dean of the Mayo Clinic School of Graduate Medical Education (MCSGME). He remained in that role through 2009. He also became the Vice-Dean of MCSGME in 2007, working closely with Dr. Mark Warner who was Dean. Steve carried the title of Designated Institutional Official by ACGME from 2007 through 2022, making him the primary contact for the ACGME in one of the country’s largest and finest graduate medical education schools. Steve succeeded Mark as Dean of MCSGME in 2011 and remained in that role through 2021. Like Mark, Steve was recognized by Mayo Clinic with one of its Distinguished Education Awards in 2022. He also has received the ASA’s Excellence in Education Award (2022), the ACGME’s Parker J. Palmer “Courage to Lead” Award (2016), and the Mayo Fellows Association’s Humanitarian Award (2021). He was inducted into the FAER Academy of Research Mentors (Education) in 2012 and the Association of American Medical Colleges Arnold Gold Humanitarian Honor Society in 2016.
- Timothy R. Long, M.D. (Senior Associate Dean for Surgery and Surgical Specialties, Mayo Clinic School of Graduate Medical Education). Tim has followed in the footsteps of Dr. Steve Rose, rising sequentially from our Rochester department’s residency leader to a senior authority in the Mayo Clinic School of Graduate Medical Education (MCSGME) and to a leader in anesthesiology education nationally. Tim became our Rochester program director in 2007 and remained in that role through 2023. He has been our Rochester department’s Vice-Chair for Education since 2009. He was appointed as an Associate Dean of MCSGME in 2019 and rose to Senior Associate Dean in that school in 2022. Outside of Mayo Clinic, Tim has been an oral examiner of the ABA since 2015. He is an editor of the Journal of Education in Perioperative Medicine. From 2021 through 2023, Tim served as the President of the Association of Anesthesiology Core Program Directors. He also is the representative of the Organization of Program Directors Association to the influential Council of Medical Specialties Society. Tim was recognized for his contributions to education by the Mayo Fellows Association with its Teacher of the Year Award and, in 2023, he received the ACGME’s Parker J. Palmer “Courage to Lead” Award.
- David O. Warner, M.D. (Associate Dean for Faculty Affairs, Mayo Clinic Alix School of Medicine). Although primarily recognized nationally for his pulmonary, smoking, and anesthesia epidemiology research expertise and leadership, David has also played a significant role in education. Throughout his career, he has received numerous Mayo Clinic Alix School of Medicine (MCASOM) Excellence in Teaching Recognition awards. In 2009, in recognition of his outstanding research mentorship of many early career clinician investigators from around the world, David was inducted into the FAER Academy of Research Mentors. He became the inaugural Director of the Mayo Clinic’s Office of Applied Scholarship and Education Science in 2014. Outside of Mayo Clinic, David served as a Director of the ABA from 2010 through 2022 and was its President in 2022. He was appointed as Associate Dean for Faculty Affairs of MCASOM in 2017 and served in that role through 2022.
- Renee E. Caswell, M.D. (Associate Dean for Surgery and Surgical Specialties, Mayo Clinic School of Graduate Medical Education). Renee was the longest serving Chair of the Education Committee in our Mayo Clinic Arizona Department of Anesthesiology, with her term lasting from 1997 through 2017. From 1997 through 2005, she was the coordinator for residency training at the Scottsdale and Phoenix campuses. In 2005, she became the Associate Program Director for the Arizona department’s residency program and wrote the accreditation application for it. In 2009, she advanced to the Program Director role and served in that capacity until 2017. Easly in her career, she also was the Director of the department’s Continuing Medical Education program. She was appointed Associate Dean for Surgery and Surgical Specialties within the Mayo Clinic School of Graduate Medical Education (MCSGME) in 2003 and remained in that role through 2008. In addition, Renee chaired the Mayo Clinic Arizona Simulation Subcommittee from 2005 through 2007. She was recognized by Mayo Clinic with its Distinguished Educator Award in 2015.
- Pamela A. Mergens, M.D. (Associate Dean for Admissions, Mayo Clinic Alix School of Medicine): Pam has been involved in medical student and resident education for her career at Mayo Clinic. From 2005 through 2012, she led Grand Rounds in our Mayo Clinic Arizona department. She was the chair of our Arizona residency program’s Clinical Competency Committee from 2007 through 2014. In 2016, she was appointed as Associate Dean for Admissions in the new Arizona campus of the Mayo Clinic Alix School of Medicine. She continued in that role until 2023.
- Susan M. Moeschler, M.D. (Assistant Dean for Faculty Development, Mayo Clinic School of Graduate Medical Education). Susie has made many contributions to education at Mayo Clinic and outside of the institution. In 2015, she was one of the inaugural recipients of an Education Science Career Development Award from Mayo Clinic’s Office of Applied Scholarship and Education Science. In 2016, she received the Course Director of the Year Award from the Mayo Clinic School of Continuing Professional Development for the Mayo Clinic Opioid Conference. Since 2015 she has been the Program Director of our Rochester Pain Medicine Fellowship. She earned recognition in 2023 as the Mayo Clinic College of Medicine and Science’s Outstanding Emerging Educator. She was also appointed as Assistant Dean for Faculty Development by the Mayo Clinic School of Graduate Medical Education in 2023. Outside of the institution, Susie is the President-Elect of the Association of Pain Program Directors. She was recognized in 2019 by the American Society of Pain and Neuroscience with its Excellence in Education Award.
- Lopa M. Misra, D.O. (Associate Dean for Admissions, Mayo Clinic Alix School of Medicine). Lopa has served as a leader of medical student and resident education on our Arizona for nearly 20 years. She led our anesthesiology medical student clerkships and rotations in Arizona from 2008 through 2018. She also has been a member of our Arizona department’s Simulation Committee since 2011 and our Arizona residency program’s Clinical Competency Committee since 2010. She joined the Arizona-based Mayo Clinic Alix School of Medicine’s Admissions Committee in 2021 and was appointed Associate Dean for Admissions in 2023, succeeding Dr. Pam Mergens.
Mystery Photos
Last week’s Mystery Photos were Lee A. Nauss, M.D. and David P. Martin, M.D., Ph.D.

Lee A. Nauss, M.D. was born in Estherville, Iowa on March 28, 1932. After graduating high school in 1950, he spent two years in the U.S. Army Medical Corps as a corpsman. Upon discharge from the Army in 1952 and working for two years as a trucker in Estherville, Lee met a beautiful young candy striper in the Estherville Hospital while visiting his grandfather. Maria and her family had immigrated to Estherville from the Ukraine during a period of political upheaval. Upon meeting, Lee learned that Maria was interested in nursing school. He drove her to several potential schools. At Allen Memorial Hospital in Waterloo, Iowa, the program director enticed both to join the nursing school. They both graduated in 1956 and moved to Rochester, with Maria working as a nurse and Lee as a student in our Nurse Anesthesia program.
Lee completed our nurse anesthesia program in 1958. He and Maria moved to Juneau, Alaska where he organized a department of anesthesia at St. Anne Hospital. He worked there for 7 years. At the urging of several Juneau physicians, Lee and Maria moved In 1965 to Riverside, California where he could take undergraduate pre-medicine classes at La Sierra University in preparation for medical school at Loma Linda University. However, that opportunity at Loma Linda feel through as he was now more than 30 years old, an age discrimination that seems exception in today’s world. Therefore, in 1966 they moved to Little Rock, Arkansas where the University of Arkansas, Little Rock School of Medicine agreed that he would qualify for entry once he was established for a year as a resident of the state. To become a resident of the state, Lee took courses at the University of Little Rock on Monday, Wednesday, and Friday and worked as a nurse at Children’s Hospital in Little Rock on Tuesday, Thursday, and Saturday. It all paid off as he matriculated to the University of Arkansas, Little Rock Medical School in 1967.
Lee earned his M.D. in 1971. His post-graduate training included an internship in Little Rock and a year of anesthesia residency training at Virginia Mason Hospital in Seattle. He and Maria had planned on his completing his anesthesia training at Virginal Mason and then moving to Alaska. However, there was an epic battle between the state of Alaska and its state board of medical practice at the time and the board essentially dissolved and would not consider applications for new medical licenses. Stuck in a Catch-22 situation, Lee decided to finish his residency training at Mayo Clinic in Rochester.
Lee and Maria arrived in Rochester with their U-Haul trailer in late June 1973 on a Saturday morning. He contacted the anesthesia office and was told that he was on call at St. Marys Hospital that evening. Welcome to Rochester, Lee! His first night on call and in town, he was covering obstetrics at SMH and decided to use an epidural anesthetic for a laboring patient. It wasn’t the first epidural used in obstetrics at Mayo Clinic but it triggered quite a discussion as the obstetricians had previously determined that none of their patients would receive epidurals. To Lee, it was natural as he was trained to use epidural analgesia at Virginia Mason. Ultimately, both Drs. Dick Theye (chair of Anesthesiology) and George Malkassian (chair of OB/GYN) agreed that epidurals were acceptable as long as Lee taught all of the residents to place them.
Upon graduation from residency training, Lee joined the department staff and organized a program for the treatment of chronic pain at Methodist Hospital. He was joined in the effort by the return of former Mayo Clinic anesthesia resident, Dr. Joe Wang (class of 1968). Together they built what is now the Pain Clinic. They were joined in that effort in 1982 with the return of Dr. Peter Wilson from Australia. Peter was a post-doctoral fellow (Fulbright Scholar) at Mayo Clinic in 1976, working on understanding the mechanism of action of opioids and non-opioid neurochemicals (e.g., baclofen) when injected intrathecally.
Lee and Joe were intrigued by the potential of using intrathecal or epidural opioids for the treatment of acute and chronic pain. Mayo Clinic had several key scientists involved in the study of spinal opioids, specifically Drs. Frederic Kerr and Tony Yaksh. At Tony’s urging, in 1977 Lee used epidural morphine in a lung cancer patient who got complete pain relief. It was the first use of intrathecal opioids in a human. After organizing a small study of 7 additional patients who had intractable cancer pain and recruiting Dr. Juergen Thomas of the Department of Neurology to assist, Joe, Lee, and Juergen published the world’s first report of the use of intrathecal morphine in humans. Our own Peter Southorn, Lee’s residency classmate, wrote about this remarkable advance in medicine in a department newsletter.
Lee received multiple Teacher of the Year Awards from the Mayo Clinic Fellows Association in recognition of his exemplary education of anesthesiology residents. He was a gifted clinician, amazing storyteller, and extraordinarily humble and gracious colleague. Lee retired from the department in 1997.
Maria passed away on February 24, 2006. Lee subsequently met and married his current wife, Geri, on January 1, 2009. In a bit of a fairy tale ending, Geri and Lee were introduced together by a couple with whom Lee and Maria had shared a cabin in Alaska, just south of Denali. Lee and Geri currently reside in Rochester.

David P. Martin, M.D., Ph.D. was born in Cincinnati, Ohio on April 28, 1964. The family moved to Kokomo, Indiana when he was 6 years of age. He completed undergraduate studies at Indiana University in 1985 and earned his M.D. and a Ph.D. in Neuroscience at Washington University in St. Louis in 1992. After an internship in St. Louis, he moved to Rochester as a resident in anesthesiology, graduating in 1996. Colleagues in his 1996 class who have served as members of our department include Roxann Pike, Todd Kor, and Brian McGlinch. Following residency, he did a fellowship in pain medicine combined with postdoctoral research in the Neurology laboratory of Dr. Phillip Low. Investigations related to that research later contributed to the creation of a high-frequency spinal cord stimulation device that is still used clinically today.
Dave chaired the Division of Pain Medicine from 1999-2001. During an era where it became increasingly challenging to excel in both the operating rooms and Pain Clinic, he chose to switch entirely to the operating rooms, specializing in orthopedic anesthesia and liver transplant. He served as departmental Vice Chair for Safety and Quality from 2010 to 2023 and implemented Safety & Quality Grand Rounds, our Near Miss program, and the SAFE-CAER event review. His roles also included serving as the medical director for the moderate sedation practice for all Mayo Clinic enterprise procedural sites.
Outside of Mayo Clinic, Dave has been an extraordinarily active member of multiple organizations. Within the Minnesota Society of Anesthesiologists (MSA), he has held every office in that society, concluding his time as an officer when he was elected President in 2015. He was awarded the MSA Distinguished Service Award in 2022 for his dedicated effort to sustain and grow the society. He has been very engaged in both committee and editorial board work in the American Society of Anesthesiologists (ASA). Highlights include becoming the founding editor-in-chief of Patient Safety CME Editorial Board, Section Chair for Education and Research, and Director. He was elected ASA Vice President for Scientific Affairs in 2022, an office he holds today. Recently, Dave joined the board of directors of the Foundation for Anesthesia Education and Research (FAER). He also is the current President of the Academy of
Anesthesiology. The Academy was formerly the Anesthesia Travel Club first started by Dr. John Lundy in 1929.
Dave’s steady hand, tenacity, and vision for the specialty have made him invaluable to our department, the Mayo Clinic, and the ASA and other specialty organizations. Dave and his wife, Laura, have 2 adult children and 3 grandchildren.
Mystery Photo Contest Winner

Last week’s contest winner was Bob Chantigian.
Here are this week’s Mystery Photos. Reminder: We are now featuring two individuals each week for the Updates. To be placed into the Mystery Photo Starbucks contest, you will need to correctly guess at least one of the featured individuals. If you identify both of them, you will double your chances of having your name drawn.
Please email your response at warner.mark@mayo.edu within 3 days of this update. I will also need your name and contact information. All correct responses will be placed into a Monday morning drawing for a $10 Starbucks card. Only one winner per individual over the 80 weeks of Mystery Photos. If you win a weekly drawing, however, please keep submitting your responses. An overall winner (with the most correct responses in the series of 80 Updates) will receive a $100 Starbucks card.

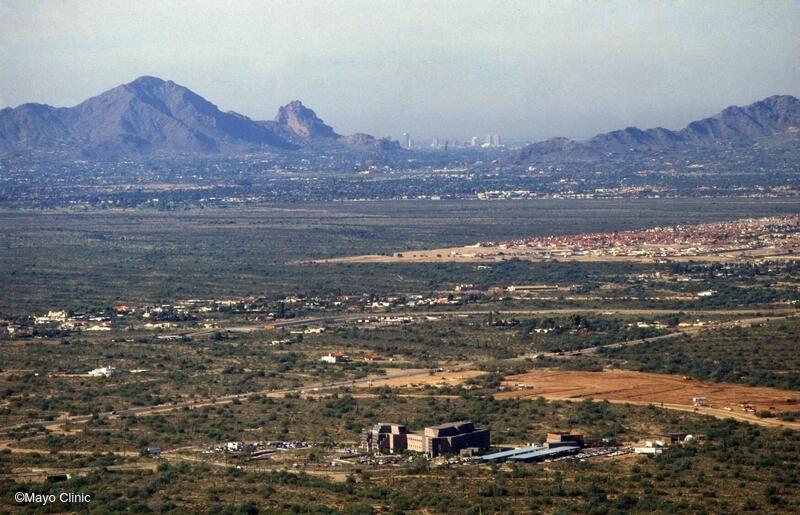
Photograph 1: Aerial view of Mayo Clinic's Jacksonville campus, 1986. Photograph 2: Aerial view of Mayo Clinic's Scottsdale campus, 1987.
The Mayo Clinic Department of Anesthesiology: The Early Development of Departments in Jacksonville, Florida and Scottsdale, Arizona
The underlying issues that drove Mayo Clinic to expand to states far beyond the Upper Midwest U.S.:
Payment systems in the U.S. evolved dramatically from 1935 through the late 1980s. In 1935, President Franklin Roosevelt signed the Social Security Act in one of his first major “New Deal” objectives. This act served the nation’s poor well for its first three decades but stumbled in meeting its objectives of providing healthcare support for many Americans. By 1961, President John F. Kennedy set out to improve medical care for elderly U.S. citizens by establishing a Medicare Task Force. By 1965, the task force’s recommendations led to President Lyndon B. Johnson’s signing of the Social Security Amendment Act (Medicare and Medicaid Act). Healthcare coverage for elderly and poor Americans rose exponentially, as did the country’s overall healthcare spending.
By the late 1970s, it was clear that healthcare expenses were spiraling upwards and that there was a need as a nation to control the rate of growth of these expenses. Multiple attempts were made in the 1980s (and have continued to be made since), most with modest and variable impact on overall healthcare expenditures. As with many national healthcare policies then and now, there were unanticipated consequences of their implementation and many of the changes during that decade fell short on providing their projected financial savings. Examples include:
- The 1981 Omnibus Budget Reconciliation Act (OBRA 1981): This act expanded Medicare and Medicaid benefits to home health care and new Medicare Supplement (Medigap) coverage. Both were anticipated to lower overall Medicare and Medicaid expenses by providing funds to pay for out-of-hospital care. In general, and for both, the opposite financial outcome occurred.
- The 1982 Tax Equity and Fiscal Responsibility Act (TEFRA): This act expanded benefits to hospice care, introduced prospective payment plans for coverage of unique populations, and added oversight of proposed care (e.g., surgical procedures) by Peer Review Organizations (PROs).
- The 1989 Omnibus Budget Reconciliation Act (OBRA 1989): This act required healthcare providers to provide pre-service estimates of the costs of their planned care management and approval by PROs before the care was delivered or reimbursed.
Not surprisingly, the rising healthcare industry adapted to these new regulations . . . and costs continued to climb. As you can imagine, administrative costs associated with these expanded regulations grew rapidly. New models of care popped up quickly. Those of us who worked in the 1980s will recall abbreviations such as HMOs (Health Maintenance Organizations), PPOs (Preferred Provider Organizations), and IPAs (Individual Practice Associations). In general, all were attempts by individual physicians, small groups, and large healthcare systems to remain profitable or even viable during this tumultuous period of expanding healthcare coverage and restrictions on payments. A more detailed summary of these changes may be found here.
One key issue that concerned large groups and healthcare systems: there was a general movement to restrict movement of patients from any one region of the country (or from one state to another). The hope was that regionalization of healthcare would encourage early non-procedural interventions (e.g., increased medication use, improved lifestyle choices) and reduce the need for expensive care associated with advanced procedural care (e.g., coronary bypass surgery). This movement raised concerns of large group practices and healthcare systems such as Mayo Clinic. At the time, approximately 30% of our patients came to Rochester from outside of our Upper Midwest region.
Mayo Clinic leaders responded to this concern by planning for new sites in Florida and Arizona. Sites in Texas were also considered initially. The institution’s geographic diversification was into the two largest U.S. cities that did not have existing medical schools at the time and cities that appeared to be relatively underserved by academic medical institutions. In addition, both Jacksonville and Phoenix were experiencing rapid growth at the time. Excellent video summaries of the start and growth of the Florida and Arizona sites may be found at Mayo Clinic in Florida: 30th Anniversary | Mayo Clinic History & Heritage and Mayo Clinic in Arizona: 30th Anniversary | Mayo Clinic History & Heritage, respectively. Both webpages are part of the Mayo Clinic History and Heritage website. This website is available to the public as well as Mayo Clinic personnel. It is also the same website that hosts our Department of Anesthesiology’s history webpages (Anesthesiology Department | Mayo Clinic | History and Heritage).
The First Two Years of Our Department in Florida
In 1986, the institution completed construction of its first Jacksonville area building on land donated by Mr. James E. Davis. It was located in the middle of an expansive pine forest along the Atlantic Intracoastal Waterway. The new Davis Building and the community-based St. Luke’s Hospital (250 beds, 14 operating rooms, and 8 miles west of the Davis Building and new Mayo campus) was staffed initially by 35 Mayo faculty members. Dr. Alan D. Sessler, chair of our department in Rochester, oversaw the development of our new anesthesiology department. He recruited Drs. James V. Harper and Timothy S. J. Shine to provide anesthesia services. Jim and Tim subsequently recruited four Rochester nurse anesthetists. These were Linda Buck, Burdette (Bud) Polk, Alicia Casabar, and Phil Kleinschmidt.
The St. Luke’s Hospital anesthesia practice was a mixed model of Mayo Clinic staff who provided services for Mayo Clinic patients and a private group of anesthesiologists who provided services for the majority of non-Mayo Clinic patients. Surgical volumes grew dramatically in the first months of operation during 1986 and 1987 and additional anesthesiologists were recruited to join our Mayo staff. The first of these new recruits included Drs. Lisa J. Vucalcic, Jerry A. Dorsch, Neil G. Feinglass, and David Mackey. By 1988, Jim Harper was appointed chair of the new Department of Anesthesiology at Mayo Clinic Jacksonville (the site’s name changed to Mayo Clinic Florida later). That same year St. Luke’s Hospital became an affiliate of Mayo Clinic, with Mayo Clinic Jacksonville assuming St. Luke’s Hospital corporate assets and liabilities.
The First Two Years of our Department in Arizona
In 1987, the Mayo Clinic Building opened in Scottsdale. Forty physicians initially staffed:
- The new Mayo Clinic Building
- Scottsdale Memorial Hospital – Osborn
- Scottsdale Memorial Hospital – North
- The Piper Center, an ambulatory surgery center adjacent to and associated with Scottsdale Memorial Hospital – North
Dr. Sessler also oversaw development of our new anesthesiology department in Scottsdale. He recruited Drs. John C. McMichan and Jesse J. Muir from Rochester and Dr. Kent P. Weinmeister, a 1982 graduate of our Rochester residency program and in private practice in Illinois. John McMichan was appointed chair of the department. During 1988 and 1989, with expansion of operating rooms at Scottsdale Memorial Hospital – North, additional anesthesiologists were recruited. These included Drs. Kurt E. Springmann and Mark R. Matthews.
During the initial year, nurse anesthetists were not part of the model of care as this model was fairly novel for Arizona in general and in the Phoenix area, specifically, at the time. Within a year (in 1988), the team care model at Mayo Clinic Scottsdale (to be named Mayo Clinic Arizona later) was approved and Pauline C. Bisel, CRNA and John (Jack) D. Hostak, CRNA were recruited to Arizona from Rochester. During the first year, while awaiting hospital privileges at Scottsdale Memorial Hospital – North, Pauline and Jack performed preoperative evaluations and provided sedation for outpatient procedures performed in the Mayo Clinic Building. By 1989, they received privileges to practice in Scottsdale Memorial Hospital – North.
Photographs from left to right: Alan Sessler, Jim Harper, Tim Shine, Linda Buck, Burdette Polk, Alicia Casabar, John McMichan, Jesse Muir, Kent Weinmeister, Pauline Bisel, and Jack Hostak.
Mystery Photos
Last week’s Mystery Photos were William L. Lanier, M.D. and Bruce J. Leone, M.D.

William L. Lanier, M.D. was born on June 8, 1955, in Statesboro, Georgia. He grew up on a farm near Metter in southeast Georgia. He attended the University of Georgia, graduating in 1976. He subsequently matriculated to the Medical College of Georgia. Upon earning his M.D. in 1980, he served as a resident in anesthesiology at Wake Forest University from 1980 through 1983. He followed his residency with subspecialty training in neurosurgical anesthesiology at Mayo Clinic in Rochester and was appointed to the Mayo Clinic faculty in 1984. By 1995, Bill had risen to the rank of Professor of Anesthesiology.
Bill was actively engaged in both laboratory and clinical research throughout his career. For 10 years, he served on the research team of Dr. John (Jack) Michenfelder’s Cerebral Blood Flow and Metabolism Laboratory at St. Marys Hospital. From there, he moved to the Medical Science Building on the Rochester campus where he established and was medical director of the Neuroanesthesiology Research Laboratory for the next 13 years. His original research focused on neuroprotection, cerebral physiology, and clinical neuroanesthesiology. He also published and lectured extensively on quality of medical evidence, medical ethics, and professionalism. Two of his most clinically important lines of research involved (1) augmentation of ischemic brain injury by clinically relevant doses of intravenous glucose solutions or minor changes in blood glucose concentration and (2) modulation of ischemic brain injury by small (e.g., 1ºC) changes in temperature. Notably, the former research resulted in changes in default intravenous 5% glucose fluid usage in anesthesiology practice worldwide and the latter research resulted in changes to how we now manage patients with ischemic brain injuries.
Bill was president of the Society for Neuroscience in Anesthesia and Critical Care (SNACC) in 1994. In 2011, he was named SNACC’s Teacher of the Year and in 2014 was recognized with the SNACC Distinguished Service Award. He was an examiner for the American Board of Anesthesiology from 1994-2014. Additionally, he has been a scientific reviewer or consultant for approximately thirty-five indexed scientific journals. He was a founding section editor for the Journal of Neurosurgical Anesthesiology; a founding editorial board member for Disaster Medicine and Public Health Preparedness; and the senior editor overseeing the conceptualization, planning, and launch of Mayo Clinic Proceedings: Innovations, Quality & Outcomes.
Bill’s many education accomplishments were highlighted in last week’s Centennial Update #45. Bill has been active his entire career and even now in retirement with mentoring high-school-, college-, and medical students, as well as resident physicians and early career faculty in anesthesiology and other fields. More than ten of his Mayo Clinic mentees have joined our departments across the institution and have spent their entire careers on the faculty. He has also mentored students seeking advanced academic degrees in the Mayo Clinic School of Nurse Anesthesia. He has been a strong advocate as well as mentor for trainees of all types during his career.
Bill remained active as a practicing physician until the time of his retirement in September 2021. However, from January 1999 to early-2017, he spent most of his professional effort serving as editor-in-chief of Mayo Clinic Proceedings, the world’s third largest circulation scholarly biomedical journal. At the time of his appointment, the Proceedings was a provincial publication, with authorship of articles overwhelmingly from Mayo Clinic physicians and scientists. During his time as editor-in-chief, and because of promotional efforts for a new Journal vision, authors from approximately sixty nations submitted manuscripts, and the journal’s Impact Factor increased from 2.0 to 7.2. He is the longest serving editor of the Mayo Clinic Proceedings.
Bill is an avid hunter and angler, having hunted and fished throughout North-, Central-, and South America. He has been active in introducing many young people to fishing. He and his wife, Mary, also enjoy gardening, travel, foods, and the arts. Bill and Mary have two children. In September 2023, they moved to their 1,000-acre Zedee Farms north of Metter, GA. The farms have been in the Lanier family for more than 2 centuries. They now actively manage their farms for commercial timber production and wildlife habitat.

Bruce J. Leone, M.D. was born in Boston, Massachusetts on November 23, 1957. He attended undergraduate school at Harvard University and graduated in 1978. After Harvard, Bruce matriculated to the University of Florida College of Medicine, graduating in the class of 1982. He completed his rotating Internal Medicine internship at Baylor University Medical Center at Dallas, Texas in 1983 and his anesthesiology residency at the University of Texas Southwestern Medical Center (Parkland Hospital) in 1985. Bruce then did a research fellowship in Cardiac Anesthesiology at Parkland Hospital, completing this in 1986, followed by two years as a Senior Registrar at the Nuffield Department of Anaesthetics at Oxford University, UK. He became an Assistant Professor of Anesthesiology at Duke University Medical Center in 1987 and completed a second cardiac anesthesiology fellowship at Duke University Medical Center in 1988.
After a decade at Duke University, Bruce joined our Mayo Clinic Florida faculty in 1998 and helped establish the cardiac and pulmonary transplant programs, working alongside cardiac surgeon, John Odell, M.D. Bruce served as Vice-Chair of the department in Research and Academic Affairs, as well as the general Vice Chair of the department. He also served as Program Director of the anesthesiology residency program from 2013 through 2015. In his education role, he was a long-serving member of our Jacksonville’s Surgery and Surgical Specialties education committee within the Mayo Clinical School of Graduate Medical Education. He was a member of the cardiac anesthesia team at Mayo Florida from 1998 through 2008, when he then transitioned to neuroanesthesia, serving as Chief of Neuroanesthesia Division from 2009 through 2014.
Bruce was active in national organizations such as the ASA. He served on ASA committees related to clinical as well as experimental circulation and equipment and facilities. He was a reviewer for the NIH’s Surgery, Anesthesia, and Trauma Study Section. Bruce was a member of the editorial boards of the Journal of Cardiothoracic and Vascular Anesthesia and the journal Anestesia en Mexico.
Bruce retired in October 2023 as a Professor of Anesthesiology. He now spends his time traveling between his homes in North Carolina and Florida with his wife Christine and their pets.
Mystery Photo Contest Winner

Last week’s contest winner was Mary Miller Mazza.
Here are this week’s Mystery Photos. Reminder: We are now featuring two individuals each week for the Updates. To be placed into the Mystery Photo Starbucks contest, you will need to correctly guess at least one of the featured individuals. If you identify both of them, you will double your chances of having your name drawn.
Please email your response at warner.mark@mayo.edu within 3 days of this update. I will also need your name and contact information. All correct responses will be placed into a Monday morning drawing for a $10 Starbucks card. Only one winner per individual over the 80 weeks of Mystery Photos. If you win a weekly drawing, however, please keep submitting your responses. An overall winner (with the most correct responses in the series of 80 Updates) will receive a $100 Starbucks card.

Please note that we will not have an Update on Thursday, August 1st. I will be traveling overseas at that time. We’ll pick back up on August 8th with Update #48.
The Mayo Clinic Department of Anesthesiology: Officers of Exceptional Rank
Mayo Clinic in general, and the Department of Anesthesiology specifically, has produced many leaders in the U.S. military. Notably, both Will and Charlie Mayo were promoted to Brigadier General rank in the U.S. Army Medical Reserve Corps in 1921. The institution has been a strong supporter of its staff members who have been involved in the various military branches, providing them special benefits when they are called to active duty. These benefits, including military salary augmentation, often exceed those provided by most academic medical centers.
There are two primary categories of military rank in the U.S. military branches. These are enlisted ranks and officer ranks. There also is a category of military rank for a unique group of personnel who have unique technical skills and knowledge. This category, warrant officers, is important but relatively small and more can be read about personnel in it online.
Enlisted Ranks
Typically, military personnel in enlisted ranks have not obtained the undergraduate degrees required of commissioned officers. They provide the great majority (82%) of military personnel overall. They are the soldiers, marines, sailors, and airmen who serve the country so well. Enlisted personnel are classified by rank type and a rank designation. These differ between various military branches. The rank designation is the letter “E” (for enlisted) and the levels rise from 1 through 9.
Army, Marines, Air Force, and Space Force | Navy and Coast Guard |
E-1: Private | E-1: Seaman recruit |
E-2: Private 2nd class | E-2: Seaman apprentice |
E-3: Private 3rd class | E-3: Seaman |
E-4 Corporal | E-4: Petty officer 3rd class |
E-5: Sergeant | E-5: Petty officer 2nd class |
E-6: Staff Sergeant | E-6: Petty officer 1st class |
E-7: Sergeant 1st class | E-7: Chief petter officer |
E-8: Master Sergeant | E-8: Senior chief petty officer |
E-9: Master Sergeant | E-9: Master chief petty officer |
Officer Ranks
Typically, military personnel who have earned undergraduate degrees and completed officer military training (e.g., at a U.S. military academy, in a Reserve Officer Training Corp – ROTC – in a university, or an Officer Candidate School) qualify for commissions in the various military branches. These commissions are approved by the President of the United States. Commissioned Officers comprise 18% of all military personnel. Officers also are classified by rank type and a rank designation. These differ between various military branches. The rank designation is the letter “O” (for enlisted) and the levels rise from 1 through 10 (although several branches have an 11th level during war).
Army, Marines, Air Force, and Space Force | Navy, Coast Guard, and Public Health Service |
O-1: 2nd Lieutenant | O-1: Ensign |
O-2: 1st Lieutenant | O-2: Lieutenant junior grade (j.g.) |
O-3: Captain | O-3: Lieutenant |
O-4: Major | O-4: Lieutenant commander |
O-5: Lieutenant colonel | O-5: Commander |
O-6: Colonel | O-6: Captain |
O-7: Brigadier general | O-7: Rear admiral lower half |
O-8: Major general | O-8: Rear admiral upper |
O-9: Lieutenant general | O-9: Vice-admiral |
O-10: General | O-10: Admiral |
Our department has been represented in the military in both enlisted and officer ranks. Our enlisted personnel have served in many roles, including riflemen, communication specialists, and Navy corpsmen and Army medics. Please note that a number of military roles incorporate the term “man” but are gender neutral. Many of these individuals enter healthcare fields after completing their military service and then join our department as administrators, support staff, respiratory therapists, nurse anesthetists, and anesthesiologists. Our Officer personnel have attained undergraduate degrees, undergone officer training, and entered or re-entered the military through the draft, voluntary enrollment, or as a requirement of receiving undergraduate or graduate military scholarships.
As you might note in the lists above, advancing up the Officer ranks that run from levels 1 through 10 takes time, talent, and outstanding performances. Within the 10 Officer rank levels, there are two inflection points: (1) between the O-5 and O-6 levels and (2) between the O-6 and O-7 levels. These distinct points are characterized by the following (using Army and Navy examples):
- Advancing from an O-5 rank level (i.e., Lieutenant colonel or Commander) to an O-6 level (i.e., Colonel or Captain) requires approval by the President and confirmation by the U.S. Senate. At lower levels, the President of the United States has sole discretion of approving appointments and promotions. These promotions typically are based on recommendations from military promotion boards. Promotions to the O-6 rank level, however, require Presidential approval and confirmation by the U.S. Senate. In general, the U.S. Senate provides its Armed Service Committee with the primary authority to review these promotion requests.
- Advancing from an O-6 rank level (i.e., Colonel or Captain) to an O-7 level (Brigadier General or Rear Admiral lower half), like promotion to O-6 levels, require approval of both the President and the U.S. Senate. Unlike promotions to the O-6 level, however, promotions to the O-7 level undergo much more intense scrutiny by the U.S. Senate Armed Services Committee and, occasionally, the full Senate.
Officers who advance to the O-6 rank level (Colonel or Captain) or higher, especially in the Army, Air Force, and Navy Medical Corps, represent a very small, unique group of outstanding military and medical leaders. In our first 100 years as a department, at least 10 remarkable individuals have achieve the O-6 rank level. One, Dr. Robert L. Lennon, has served at an O-7 rank level (Army Brigadier General). Bob is one of only a very small number of anesthesiologists or nurse anesthetists overall to attain this lofty rank in the nation’s history.
These outstanding individuals, listed alphabetically, are:
- Eric L. Bloomfield, M.D., Colonel, U.S. Air Force
- Edward P. (Paul) Didier, M.D., Colonel, U.S. Army
- Robert L. Lennon, D.O., Brigadier General, U.S. Army
- Brian P. McGlinch, M.D., Colonel, U.S. Army
- Paul D. Mongan, M.D., Colonel, U.S. Army
- Michael J. Murray, M.D., Ph.D., Colonel, U.S. Army
- Steven R. Rettke, M.D., Captain, U.S. Navy
- Benjamin W. Riley, CRNA, DNAP, Colonel, U.S. Army
- Frank J. Villamaria, M.D., Captain, U.S. Navy
- Francis (Fran) X. Whalen, Jr., M.D., Colonel, U.S. Army
You may read more about each of these exemplary leaders on our department’s history website at Mayo Clinic | Anesthesiology | Mayo Clinic Military Anesthesia Statistics. Clicking on the photo of each will provide you with background information on each. This website currently contains information on 35 department members who have served in the military. However, we believe that as many or more than 100 past and current members have served in the military. Dr. Steve Rettke and I are forming site-specific military advisory groups who we hope will be able to identify colleagues, past and present, who have served. We will then follow up with communications to encourage them to add their information to the department military webpage.
Mystery Photos
Last week’s Mystery Photos were Steven R. Rettke, M.D. and David O. Warner, M.D.

Steven Rettke, M.D. was born in Marinette, Wisconsin on October 22, 1946. He attended Western Michigan University in Kalamazoo, Michigan, earning a B.S. degree in Aviation Engineering in 1969. We believe he may be the only consultant in our institution’s history to hold an Airframe and Powerplant mechanic’s license. Steve also received a B.S. degree in biology from Jacksonville University (Florida) in 1975. He subsequently earned his M.D. degree in 1979 from the University of Wisconsin, Madison. He did his residency in anesthesiology at Mayo Clinic Rochester and joined our staff in 1982. His classmates in that entering 1979 residency class included Drs. Bob Chantigian, Mary Ellen Warner, and me. Our cumulative years on staff at Mayo Clinic now stand at 164.
Prior to completing his first college degree, Steve joined the U.S. Naval Reserve in February 1967 as an Aviation Reserve Officer Candidate (AVROC). He entered active duty in 1969 after receiving his initial officer commission. Steve then earned his wings as a Naval Aviator on October 16, 1970. His class was the last to fly the TF-9J Cougar. He qualified to fly onto and off of aircraft carriers aboard the U.S.S. Lexington (CV-16). He went on to fly the A-7 Corsair and was attached to Attack Squadron 87 (VA-87). A photo of Steve in his Corsair may be viewed below. He was deployed from February 1972 to December 1972 aboard the U.S.S. Franklin D. Roosevelt (CVA-42) to the western and eastern Mediterranean area of operations. He transferred to the U.S. Navy Medical Corps after medical school and spent a total of 27 years of active and reserve duty before retiring as a Captain.

Steve was a leader in our Rochester department throughout his career. He was Section Head of Rochester Methodist Hospital North Anesthesia from 1986 to 1988. He then was Division Chair of Multispecialty Anesthesia from 1988 to 1991. From 1992 to 2000 he was Division Chair of Rochester Methodist North Anesthesia.
Our department has been asked to provide anesthesia care for several U.S. presidents and their family members over the years. I’m not violating any HIPAA regulations when sharing this publicly available information with you that Presidents Lyndon B. Johnson, Ronald Reagan, and George H. W. Bush received perioperative care led by Mayo anesthesiologists (in Washington, D.C.) or by our Mayo anesthesia care teams across the institution. For example, Dr. Paul Didier provided care for Presidents Johnson and Reagan. Steve was our leader in caring for Presidents Reagan and Bush. Dr Roy Cucchiara led the care for President Reagan. Dr. Jim Hebl was involved in the care of President Bush. Our institution-wide department is fortunate to be asked to provide care for many U.S. and international leaders. Special kudos for those who have provided this care and for treating each of these leaders well, just as we do for all patients.
Steve was our lead anesthesiologist in the initial establishment of the Mayo Clinic liver transplant program, working closely with colleagues such as gastroenterologists Drs. Roland (Rollie) Dickson and Russell (Russ) Weisner and transplant surgeon Dr. Ruud Krom. As our department’s Liver Transplant Program Coordinator from 1984 to 1998, he was responsible for setting up protocols and working with other Institutional specialties. This involved designing and, with Mayo Engineering, building the Mayo rapid infusion pump since there were no commercially available rapid infusion pumps at the time. The original engineering drawing for the first version of the Mayo rapid infusion pump can be found below. Nationally, Steve was the anesthesia specialty’s representative to the United Network for Organ Sharing (UNOS). In addition, he was the inaugural chair of the ASA’s Committee on Transplant Anesthesia.
In December 2014, Steve retired as Professor of Anesthesiology. He and his wife Mary have two sons and reside in Rochester.

David O. Warner, M.D. was born in Columbus, Ohio on May 31, 1957. For those aware that David is my first cousin, his parents, Drs. E. Jackson (Jack) Warner and Louise Oman (Omie) Warner were pediatric anesthesiologists at Children’s Hospital in Columbus (now Nationwide Children’s Hospital). David obtained his undergraduate degree and his M.D. from the Ohio State University in 1979 and 1983, respectively. According to Dr. Peter Southorn in his summary about David in our department’s Art to Science text about our history (published in 2000), “He (David) was lured to Rochester by his cousin . . . “ I’m not sure “lured” is the correct term, but Mary Ellen and I were able to interest David and his wife, Julie, into visiting Rochester, a trip that may have been one of the best things Mary Ellen and I have done for Mayo Clinic and our department. Regardless of how he got to Rochester, David completed his five-year residency program in 1988. It included two years as a research fellow under the mentorship of Dr. Kai Rehder.
While David’s clinical career was predominantly focused on the care of children, his research interests varied over his 35 years as a consultant in our department. He was, and remains, a remarkable and innovative researcher. His research falls into six primary categories.
- Respiratory physiology: David’s early work with Drs. Kai Rehder and Bob Hyatt was focused on pulmonary mechanics and respiratory muscle physiology. His work led to our current understanding that volatile anesthetics relax smooth muscle both by impairing neural reflexes and by direct effects on airway smooth muscle. The ability of volatile anesthetics to relax even maximally stimulated airway smooth muscle is unique (e.g., not shared by beta-adrenergic agonists) and is the foundation for ongoing drug discovery efforts seeking novel bronchodilators.
- Perioperative tobacco control: David had a longstanding desire to improve perioperative lung health. His studies on the impact of tobacco smoke on lungs during and after anesthesia and surgery, as well as the potential to use the perioperative period to get patients to stop smoking, have led to major reductions in perioperative pulmonary complications as well as increased rates of smoking cessation in surgical populations. He founded the ASA’s Smoking Cessation Task Force in 2008 and influenced the Centers for Medicare & Medicaid Services (CMS) to pay anesthesia professionals for smoking cessation counseling of patients.
- Neurodevelopment following anesthesia and surgery in children: Based on preclinical studies suggesting that anesthesia may be associated with neurotoxicity in the developing brain, David organized a departmental team to investigate this issue in children undergoing anesthesia and surgery. The team’s first studies providing evidence that neurotoxicity from anesthetics may occur in children, showing that anesthetic exposure within the first three years of life is associated with a doubling of the risk for the later development of learning disabilities. Ongoing research is aimed at understanding whether anesthesia and surgery is causative or simply confounding in behavior changes and diminished fine motor skills in children and later in their lives, especially in those with multiple exposures to anesthesia and surgery.
- Cognition after anesthesia and surgery in the elderly. Similar to the findings that anesthesia may cause neurotoxicity in developing brains, there is some evidence that this impact may also be found in elderly brains. David assembled a Mayo team and found that although surgery with anesthesia is not associated with an increased risk of clinical diagnoses of long-term cognitive impairment, it is associated with a modest acceleration of cognitive decline. These results are reassuring from the standpoint of anesthesia exposure but highlight the continued need to address perioperative brain health as his team also found that postoperative delirium is associated with subsequent cognitive impairment.
- Innovation in postgraduate medical education and assessment. As a director of the American Board of Anesthesiology, David led its Research Committee and produced papers that documented the value of board certification as well as increased understanding of how anesthesia professionals process and retain new information. These studies led to his development of the ABA’s Maintenance of Certification in Anesthesiology (MOCA) continuing education assessment tool, the MOCA Minute. They also triggered the inclusion of a novel Objective Structured Clinical Exam (OSCE) into the ASA’s examination process.
- Research in education and mentorship. David recognized the need for improvements in our educational systems at Mayo Clinic and elsewhere. He founded the Mayo Clinic College of Medicine and Science’s Office for Applied Scholarship and Education Science (OASES). The OASES program brings the expertise of professional educators to our institution’s educational programs.
Administratively, David has served within our department as its Rochester vice-chair for research. He co-founded the Mayo Perioperative Outcomes Group in 1995 and followed that by founding the Anesthesia Clinical Research Unit in 1999. Within the institution’s research community, David has been Associate Dean for Clinical and Translational Research, director of Community Engaged Research, and co-director of the Office for Diversity in Clinical Research. He has been an editor of Anesthesiology and the Journal of Applied Physiology. He was the president of the ABA in 2022 and was recognized by the ASA with its Excellence in Research Award that same year.
David retired clinically in January 2023. He continues as a supplemental consultant, working with department members to write research grant applications and offering his advice and insights to our colleagues with research and career interests. David and his wife, Julie, reside in Rochester. They have three children.
Mystery Photo Contest Winner
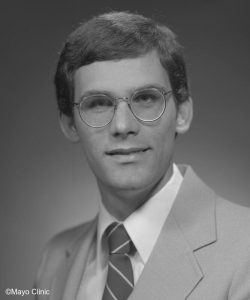
Last week’s contest winner was Philip Boyle.
Here are this week’s Mystery Photos. Reminder: We are now featuring two individuals each week for the Updates. To be placed into the Mystery Photo Starbucks contest, you will need to correctly guess at least one of the featured individuals. If you identify both of them, you will double your chances of having your name drawn.
Please email your response at warner.mark@mayo.edu within 3 days of this update. I will also need your name and contact information. All correct responses will be placed into a Monday morning drawing for a $10 Starbucks card. Only one winner per individual over the 80 weeks of Mystery Photos. If you win a weekly drawing, however, please keep submitting your responses. An overall winner (with the most correct responses in the series of 80 Updates) will receive a $100 Starbucks card.
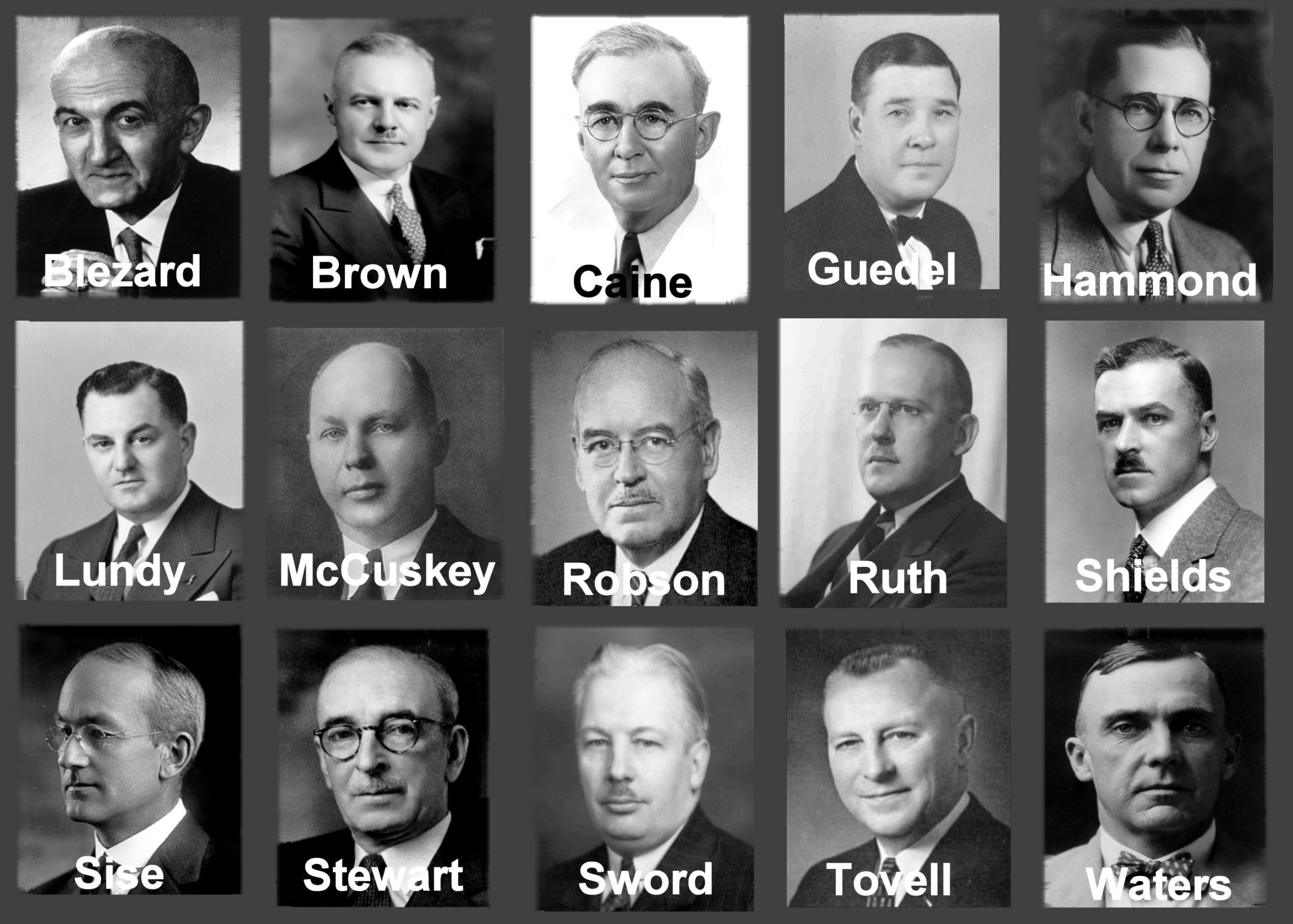
Photograph: Members of the first meeting of the Anaesthetists' Travel Club in 1929.
The Mayo Clinic Department of Anesthesiology: Dr. Lundy, the Anaesthetists’ Travel Club, and the Development of the Specialty
The montage above shows the anesthesiologists who attended the first meeting of the Anaesthetists’ Travel Club. The meeting was held in Rochester in 1929 and was organized by Dr. John Lundy. Drs. Lundy and Ralph Tovell are both from Mayo Clinic. Dr. Tovell was a fellow at the time of the meeting.
Dr. John Lundy was one of the founders of anesthesiology and our department’s first chair. As you have read in previous Centennial Updates, he was a remarkable innovator, clinician, and writer. He also was a dynamic force in organizing physicians who were practicing anesthesia in North America. Mayo alumnus Dr. Doug Bacon, one of the world’s leading anesthesia historians and a former Wood Library Museum History Laureate, has written a wonderful story describing Lundy’s creation of the Anaesthetists’ Travel Club. This club served as the nidus for the foundation of today’s American Society of Anesthesiologists, the American Board of Anesthesiology, and the Academy of Anesthesiology. It’s inaugural meeting was held in Rochester in 1929. A special thank you to Doug for this contribution.
“Working at the Mayo Clinic, Dr. John Lundy had the opportunity to interact with the world’s leading surgeons. When they would come to Rochester as visitors, he’d see them in the operating rooms and field their questions about anesthesia. He also met them in more formal educational activities. For example, he was invited by Drs. Will and Charlie Mayo to a meeting in Rochester of the Society of Clinical Surgery. The society had been founded by the Mayo brothers decades before Lundy’s arrival to Rochester. The society aimed to demonstrate new surgical techniques in the hosts’ “home” hospital. No formal papers were presented, but rather the visitors gathered with the hosts to discuss what they had seen that day over dinner.
Lundy co-opted this educational activity and applied it to anesthesiology by forming the Anaesthetists’ Travel Club. Using a similar approach to Will and Charlie with their Society of Clinica Surgery, he sent invitations to up-and-coming physician anesthesia specialists from across the United States and Canada. Seventeen physicians dared to venture to Minnesota in early winter, arriving in Rochester on December 16th, 1929, for the inaugural meeting. For those from the U.S., Dr. Arthur Guedel traveled from Los Angels, California, Dr. Robert Hammond from White Plains, New York; Dr. Brian Sword from New Haven, Connecticut; Dr. Lincoln Sise (the “old man” at 55 years of age) from Boston; Dr. Ansel Cain from New Orleans; Dr. Henry Ruth from Philadelphia; and Dr. Ralph Waters from nearby Madison, Wisconsin. Canada was well represented with Dr. John Blezard from Edmonton; Drs. Eason Brown, Charles Robson, and Harry Shields from Toronto; and Dr. Charles Stewart from Montreal.
The group toured many of the unique features of Mayo Clinic. They spent a day in the operating rooms of St. Marys Hospital watching the administration of spinal anesthesia and ethylene/nitrous oxide anesthesia. Additionally, they witnessed trans-sacral and trans-vertebral blocks as well as the use of sodium amytal. They toured Mayo’s physiology laboratories, watching experiments on mice that were anesthetized with cyclopropane in oxygen. The highlight of the meeting was the concluding evening’s invitation to the Staff Meeting of the Mayo Clinic at the top of the one-year-old Plummer Building. Will and Charlie Mayo addressed the group as did several other members of the staff who presented topics related to anesthesia.
The meeting was a remarkable success, and arrangements were immediately made for additional meetings. The second meeting was held in Madison, Wisconsin in 1930 with Dr. Ralph Waters as host. The Anaesthetists Travel Club would return to Rochester three more times, including the last meeting of the club in 1952.
Through the Anaesthetists’ Travel Club, Lundy nurtured a group of young leaders in anesthesiology. These initial members of the Travel Club would eventually advance the certification process of the New York Society of Anesthetists, transforming the society into the American Society of Anesthetists (ASA, now the American Society of Anesthesiologists). In turn, the ASA worked with other groups and created the American Board of Anesthesiology (ABA) in 1938. Of the original nine ABA directors, only Dr. H. Boyd Stewart of Tulsa, Oklahoma was not an initial member of the Travel Club. He would subsequently be inducted into the club in 1940.
A simple invitation in 1929 from Lundy to aspiring young anesthesiologists to come to Rochester and see new and innovative anesthesia techniques created a powerful cadre of physicians who defined the specialty and determined who was qualified to practice as a anesthesiologist. These advances continue today through the work of the ASA and ABA. The Travel Club was, in part, a casualty of anesthesiology’s success in World War Two. As the discipline expanded rapidly during the war, a new, more dynamic organization was needed. Therefore, in collaboration with Dr. Rolland Whitacre of Cleveland, Ohio, Lundy created the Travel Club’s successor—the Academy of Anesthesiology. The Academy carries on the traditions of the Anaesthetists’ Travel Club in scholarship, leadership, and camaraderie. The Anaesthetists’ Travel Club provides lasting testament to Lundy’s forethought and creativity.”
References:
- Stephen CR. Anaesthestis’ Travel Club 1929-1952 An Historical Review.
- Marsh HM, Stephen CR, Bacon Dr (eds.). The Anaesthetists’ Travel Club—Academy of Anesthesiology 75 Years in Service to This Specialty. The Academy of Anesthesiology. 2004
- Lennon R, Lennon RL, Bacon DR. The Anaesthetists’ Travel Club: an example of professionalism. Journal of Clinical Anesthesia 2009; 21:137-142.
- The Collected Papers of John S. Lundy. Mayo Foundation Archives. Rochester, Minnesota
- Bacon DR. The Second Anesthetists' Travel Club Meeting: Bootleggers, Madison and Ralph Waters!, Journal of Anesthesia History, 2019; 5(4): 141-144 PMID: 31735279 https://doi.org/10.1016/j.janh.2019.02.002
- Staff Meetings of the Mayo Clinic Wednesday December 18, 1929. Proceedings of the Staff meetings of the Mayo Clin. 1929; 4(51):Sup I.365-416
Mystery Photos
Last week’s Mystery Photos were Ralph T. Knight, M.D. and Mark T. Keegan, M.D.
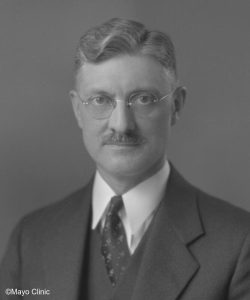
Ralph T. Knight, M.D. was a 1912 graduate of the University of Minnesota School of Medicine. He subsequently trained in surgery at that same institution and started a general surgical practice in Minneapolis. From 1918 through 1920, Dr. Knight was a surgeon in the U.S. Army and served as an Ambulance Battalion Commander on the front lines of WWI’s battles in northern France. Upon the conclusion of the war, he returned to Minnesota and his general surgical practice. His practice was primarily located in the Minneapolis City Hospital (often called the Minneapolis General Hospital and currently the Hennepin County Medical Center) and affiliated with the University of Minnesota. In 1928, recognizing the need for well-trained nurse anesthetists in the Twin Cities area, he organized and started the Minneapolis School of Anesthesia at the University of Minnesota and Minneapolis City Hospital. Alice Anderson was the nurse anesthetist chosen by him to administer the program.
In 1935, Dr. Knight stepped away from his surgical practice, moved to Rochester, and was trained by Dr. John Lundy. His fellow classmate was Dr. R. Charles Adams. Dr. Adams would join our department as a consultant in 1937 and serve as its chair for a brief time in 1952 and 1953. More on Dr. Adams in a later Mystery Photo.
Dr. Knight left Rochester upon completing his anesthesia training in 1937, returning to Minneapolis and the University of Minnesota as the chair of its Section on Anesthesia. He was an extraordinary advocate for improving anesthesia care in Minnesota and elsewhere. He became the first professor of anesthesiology at the University of Minnesota and wrote extensively on general anesthesia. In 1947, he started the first state society of anesthesiology in the U.S. He was the first president of the Minnesota Society of Anesthesiologists (MSA), assuming that role on December 3, 1947. The MSA became the newly-founded American Society of Anesthesiologists’ first state component society. He advanced to become ASA’s 1953 president.
Dr. Knight was director of anesthesiology at the Minneapolis Veterans Administrative Hospital towards the end of his career. The MSA has a dedicated Ralph T. Knight, M.D. Award to recognize outstanding service to the society. You may read more about Dr. Knight’s career in a summary provided on the website of the Wood Library Museum of Anesthesiology and printed here.

Mark T. Keegan, M.D. was born in Dublin, Ireland on October 7, 1968. He was the first in his family to pursue higher education. His parents worked in industries often associated with his home country - his father, Jim, spent his entire working life at the famous Guinness Brewery, and his mother, Pat, calculated horse-racing bets in a turf accountant (aka bookmaker) office!
Mark attended Trinity College, Dublin, graduating in 1992, the year the university celebrated its 400th anniversary, with the degrees of BA MB BCh BAO. He trained in Internal Medicine in Dublin at St. James's and the Mater Misericordiae Hospitals, passing the exam for Membership of the Royal College of Physicians of Ireland in 1995. As part of that Internal Medicine training, he spent 6 months in 1994 as the second person in a newly established visiting resident program between the Mater Hospital and the Mayo Clinic’s Rochester Internal Medicine residency program. He returned to Ireland for a year to work in anesthesia at the Meath-Adelaide-National Children's Hospital before coming back to Rochester in 1996 to complete an anesthesiology residency and critical care fellowship, the latter as a Special Clinical Scholar. While in training, Mark was a chief resident, received the anesthesiology residency In-Training Examination award, the Critical Care Academic Clinician Award, and, in 1999, the Mayo Brothers’ Distinguished Fellowship Award. This latter award is given to 6 trainees every year selected from across the entire enterprise “in recognition of an outstanding record in clinical performance, humanitarianism and scholarly activity”.
In 1999, Mark became my first hire as a new department chair. He served as a Mayo Clinic Special Clinical Scholar (modification of today’s Mayo Clinic Scholar program) while a fellow in Critical Care Medicine during 2000. Since joining the staff in December 2000, he has divided his time between the intensive care units at both campuses in Rochester and the South (now Jacobson) OR division, though since the COVID-19 pandemic almost all his time has been in the ICUs. Additionally, he spent a decade on the liver transplant team. Although primarily a clinician, Mark gained a Masters Degree in Clinical and Translational Science from Mayo Graduate School in 2011 and has expertise in the use of prognostic scoring systems, writing many papers with the late and much-loved Dr. Bekele Afessa from the Division of Pulmonary and Critical Care Medicine. His exceptional article on a novel severity of illness scoring system may be found here. Additionally, prompted by his thoracic surgical ICU experience, Mark mentored critical care fellow Evans Fernandez on a widely cited study that demonstrated the importance of intraoperative tidal volume on the incidence of post-pneumonectomy respiratory failure, leading to significant changes in clinical practice. For those readers who worked with Dr. Afessa, a memorial article about him can be found here.
Starting as a critical care medicine question writer in 2007, Mark has ascended through the ranks of the American Board of Anesthesiology (ABA), serving on multiple committees, as an APPLIED examiner and, since 2016, as a Director. He is currently the Treasurer of the ABA and will assume the ABA Presidency in October 2025, as the second non-North American born president of that organization (Dr. Suresh Santhananam of Chicago has been the other). During the COVID-19 pandemic, he chaired both the ABA Assessments Committee and the ABA Task Force on the Virtual APPLIED examination, leading the development and delivery of a remote form of the final certifying examination to more than 3000 candidates in 2021 to allow career progression when in-person examinations were cancelled. In addition to his ABA work, extramurally, Mark has served as Chair of the American Board of Medical Specialties Ethics and Professionalism Committee and as associate editor-in-chief of the American Society of Anesthesiologists ACE Program.
Mark and his wife, Patricia, who is also from Ireland and is a highly respected pediatric clinical nurse specialist (CNS) at Mayo Clinic, have two high-school age children.
Mystery Photo Contest Winner

Last week’s contest winner was Nicole Andrijasevic.
Here are this week’s Mystery Photos. Reminder: We are now featuring two individuals each week for the Updates. To be placed into the Mystery Photo Starbucks contest, you will need to correctly guess at least one of the featured individuals. If you identify both of them, you will double your chances of having your name drawn.
Please email your response at warner.mark@mayo.edu within 3 days of this update. I will also need your name and contact information. All correct responses will be placed into a Monday morning drawing for a $10 Starbucks card. Only one winner per individual over the 80 weeks of Mystery Photos. If you win a weekly drawing, however, please keep submitting your responses. An overall winner (with the most correct responses in the series of 80 Updates) will receive a $100 Starbucks card.

Photograph: Albert Faulconer, M.D., Jr., served on the institution’s single Board of Governors from 1963 through 1969 and was the first anesthesiologist chosen for Board membership.
The Mayo Clinic Department of Anesthesiology: Contributions to the Mayo Board of Governors and Trustees
Within the institution, the Mayo Clinic Board of Governors has traditionally overseen the organization’s functions. Until the sites in Jacksonville (1986) and Scottsdale (1987) were started, a single Board of Governors directed all institutional initiatives. With the opening of these sites beyond Rochester, each developed its own Board of Governors. They were overseen in a matrix administrative structure led by a Mayo Foundation Chief Executive Officer and a Chief Administrative Officer.
For much of the first two and a half decades of “Mayo Clinic,” Will and Charlie Mayo were responsible for the organization and made the major decisions. By 1919, they had decided that the Mayo Clinic would not continue into the future as a family organization but instead as a public trust. To achieve this, an oversight board was required. Therefore, the Mayo Clinic Board of Governors, that may or may not include a Mayo family member, was appointed.
There is conflicting information on when the Board of Governors first started. In a 1954 Mayovox article, it describes in detail the development of a Mayo Clinic Board of Governors in the early 1920s. The first members were elected on November 21, 1921. So far, so good. However, other articles refer to what appears to be the Board of Governors as the Mayo Clinic Board of Trustees. It isn’t entirely clear but a Board of Trustees appears to have been the term used for the oversight board that included public members as well as physicians and administrators from within Mayo Clinic. For example, Robert C. Roesler, chairman of the Mayo Clinic’s Department of Administration and vice-chairman of its Board of Trustees, wrote in 1981 that the organization was overseen by a Board of Trustees, with public members, in elected.
The leadership board of Mayo Clinic has fluctuated over time as the organization has grown, expanded geographically, added non-clinical subsidiaries, and transitioned from a single Rochester organization to a vast network that expanded around the world. For the purposes of this Centennial Update, we will refer to a Mayo Clinic Board of Governors that has functioned since 1919. The Mayo Clinic was reorganized in 1970 into the Mayo Foundation, and it is clear that a unique Board of Trustees was well established by that time. A U.S. president, Lyndon B. Johnson, and a U.S. vice-president, Walter Mondale, have served on the Board of Trustees as well as numerous remarkable governmental, industrial, financial, technologic, and societal leaders.
With the 1970 reorganization into a foundation, the new Bylaws stipulated that there must be internal members of the Board of Trustees and as many, plus two, public members. Today, the Board of Trustees continues to have a majority of public members. Also, since 1970, a public member has served as chair of the Board of Trustees. The Board of Trustees in 1970 was used primarily to provide advice to the physician and administrative leaders of the Mayo Clinic. Over time, and particularly since 2010, it has evolved as the authority body of the institution, approving all institutional major policies and budget and capital funding decisions.
With expansion of Mayo Clinic from Rochester to Arizona, Florida, and the Mayo Clinic Health System in the last 15 years of the 20th century, the Mayo Clinic Boards of Governors in the Midwest (Rochester and the Mayo Clinic Health System), Arizona, and Florida and their oversight responsibilities continued until 2005 when they were merged into a single institutional Board of Governors. This single Board coordinates efforts across an integrated institution. However, there remain site responsibilities. From 2005 through 2012, these were the responsibility of site Executive Boards. In 2012, these Executive Boards evolved into Executive Operations Management Teams. These leadership groups continue to evolve, changing names and occasionally responsibilities.
Our Department of Anesthesiology has been well represented on these Boards and Management Teams during the past half century. Members of our department who have served on these Boards have provided distinguished service to the institution and the department. They include:

Albert Faulconer, M.D., Jr. Dr. Faulconer served on the institution’s single Board of Governors from 1963 through 1969 and was the first anesthesiologist chosen for Board membership.
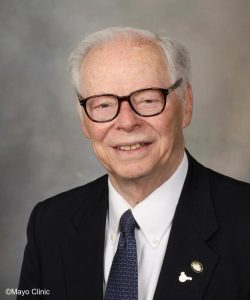
Alan D. Sessler, M.D. Dr. Sessler served on Rochester’s Board of Governors from 1989 through 1994. He also served on the Board of Trustees in 1992 and 1993.

Mark A. Warner, M.D. Dr. Warner served on Rochester’s Board of Governors from 1999 through 2005, its Executive Board from 2006 through 2012, and its Executive Operations Management Team from 2012 through 2016.

Leslie N. Milde, M.D. Dr. Milde served on the Arizona Executive Board from 2005 through 2010. She also served on the Board of Trustees from 2006 through 2010.
Mystery Photos
Last week’s Mystery Photos were Jeff T. Mueller, M.D. and Roy A. Greengrass, M.D.

Jeff T. Mueller, M.D. was born on December 31, 1963 in Wichita, Kansas and raised in central Kansas in Salina. He was the first in his family to graduate from college and pursue a professional education. His parents were both raised on small farms. His father’s lifetime occupation was coast-to-coast truck driving. His mother often worked as a part-time secretary and bookkeeper for small businesses. All members of the family helped with the grandparents’ small farms in the summertime.
Jeff completed undergraduate education at the University of Tulsa where he received a Bachelor of Science in Mechanical Engineering in 1986. After graduation he worked as an engineer in the propulsion engineering section of Martin Marietta Aerospace, specifically in the areas of fluid mechanics, heat transfer, and thermodynamics. Jeff entered the Washington University School of Medicine in St. Louis, Missouri in 1989. He graduated from medical school in 1993, followed by an internship in internal medicine and a residency in anesthesiology at Mayo Clinic in Rochester and Scottsdale, Arizona. Upon completion of residency training in 1997, Jeff joined the staff of Mayo Clinic in Arizona. He moved to a private practice in his hometown of Salina, Kansas in 1999 and 2000 and then returned to the staff at Mayo Clinic in Arizona.
Jeff’s practice leadership contributions include serving as the Medical Director of Perioperative Services in Arizona, Medical Director of the Mayo Clinic Hospital in Arizona, and Chair of the enterprise Hospital Practice Subcommittee. During his time as Mayo’s Chair of Hospital Practices, he led the successful enterprise-wide central line standardization and hospital mortality improvement projects which were reported in peer-reviewed publications. Jeff helped re-initiate publication of Faust’s Anesthesiology Review with its fourth edition and has served as an associate editor of the fourth, fifth and sixth editions. During the Covid pandemic, Jeff revived his engineering background and collaborated with faculty at his undergraduate alma mater to successfully research and report on the N95 respirator leakage risks associated with double masking.
Jeff has served as president of the Arizona Society of Anesthesiologists, president of the Arizona Medical Association, and a member of the Arizona Hospital and Healthcare Association Board of Directors. He has also served in many American Society of Anesthesiologists’ leadership roles. These include his service as Vice President for Professional Affairs and Chair of the ASAPAC Executive Board. He is a tireless contributor to these organizations. He has been recognized for his efforts by the Arizona Medical Association with its National Leadership Award (2013), the Arizona Society of Anesthesiologists’ Distinguished Service Award (2023), and the American Society of Anesthesiologists’ Bertram W. Coffer Excellence in Government Award (2015).
Jeff resides in Scottsdale, Arizona with his spouse, Eileen Klein.

Roy A. Greengrass, M.D. was born on January 19, 1948 in Winnipeg, Manitoba. He graduated from the Department of Medicine, University of Manitoba in 1973 receiving BSc Med and M.D. degrees. His early career involved caring for patients in a busy family practice in rural Manitoba where, besides primary care, he performed obstetrical, surgical and critical care procedures. He returned to the University of Manitoba to complete an anesthesiology residency and received the Fellow of the Royal College of Medicine and American Board of Anesthesiology certification. During his residency Roy had the privilege of being mentored by internationally recognized leaders in anesthesiology, including Dr. Shinman Liu and Dr. Y.K. Poon (a fellow of Sir Robert McIntosh) who molded Roy’s future career by demonstrating regional anesthetic techniques that allowed major procedures to be safely performed in awake patients.
After completing his anesthesiology training, Roy joined the Department of Anesthesiology Health Sciences Center Winnipeg as a consultant. Roy was an avid reader and interested teacher who helped develop a regional anesthesia curriculum, including cadaver workshops. He helped incorporate regional anesthetic lectures into Grand Rounds and invited internationally recognized leaders in regional anesthesia as lecturers.
In 1992, he was recruited to Duke University by Dr. Jerry Reves to join an internationally recognized regional anesthesia division led by Dr. Susan Steele. Roy helped create a weekly problem-based learning lecture which was very popular with the residents. The Duke team helped create the country’s first resident regional anesthesia rotation that did not involve an operating room commitment. With Dr. Steele, Roy helped create a Regional Anesthesia Fellowship at Duke which remains very popular today. Dr. Steele and Roy were among the first in the world to send patients home with indwelling regional catheters, several of which were designed by them.
We are fortunate that Roy was recruited to Mayo Clinic Florida in 2001 by Dr. Tim Lamer to assist with the regional anesthesia practice. He has helped introduce additional regional techniques such as paravertebral blocks which have helped facilitate ambulatory discharge after major breast procedures. Roy also assisted in the increased number and complexity of continuous regional techniques in our Florida practice and contributed to the literature on their advantages. He was part of the creation of a Regional Anesthesia Fellowship at MCF and was its inaugural director. With assistance from the Department of Nursing in Jacksonville, Roy helped create a hospital ward-based low-dose ketamine service to assist patients on chronic opioids having major procedures.
Roy mentored numerous residents and fellows, many who currently hold academic positions nationally and internationally. He continues to be actively involved in clinical and academic practice. His research interests involve methodologies to attenuate chemotherapy-induced peripheral neuropathy and the use of local anesthetics as potential chemotherapy adjuvants. He notes that he is privileged to work with gifted regional anesthesiologists and CRNA’s in our Florida practice. He has received Educator of the Year Awards at Winnipeg, Duke, and Jacksonville. In 2001, the American Society of Regional Anesthesia recognized his contributions to regional anesthesia and pain medicine with its Nils Löfgren Award.
Roy has five children. During his leisure time he enjoys running, kickboxing, The Bard, Beethoven and Newton.
Mystery Photo Contest Winner
Last week’s contest winner was Steven Porter.

Here are this week’s Mystery Photos. Reminder: We are now featuring two individuals each week for the Updates. To be placed into the Mystery Photo Starbucks contest, you will need to correctly guess at least one of the featured individuals. If you identify both of them, you will double your chances of having your name drawn.
Please email your response at warner.mark@mayo.edu within 3 days of this update. I will also need your name and contact information. All correct responses will be placed into a Monday morning drawing for a $10 Starbucks card. Only one winner per individual over the 80 weeks of Mystery Photos. If you win a weekly drawing, however, please keep submitting your responses. An overall winner (with the most correct responses in the series of 80 Updates) will receive a $100 Starbucks card.

Photograph: A look at the new exhibit at the International Museum of Surgical Science that highlights the first 100 years of the Department of Anesthesiology and Perioperative Medicine, August 15, 2024.
First, An Apology: Dr. Brad Narr and the Rochester Executive Operations Team
Update #49 (August 15, 2024) highlighted members of the department who had served on the Mayo Clinic’s highest governing boards (i.e., the Board of Trustees, the Board of Governors, the site Executive Boards, and the Executive Operations Teams). As the governing boards have evolved, especially in the past two decades, their names have changed frequently. With these transitions, I failed to highlight Dr. Brad Narr as one of our members who has served at the highest levels of the institution. Brad served on the Rochester Executive Operations Team from 2005 through 2014 and its successor, the Midwest Executive Operations Team, from 2014 through 2021. As noted earlier in a summary about him in Update #41 on June 13, 2024, Brad also is the only non-surgeon who has ever chaired the Rochester Surgical Committee (now known as the Surgical and Procedural Committee).

The Mayo Clinic Department of Anesthesiology: The International Museum of Surgical Science
Our department was invited late last year by the International Museum of Surgical Science (IMSS) to develop an anesthesiology exhibit that would showcase our Centennial Celebration as well as the overall field of anesthesiology. The IMSS is a foundation of the International College of Surgeons. Its museum is housed in a spectacular facility on Lake Shore Drive in downtown Chicago. It is located adjacent to the Water Tower District and is an easy walk from the north end of Miracle Mile. More than 50,000 visitors pass through its exhibits annually. You may read more about the museum at Best Museum Chicago - Things to Do in Chicago - International Museum of Surgical Science (imss.org).
A team consisting of Dr. Doug Bacon, Alec Thicke (our archivist), Renee Ziemer (Historical and Heritage Program Manager at Mayo Clinic), and me developed the exhibit. Its grand opening was this past Thursday, August 15th and the exhibit will be present for a year. You may read more about it at 100 Years of Innovation: Mayo Clinic and the History of the Specialty of Anesthesiology - International Museum of Surgical Science (imss.org). Over time, additional content will be added to the IMSS webpages associated with our exhibit. One of the first pages describes the contributions of our early nurse anesthetists (Nurse Anesthetists at the Mayo Clinic (imss.org).
We are very proud to be the first institution and department to represent the field of anesthesiology in the museum. In the coming weeks, we’ll add material and photos about the exhibit to our Mayo Clinic Anesthesiology History website (Anesthesiology Department | Mayo Clinic | History and Heritage). If you are in downtown Chicago between now and August 2025, please stop by the IMSS’s remarkable museum and visit our exhibit. The address is 1524 North Lake Shore Drive in Chicago. I believe you will be proud to see our department showcased there. Below you can see some photographs taken from the opening.

- Dr. David Martin, host of the opening ceremony for the exhibit.

- Visitors to the exhibit.

- A well-recognized Mayo wax model demonstrating potential regional blocks.

- Our archivist, Alec Thicke, addressing attendees at the opening ceremony.

- Dr. Doug Bacon, former Wood Library Museum History Laureate and Mayo staff member, highlighting the contributions of our department to the development of the specialty.
Mystery Photos
Last week’s Mystery Photos were Maurice Albin, M.D. and Marlea A. Judd, CRNA, DNP.

Maurice S. Albin, M.D. was born on March 18, 1923, in Brooklyn, New York. After graduating high school in 1941, he joined the U.S. Army and served in the European theater during World War II. He was an infantry medic at the Battle of the Bulge. Upon returning from the war, he entered New York University and graduated in 1952. He attended medical school at the Universidad Nacional Autonoma de Mexico in Mexico City where he earned his M.D. He moved to Rochester in 1960 as a resident in anesthesiology with classmates such as Drs. Alan Sessler and Martha Smith (Mrs. Alan Sessler). He completed his training in 1962.
Dr. Albin moved to Case Western Reserve University. At that institution, he worked extensively with Dr. Robert White, a neurosurgeon widely known for attempting total head transplants in primates (Robert J. White - Wikipedia). Ironically, I heard Dr. White present this astonishing work at a meeting of the Ohio Athletic Trainers Association in Springfield, Ohio in 1975. It was at this meeting that I first learned of Dr. Albin. Although head transplantation was unsuccessful (and Dr. White was branded as “The Butcher” by several animal rights groups), the two were nominated for the Nobel Prize twice (2004 and 2010) for their work in limiting spinal cord deterioration in injury with hypothermia. Dr. Albin moved to the University of Pittsburgh, then to the University of Texas San Antonio, before settling into the University of Alabama in Birmingham.
Dr. Albin was a pioneer in neuroprotection and understanding of the biomechanics of spinal cord injury. His work on cerebral blood flow, spinal cord ischemia, and venous air embolism led to several innovations and modifications to anesthesia practice. He played a primary role as a founder of the Society of Neuroscience in Anesthesiology and Critical Care (SNACC) and was the society’s second president and recipient of its Distinguished Service Award. An excellent summary and thoughtful reflections on his impact on neuroprotection and the establishment of the field of neuroanesthesiology was written by Dr. Andy Kofke in 2016 upon Dr. Albin’s death).
As an accomplished story-teller who was an experienced battlefield Army medic in World War II, Dr. Albin loved to study and write about anesthesiology’s initial use in the U.S. Army during the Civil War. He became one of the country’s leading authorities on that topic. His article in the ASA Monitor in 2014 is a remarkably interesting summary of Civil War anesthesiology.
Dr. Albin was married to the love of his life, Marguerite, for more than 70 years. They had three children and six grandchildren when he died on July 2, 2016.

Marlea A. Judd, CRNA, DNP was born in Huron, South Dakota and spent most of her childhood years in very small rural towns in South Dakota and Nebraska. She attended Mount Marty College in Yankton, South Dakota to obtain her nursing degree and was introduced to Mayo Clinic recruiters at the school. She gambled on a big move and the prairie winds blew Marlea to Rochester in August 1983.
Marlea started in the old 4 Mary Brigh critical care unit on the St. Marys Campus and was scared straight by the high patient acuity and the level of complicated surgical patients that Drs. Frank Sims (orthopedic oncology), Peter Pairolero (thoracic surgery), Mike Farnell (emergency surgery), Larry Hollier (vascular surgery) and many other trauma/thoracic/vascular surgeons would send there. Over the next couple of years, she thrived, became the unit’s Charge Nurse and started to consider new opportunities. She was always impressed with the nurse anesthetists who brought patients back from surgery. She contacted Don Nelson, our lead CRNA on the St. Marys campus, and asked to shadow a nurse anesthetist.
After that one experience, she was convinced to enter our training program. Marlea graduated in February 1988. At that time, there were 6 students per class. The school started 2 classes per year. Two of her classmates, Mavis Ward and Mark Solomonson, spent their careers in Rochester. After graduation, Marlea joined our department with a Rochester Methodist position and eventually found her “home” working with pediatrics, EENT, and oral surgery. During her initial years on staff she worked closely with Drs. Allan Gould and Ron Mackenzie and nurse anesthetists Marilyn Crawford, Merry Milverstedt, and JoAnn Haebig. She completed her Master of Science degree from our nurse anesthesia training program in 2001. Marlea was selected as a supervisor for the Methodist Hospital South Division, St. Marys Hospital Cardiac and Vascular Procedural Center, and Obstetric Anesthesia that same year.
In 2001, Drs. Mark Warner and Brad Narr and Rochester CRNA Director Steve Osborn announced the creation of an outpatient procedural practice in the new Gonda Building. Dr. Warner, chair of the department, asked Marlea to team with Dr. Mary Ellen Warner, Dr. Narr, administrator Steve Jorgensen, and Steve Osborn to design, develop, and operationalize a totally new practice model for what was to become the Gonda 7 Outpatient Procedure Center. The unit was built with safety, efficiency and patient satisfaction top of mind. The unit was unique as all employees (e.g., core nursing staff, surgical staff, and technical support staff) were employed by the Department of Anesthesiology. The all-RN model of care provided surprising flexibility and outstanding expertise for the unit’s varied roles. It was a huge success for the department as well as the patients. The overall practice and business models from that initial Gonda 7 Outpatient Procedural Center has been replicated in many parts of the institution and around the world.
The “outfield” or Non-Operating Room Anesthesia (NORA) practices in Rochester grew 20% annually in the first decade of the century. Marlea and Dr. Mary Ellen Warner established the RN and CRNA Bedside Sedation Team in 2011 to provide safe sedation care to inpatients and decrease the need to bring these patients into the OR. It also was remarkably successful and emulated across the country.
When Steve Osborn, past CRNA Director (1994-2011) retired, the Rochester department had grown to 205 nurse anesthetist full-time equivalents. Two CRNA Directors were now needed to support the practice. Marlea and Jean Guyer, CRNA, DNP were selected for the new positions in 2011 and they continued to grow the nurse anesthesia staff. They faced challenges with introducing and implementing programs and protocols such as QGenda (a scheduling system), EPIC (an electronic medical record), Hemosafe (automated blood distribution system), and standardized glycemic control protocols. It was a busy time, and Marlea, Jean, and the entire department fared well.
In 2014, Dr. Brad Narr, now the Rochester department chair and also the chair of the Mayo Clinic’s Midwest Surgical and Procedural Committee, shared the need for complete anesthesia integration into the Mayo Clinic Health System (MCHS). Dr. Jim Hebl and Marlea were selected to lead that venture. They started by visiting the 18 MCHS sites existing at that time to see how the Rochester department could help them with equipment, resources, or governance to support the institution’s mission and vision. It was a new adventure to learn all of the different struggles and accomplishments that faced these important MCHS sites. When Dr. Hebl moved in 2016 to Mankato to serve as Mayo’s Regional Vice-President for MCHS Southwestern Minnesota, Dr. Sandy Kopp joined as Marlea’s partner to advance our MCHS community anesthesiology practices. By 2018, the MCHS and Rochester practices were both major entities so Marlea transitioned to solely leading the MCHS nurse anesthetists. In Rochester, the department added Bettina Thompson, CRNA, DNP as a new CRNA Director. At that time, there were over 300 nurse anesthetist full-time equivalents in the Rochester practice and 100 of them across MCHS.
Marlea worked at Mayo Clinic for nearly 41 years and retired in April 2024. She lives in Minneapolis and spends time with friends, family, and traveling with her husband, Joe. She continues to advise our department and specifically me as a member of our Centennial Project Team.
Mystery Photo Contest Winner

Last week’s contest winner was Seth Mogler.
Here are this week’s Mystery Photos. Reminder: We are now featuring two individuals each week for the Updates. To be placed into the Mystery Photo Starbucks contest, you will need to correctly guess at least one of the featured individuals. If you identify both of them, you will double your chances of having your name drawn.
Please email your response at warner.mark@mayo.edu within 3 days of this update. I will also need your name and contact information. All correct responses will be placed into a Monday morning drawing for a $10 Starbucks card. Only one winner per individual over the 80 weeks of Mystery Photos. If you win a weekly drawing, however, please keep submitting your responses. An overall winner (with the most correct responses in the series of 80 Updates) will receive a $100 Starbucks card.
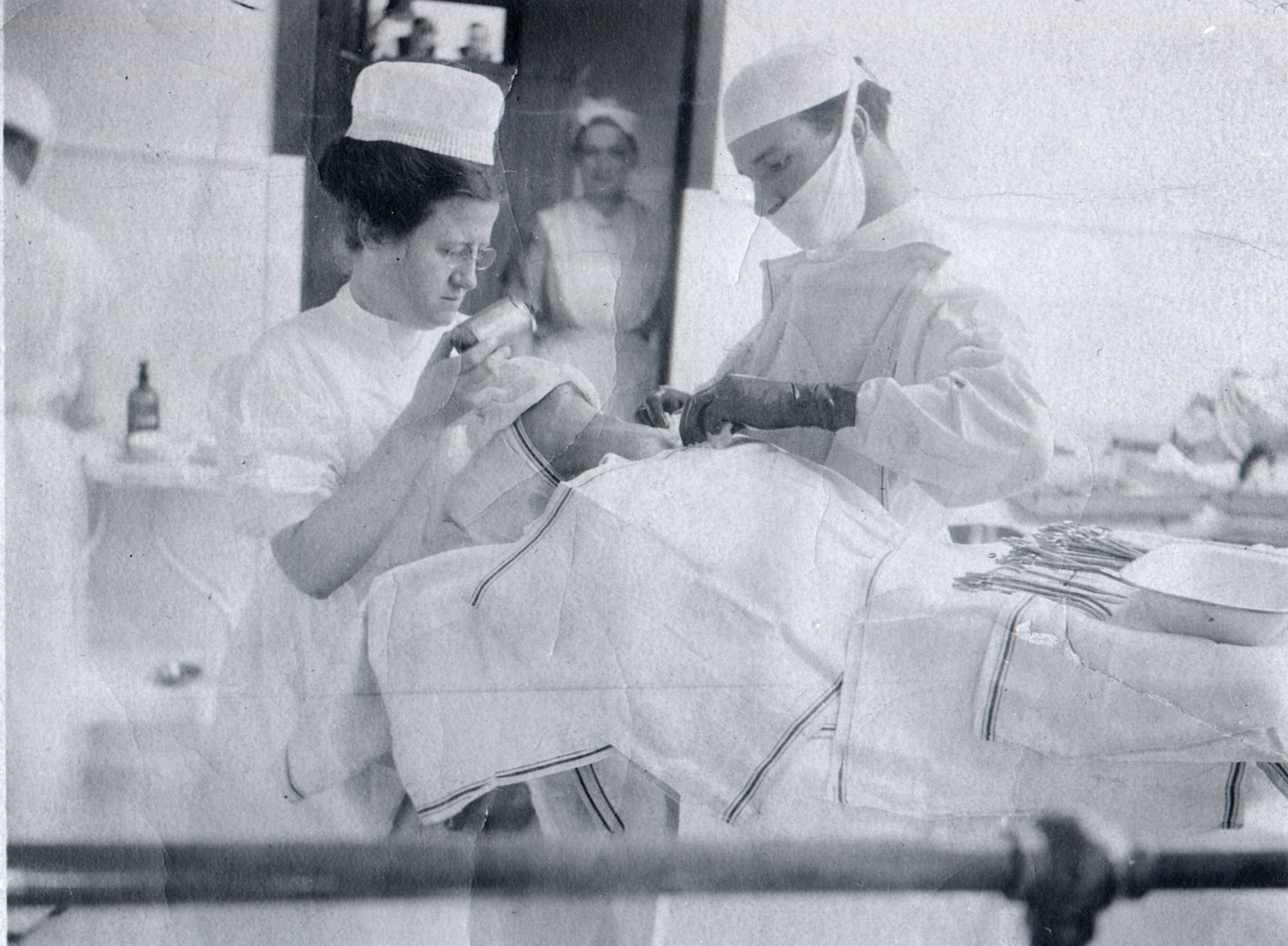
Photograph: Florence Henderson administering ether while Dr. Donald C. Balfour of
Mayo Clinic performs a thyroid surgery, circa early 1900’s. Henderson worked closely with Alice Magaw and published remarkable outcomes for anesthetized Mayo Clinic patients.
The Mayo Clinic Department of Anesthesiology: Two Exceptional Alumni Who Became Leaders of Nurse Anesthesia Nationally and Internationally
Mayo Clinic has been a leader in the development and advancement of nurse anesthesia since Edith Graham first learned to deliver ether anesthesia from William Worrell Mayo in 1889. Examples of key leaders early in nurse anesthesia include:
- Alice Magaw became the “Mother of Anesthesia” and was the first nurse anesthetist to publish in the medical literature.
- Florence Henderson worked closely with Alice Magaw and published remarkable outcomes for anesthetized Mayo Clinic patients.
- Florence McQuillan was Dr. John Lundy’s first chief nurse anesthetist and subsequently the AANA’s first Executive Director, serving 22 years in that role.
The department has continued to be a leader in nurse anesthesia nationally as well as internationally. In this Update, we’ll highlight two of these leaders, Mary S. Marienau, CRNA, Ph.D. and Ronald F. Caulk, CRNA. Both Mary and Ron were highlighted in our department’s 2010-2011 Mayo Nurse Anesthesia Alumni Newsletter. Pages 11 and 12 of the Newsletter showcase an interview of Mary as it was reported in an earlier Minnesota Association of Nurse Anesthetists’ Newsletter. Page 13 describes Ron’s remarkable contributions. Both are enlightening stories, and I encourage you to read them. For our nurse anesthetists who trained or worked in Rochester, the Newsletter also will provide you with engaging photos and notes about many of our colleagues at an earlier time in their careers.

Mary S. Marienau, CRNA, Ph.D. is an outstanding nurse anesthetist and educator. She also is one of my closest friends and colleagues. I had the privilege of first meeting Mary when I was an intern on the Rochester Orthopedic call team in early 1980. Mary had just joined our department as a nurse anesthetist the year before. Unfortunately, she had injured her foot and I was called to the St. Marys Hospital emergency room to place a cast. Let’s just say it didn’t go as well as I had hoped, and Mary had to return to the emergency room the next day to have it removed and replaced. We have shared laughs over that story for the past 44 years.
Fortunately for me, I had the privilege of working daily with Mary for much of my career, starting when we teamed as section chair and supervisor in what was the old Section of General Anesthesia at St. Marys Hospital (now the Division of Multispecialty Anesthesia). Other supervisors in that section at the time included John Carter, Dan Schnell, and Jack Hostak. Mary and I started the pediatric anesthesia group together, were part of our first pediatric solid organ transplant team and are particularly proud of our novel approaches to obtaining airways in children with severe craniofacial malformations. During the 1983 through 1989 period, Mary and our section colleagues provided care for more than 450 infants and children with Pierre Robin and Treacher Collins syndromes, hemi-microsoma, and massive head and neck hemangiomas – and remarkably for those days before pediatric fiberoptic tools were available, never once needed to perform a tracheostomy.
Mary received a nursing diploma from Allen Memorial Hospital School of Nursing (1971), a B.A. degree (1976) from the University of Northern Iowa, a certificate in Nurse Anesthesia from the Mayo Clinic School of Health Sciences Nurse Anesthesia Program (1979), an M.S. degree (1986) from Winona State University, and a Ph.D. degree (2011) in Adult Education from the University of Minnesota. Early in her career she was a nurse at health facilities in Waterloo, Iowa. Mary was appointed a staff anesthetist in the Department of Anesthesiology at Mayo Clinic in 1979 and advanced to a supervisory role in 1982.
She became director of the Nurse Anesthesia Program at Mayo Clinic School of Health Sciences in 1997 and director of the Doctor of Nurse Anesthesia Practice Program at the school in 2017. Mary published extensively and is one of the most cited nurse anesthetists at Mayo Clinic. She advanced to the rank of assistant professor of anesthesiology at Mayo Clinic College of Medicine and Science in 1998. Mary has been active in professional associations and served as an officer and board member of the Council on Accreditation for Nurse Anesthesia Educational Programs. Mary is the recipient of numerous awards, including the Outstanding Educator Award from Mayo Clinic School of Health Sciences and the Outstanding Professional Achievement Award from the Minnesota Association of Nurses Anesthetists. She retired from Mayo Clinic in July 2020 but continues as a member of our department’s Centennial Project team.

Ronald F. Caulk, CRNA was born in Des Moines, Iowa in 1938. He was the first man to graduate from the Mercy Hospital nursing school in Des Moines. Shortly after graduating in 1959, he moved to Rochester as a student nurse anesthetist. Jack Hostak, newly minted CRNA, was a mentor for Ron during his training in our program. Ron graduated in 1962. After several years of work in Ft. Madison, Iowa, Ron moved to the Phoenix area and worked at Casa Grande and Mesa. Ron’s clinical career subsequently took him back to the Midwest , specifically Peoria and Chicago, Illinois.
Ron was an incredibly effective advocate for nurse anesthesia, as was his wife, Susan Smith Caulk, also a CRNA. Ron rose through the ranks of the AANA to become its president in 1977. Susan also worked closely with the AANA, serving as its director of Continuing Education and Certification for many years. While AANA president at the association’s 1978 annual meeting, Ron joined forces with Hermi Löhnert, a Swiss nurse anesthetist, and John Garde, the AANA Executive Director. They decided to initiate an international network for nurse anesthetists, with the first International Symposium to be held in Luzern, Switzerland in 1985. At the second International Symposium held in Amsterdam, The Netherlands in 1988, it was decided to launch an international organization for nurse anesthetists. The International Federation of Nurse Anesthetists (IFNA) was started in June 1989. It is an important organization that is now recognized as the official voice for nurse anesthetists worldwide. Ron served as its first vice-president for a single year, then advanced to President, a role he filled from 1990 through 1995. He also became the IFNA’s first executive director, working in that role from 1994 through 2004.
Ron was the recipient of various awards. In 1992, he received the AANA’s most prestigious honor, the Agatha Hodgins Award for Outstanding Accomplishment. In 1999, he was inducted as a Fellow of the Academy of American Nurses. The next year, he received the Mother McAuley Distinguished Alumni Award from Mercy College, Des Moines, Iowa. In 2002 Ron was awarded the Hermi Lohnert Award for Outstanding Contributions to Nurse Anesthesia Internationally. Finally, in 2011 he received the Mayo Clinic School of Health Sciences Alumni Association’s Recognition of Outstanding Contributions Award.
Ron passed away on April 29, 2016, in Scottsdale, Arizona.
Mystery Photos
Last week’s Mystery Photos were Karl A. Poterack, M.D. and Timothy S. J. Shine, M.D.
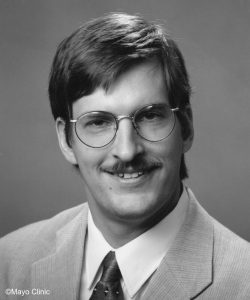
Karl A. Poterack, M.D. was born in Grand Rapids Michigan on March 25, 1961. He received his undergraduate and M.D. degrees from the University of Michigan, graduating medical school in 1985. Karl started in a general surgery residency program at the Medical College of Wisconsin in Milwaukee but after two years realized that he didn't have a particular love for operating and instead enjoyed taking care of sick patients. So luckily there was an open spot in Dr. John Kampine’s anesthesiology residency at the Medical College of Wisconsin and he started his anesthesia training in 1987. After finishing residency and then a neuro-anesthesiology fellowship at Milwaukee in 1991, he was obligated to pay back a military obligation from medical school. He was assigned to Wilford Hall Medical Center in San Antonio, TX where he was a staff anesthesiologist for four years.
After leaving the military in 1995 as an Air Force major, Karl returned to the Medical College of Wisconsin for two years where he was a section chief of anesthesiology services at Froedtert Memorial Lutheran Hospital. He was recruited by our own Dr. Leslie Milde to join the Mayo Clinic Arizona anesthesiology department in 1997. At that time, the department was providing outpatient surgical anesthesia in the Shea Blvd. Clinic Building and providing inpatient care at what was then Scottsdale North Hospital while the new Mayo Clinic Hospital was being completed. After the new hospital opened in 1998, Karl was the anesthesiologist for the first anesthetic given in it and the 1st liver transplant that was performed there in 1999. He was part of the liver transplant anesthesia team for the next 20 years as that program grew to be the largest solid organ transplant program in the U.S.
During his Mayo career, Karl has served in multiple roles, including Director of Quality Improvement for the department, Medical Director of Surgical Services, chair of the Mayo Clinic Arizona Accreditation and Regulatory Subcommittee through 4 cycles of Joint Commission surveys, as well as Medical Director of Clinical Informatics in the institution’s enterprise-wide Center for Information and Knowledge Management. In 2014, he became board certified in Clinical Informatics, one of the first anesthesiologists in the initial group of physicians nationwide to be boarded in this new specialty.
Karl and his wife, Stephanie, have 4 children ranging in age from 36 to 9, and a 3-year-old grandson. They live in Phoenix with their youngest son, Carson. In Karl’s spare time, he enjoys travel and photography.

Timothy S. J. Shine, M.D. was born in Dublin, Ireland on September 1, 1953. He earned the degrees of B.A. and M.D. in 1979 from Trinity College in Dublin. After completing an internship at St. James Hospital in Dublin (1979-1980), he moved to Rochester and was a resident in anesthesiology from 1980 through 1984. Tim also served here as a fellow in cardiovascular/thoracic anesthesia and pain clinic/regional anesthesia during the 1984-5 academic year. After working one year at the Carle Clinic in Champaign-Urbana, Illinois, Dr. Alan Sessler, the Rochester department chair at the time, recruited Tim to join Dr. Jim Harper as the first two members of our nascent Department of Anesthesiology in Jacksonville.
Tim served as chair of the Division of Liver Transplant Anesthesia in Jacksonville from 2006 through 2017 and was a member of numerous administrative committees. Examples include membership on the Mayo Clinic Florida Clinical Practice Committee, Surgical Committee, and Pharmacy & Therapeutics Committee. His special interests included cardiovascular anesthesia, transplant anesthesia, and intraoperative transesophageal echocardiography. He is the recipient of two Teacher of the Year awards from our Department of Anesthesiology at Mayo Clinic in Florida.
During his Rochester training, Tim participated in a number of laboratory and clinical trials, working with mentors and colleagues such as Drs. Mike Nugent, Mike Murray, and Dave Plevak. His participation in scholarly publications continued in Florida. He co-authored papers on diverse topics ranging from spinal cord preservation techniques during thoracic and upper abdominal vascular procedures and solid organ transplant anesthesia to the use of perioperative echocardiography. His co-authors in Florida included close friends such as Drs. Neil Feinglass, Wolf Stapelfeldt, Dave Mackey, Roy Greengrass, Sorin Brull, Steve Aniskevich, Claudia Crawford, Bruce Leone, Archer Martin, Sher-Lu Pai, and Steve Clendenen. He is extraordinarily proud of the efforts and expertise of his colleagues as they worked together to develop one of the country’s largest and most successful solid organ transplant programs and the anesthesia teams that have supported them. Tim retired in 2018 after having served in our Florida department’s first 32 years.
Tim and his wife, Marsha, have two children. They continue to reside in Jacksonville and enjoy hiking. They also are proud fans of the Jacksonville Jaguar (NFL).
Mystery Photo Contest Winner

Last week’s contest winner was Sandra Sanchez.
Here are this week’s Mystery Photos. Reminder: We are now featuring two individuals each week for the Updates. To be placed into the Mystery Photo Starbucks contest, you will need to correctly guess at least one of the featured individuals. If you identify both of them, you will double your chances of having your name drawn.
Please email your response at warner.mark@mayo.edu within 3 days of this update. I will also need your name and contact information. All correct responses will be placed into a Monday morning drawing for a $10 Starbucks card. Only one winner per individual over the 80 weeks of Mystery Photos. If you win a weekly drawing, however, please keep submitting your responses. An overall winner (with the most correct responses in the series of 80 Updates) will receive a $100 Starbucks card.
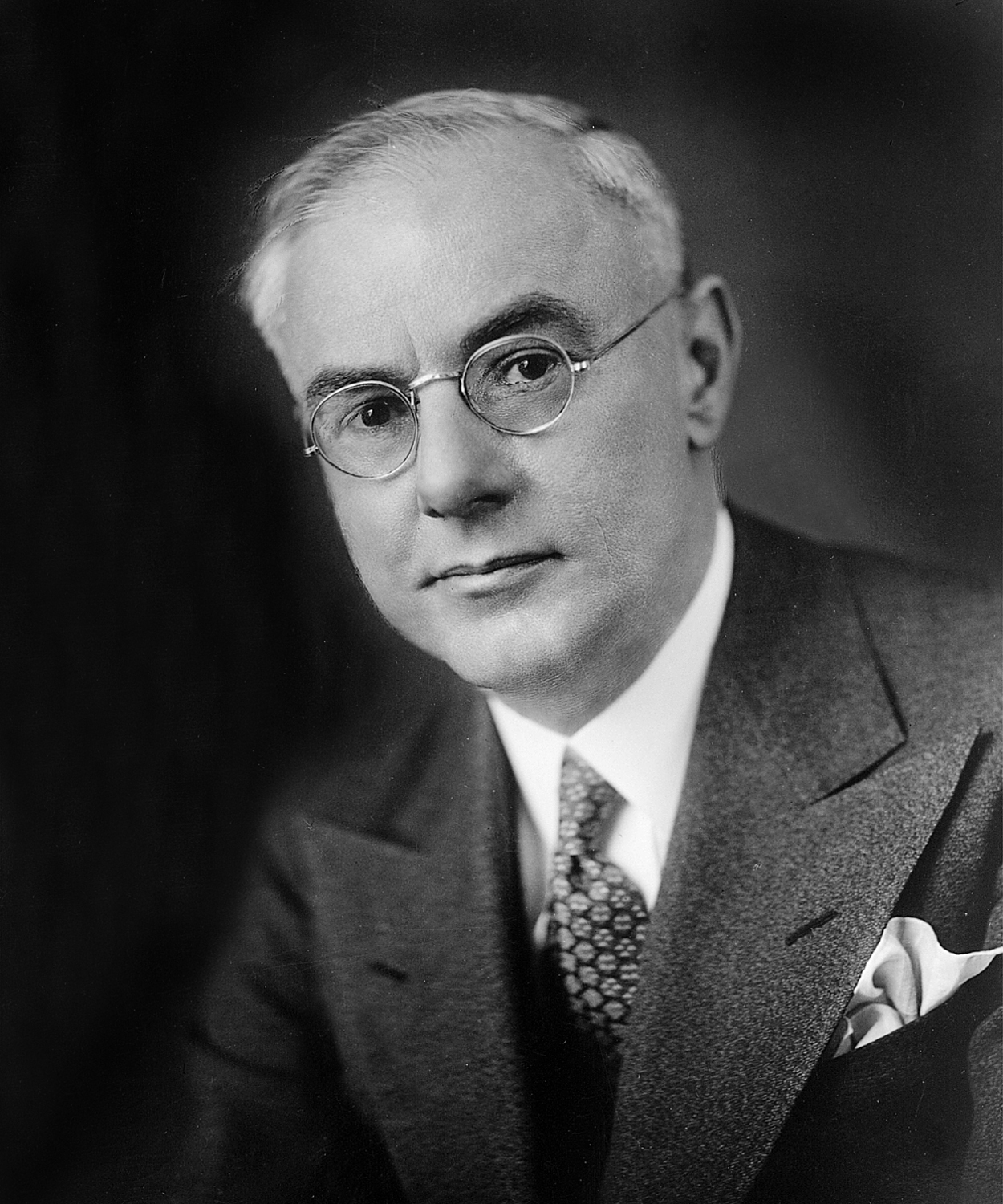
The Mayo Clinic Department of Anesthesiology: The Beginning of Intensive Care in Rochester
Prior to 1940, there was no respiratory or inhalation service at Mayo Clinic. Dr. Walter M. Boothby, an anesthesiologist who spent much of his career in the field of respiratory physiology and basal metabolism, was recruited to Rochester soon after the conclusion of World War I. He established Mayo’s Metabolic Laboratory and started oxygen therapy for Mayo patients. In 1940, he recruited Dr. H. Frederic Helmholz, Jr. a physician and physiologist, to join him in the laboratory and assume leadership in oxygen therapy. This relationship between Drs. Boothby and Helmholz served as the starting point for the development of respiratory and intensive care at Mayo Clinic in Rochester. It expanded slowly and coincident with the introduction of positive pressure ventilators and other innovations. In 1966, Mayo Clinic officially approved the development of respiratory intensive care units at both Rochester Methodist and St. Marys Hospitals.
Today’s story will highlight these 2 key leaders who started what was to become respiratory care at Mayo Clinic. They were remarkable stars in the fields of medicine and physiology, and their combined efforts established what has become one of the country’s leading institutions in critical care medicine. Future Update articles will describe the development of intensive care and respiratory care.
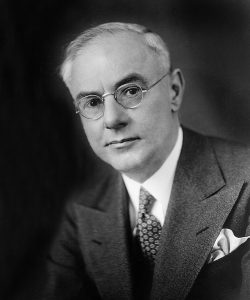
Walter M. Boothby, M.D. was born in Boston on July 28, 1880. After graduating from Harvard Medical School in 1906, he continued his training in Boston. He served as a physician anesthetist in Boston City Hospital in 1912 under the supervision of Dr. Fred Cotton. During that year he and Dr. Cotton devised the Cotton & Boothby anesthesia apparatus, a precursor to today’s anesthesia machines (Cotton & Boothby Apparatus - Wood Library-Museum of Anesthesiology (woodlibrarymuseum.org). Dr. Harvey Cushing, renowned surgeon at Peter Bent Brigham Hospital, learned of Dr. Boothby’s anesthesia interests and in late 1912 invited him to be the supervisor of anesthesia in his hospital. However, he first arranged for Dr. Boothby to spend a year in Oxford, England with Dr. J.S. Haldane studying basal metabolism, including the measurement and metabolism of gases such as ether. Upon his return to Boston in late 1913, Dr. Boothby expanded on Dr. Cushing’s concept of an anesthesia record. Dr. Cushing had previously developed and advocated for the use of an anesthesia record and the concept of minute-by-minute monitoring of patients with blood pressure measurement and auscultation of breath and heart sounds by precordial stethoscope. Dr. Boothby added the measurement and recording of inhaled anesthetic concentrations, primarily ether at that time, a monitoring addition that is now standard for all anesthetic documentation.
Dr. Boothby was very interested in anesthetic uptake and metabolism as well as other metabolic measurements. His work with basal metabolism attracted the attention of Mayo Clinic’s Dr. Henry Plummer. Dr. Plummer recruited Dr. Boothby to move to Rochester and establish a metabolic laboratory. His arrival was delayed by World War I during which time he was assigned a major role with improving the masks used by front line soldiers to avoid poisoning with chlorine, phosgene, and mustard gases. After the war and upon his move to Mayo Clinic, Dr. Boothby established Mayo’s Metabolic Lab. His subsequent work set the worldwide standards for measuring metabolic needs in health and various disease states, including thyroid disorders and diabetes. He did not work in clinical anesthesia while at Mayo Clinic. However, he did work with Dr. Plummer on understanding postoperative hypoxia and had a lead role in arranging for oxygen to be provided to hypoxic postoperative patients. As of this writing, Dr. Boothby does not appear to have worked with Dr. Lundy or other Mayo anesthesiologists before World War II. However, he did collaborate with anesthesiologists such as Dr. Albert Faulconer after the war.
The mid-1930s were a remarkable time in aviation history as planes were designed that could reach more than 10,000 feet in altitude. Flight into the upper heights presented problems with oxygen supply and metabolic needs. With trouble brewing in Europe and the potential need for high altitude military aircraft and with the support of Drs. Will and Charlie Mayo in their final years, Dr. Boothby established the Mayo Aero-Medical Unit in conjunction with colleagues Drs. Earl Wood, Randolph Lovelace, Art Bulbulian, and others. Dr. Bruce Fye, famed Mayo cardiologist and historian, describes this unit and its contributions to the military in an excellent summary found on our institution’s heritage website (Top Secret: Mayo Aeromedicine and Operation Paperclip - W. Bruce Fye Center For the History of Medicine - Guides at Mayo Clinic). The team studied the physiology of high G-forces and oxygen delivery to aviators in freezing, low oxygen altitudes, resulting in the development of G-suits (compression devices), the use of the Valsalva maneuver to maintain cerebral blood flow in high G-force turns, and the Boothby-Lovelace-Bulbulian (BLB) oxygen mask. All of these are still used by today’s fighter pilots. They received the 1939 Collier Award, the highest recognition in aviation, for their efforts. An excellent 36-minute Mayo Clinic movie about the Aero-Medical Unit and its impact on the Allies winning WWII may be viewed at Rising to the Challenge: The Mayo Aero Medical Unit in World War II (mayoclinic.org).
In 1940, Dr. Boothby recruited Dr. H. Frederic Helmholz, Jr. to join him in providing respiratory therapy and support for Mayo Clinic patients. An extensive account of Dr. Boothby’s career may be found here.
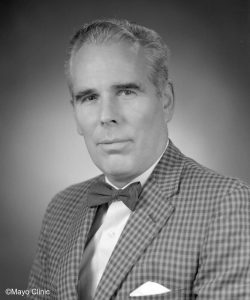
Henry Frederic (Fred) Helmholz, Jr., M.D. was born in Evanston, Illinois on December 27, 1911. In 1921, his father, Dr. Henry F. Helmholz, Sr., was recruited by Dr. Charlie Mayo to move to Rochester to establish the new clinic’s first Section on Pediatrics. The younger Dr. Helmolz was 10 years old when he rode the Northwestern Railway from Chicago to Rochester with his family. He initially attended the Rochester Public High School but spent his final two years (1927 through 1929) in Faribault, Minnesota attending its military academy, Shattuck School. Upon his graduation from Shattuck School, he attended Dartmouth College, earning his degree in 1933. This was followed by four years at Johns Hopkins Medical School and a year as a intern at the Massachusetts General Hospital.
Parenthetically, while in medical school in 1935, Dr. Helmholz married his Rochester girlfriend, Mary Balfour. Mary was a granddaughter of Dr. Will and Hattie Mayo and the daughter of Dr. Don and Carrie (Mayo) Balfour. Their bridal dinner was held on the top floor of the home of Dr. Will and Hattie Mayo. That room is now known as Balfour Hall in the Foundation House. Dr. Helmholz noted in a 2007 interview with Dr. David Plevak (see link below) that the original upper floor room was beautiful but not as ornate as the current Balfour Hall.
In 1939, he applied for a physiology fellowship at Mayo Clinic. Ironically, his MGH mentor did not know that Dr. Helmholz was the son-in-law of Dr. Balfour, the fellowship director, when he wrote his letter of recommendation. Dr. Helmholz was assigned to work with Dr. Fred Mann (yes, Mann Hall in Rochester’s Medical Science Building is named after this Mayo physiologist) at the new Institute Hills laboratory facility southwest of the city. He made and published several of the world’s first measurements of fetal circulation in animals during his initial fellowship year at Institute Hills. His work impressed Dr. Boothby, and Dr. Helmholz was invited in 1940 to join the nascent Mayo Aero-Medical Unit. In 1942, Dr. Lovelace and the U.S. Air Surgeon were so impressed with Dr. Helmholz’s knowledge of respiratory mechanics and oxygenation in flight that they asked him to move to San Diego to work with the pilots and engineers at Consolidated Aircraft Corporation. This company was producing the B-24 bombers used in World War II, and Dr. Helmholz served as a consultant as they worked to help airmen handle the challenges of high-altitude flight.
In 1947, Dr. Helmholz returned to Rochester as a consultant in the Section of Physiology. Dr. Boothby asked him to serve as the Director of Inhalation Therapy. He thought he was up to the challenge but did not know what it entailed when he started. He was blessed to find that Bernie Gilles, a nurse anesthetist working with Dr. John Lundy and a former Marine, was not only interested in inhalation therapy but someone who wished to improve and grow the field of respiratory therapy. Mr. Gilles wished for it to move beyond the delivery of oxygen to patients (inhalation therapy). Working together, they established a strong respiratory therapy program and played key roles in having inhalation therapists deliver chest physiotherapy and starting Mayo Clinic’s Pulmonary Function Lab. The lab proved the potential of analyses of exhaled gases to detect pulmonary diseases as well as metabolic disorders involving the thyroid, liver, and pancreas.
It was Bernie Gilles who proposed to Dr. Helmholz that Mayo Clinic should seek respiratory therapy certification of its locally trained inhalation therapists. With Dr. Helmholz’s coaching, Bernie became Mayo’s first certified respiratory therapist. This educational activity started Dr. Helmholz’s introduction to the newly formed American Association of Respiratory Care (AARC) and its certification process. During the 1950s and 1960s, Dr. Helmholz began to play a significant role in the development of respiratory care locally and nationally.
- Locally: He was an advocate for establishing a training program for respiratory care in conjunction with Rochester Junior College (today, the Rochester Community and Technical College). He became one of the primary instructors for the school and has been recognized with the Distinguished Emeritus Award from the Mayo Clinic School of Health Sciences for his efforts.
- Nationally: He joined the AARC’s Board of Schools and, after a major squabble between the American Society of Anesthesiologists and the AARC led to the dissolution of the Board, rekindled oversight of respiratory therapy schools across the nation by serving as the first chair of a new Joint Review Committee on Inhalation Therapy Education. Over time, he served as President of the National Board of Respiratory Care. The AARC has recognized Dr. Helmholz’s contributions with honorary membership and its Jimmy Young Medal, the highest award given by the association. The National Board of Respiratory Care has honored him with an H. Frederic Helmholz, Jr., M.D. Education Research Fund and a named scholarship.
Much more on the fascinating life and career of Dr. Helmholz can be found in a 2007 video interview organized by our own Dr. David Plevak and Mr. Jeff Ward (A Conversation with H.F. Helmholz Jr., M.D. (mayoclinic.org). Dr. Helmholz died in Rochester on January 7, 2012, at age 100.
Mystery Photos
Last week’s Mystery Photos were Lloyd H. Mousel, M.D. and David M. Rosenfeld, M.D.

Lloyd H. Mousel, M.D. was born in Cambridge, Nebraska on December 24, 1903. After receiving his M.D. degree from the University of Nebraska in 1930, he did his internship year in Tacoma, Washington and established ties there that would eventually draw him back to the Seattle area later in life. He practiced general medicine in McCook, Nebraska and in his nearby hometown of Cambridge until 1936. He moved to Rochester as a resident in anesthesiology, completing his training and earning a Master’s degree from the University of Minnesota in 1939. His Master’s degree was on the effectiveness of respiratory stimulants during anesthesia and provided him with insights that directed much of his academic career to the study of anesthesia for the nascent use of thoracic surgery.
In 1939, Dr. Mousel was appointed as a consultant in our department, joining a department of 3 other anesthesiologists, Drs. John Lundy, Ed Tuohy, and Charles Adams. Dr. T. Harry Seldon subsequently joined the department in 1940. Although a member of the department until 1946, Dr. Mousel was called to military duty in 1942 and served most of his remaining four years as a Mayo consultant in U.S. Army assignments. Much of his duty was focused in Washington, D.C. running Gallinger Municipal Hospital, a primary hospital in the nation’s capital used for the care of injured soldiers, Marines, airmen, and sailors. He also was assigned as the Army’s leader of anesthesia for thoracic surgery during his service. In this role, he standardized data collection about the care of thoracic surgery patients who received their care in the Army’s 7 designated “thoracic surgery” hospitals. Based on the findings of the accumulated work, he wrote extensively about anesthesia for thoracic surgery, with his insights guiding clinical practices across the country for the article next several decades. His 1947 provides a fascinating look at the development of anesthesia for thoracic surgery and its status, clinical practices, and morbidities during World War II.
In 1946 and upon his military discharge, Dr. Mousel resigned from Mayo Clinic and accepted the position as chief of anesthesia services at the George Washington University, a role he held from 1946 through 1951. He subsequently moved to Seattle and became the chief of anesthesia services at the rapidly growing Swedish Hospital. He worked closely with the University of Washington and his hospital’s anesthesia services became an integral part of the anesthesia training program at the university.
Dr. Mousel died on June 13, 1970.

David M. Rosenfeld, MD was born May 9, 1969, at Michael Reese Hospital in Chicago, IL. He grew up in Glencoe, IL, a small town twenty miles north of Chicago. His undergraduate education was at the University of Colorado, Boulder, where he earned a degree in Political Science in 1991, considering a career in law and the foreign service. In 1992 he acted on his long-repressed desire to be a physician and enrolled in a one-year post baccalaureate pre-medical program at Loyola University in Chicago. He graduated from Northwestern University Medical School in 1998, where he participated in research focusing on the immunology and cellular rejection pathways of Islet of Langerhans transplantation. Dr Rosenfeld served his internship in general surgery at University of Wisconsin Hospital in Madison, followed by his anesthesiology residency at UCLA Medical Center. He completed his residency training in 2002. While a medical student at Northwestern he met his future wife Missi, at the time a visiting medical student from University of Arizona, and the couple was fortunate to train in anesthesiology together at UCLA. His residency was followed by a Pain Medicine fellowship at Brigham and Women’s Hospital in Boston.
Dave joined the department at Mayo Clinic Arizona in 2003. In his first years of practice, he combined clinical work between general, regional, and cardiac anesthesia, while devoting twenty-five percent time to clinic and in-patient pain medicine. The first decade of the 21st century saw tremendous advances in pain medicine, but also an explosion in the use of prescription opioids prescribed to treat mostly benign pain conditions leading to what is now referred to as the opioid epidemic. Well intentioned improvements in pain management for hospitalized patients led to an increase in adverse events mainly due to opioid-induced respiratory depression. In 2007 Dr. Rosenfeld and partner Julia Griffin, RN, CNS, established the first MCA Pain Management Committee, with a focus on quality improvement and safety. Many initiatives were advanced across MCA to improve education, standardization of opioid use protocols, and improved monitoring for patients. At the enterprise level he worked with one of our Rochester colleagues, Dr. Terre Horlocker, on the “Surgery + Opioid = Narcan” project in 2007. The project helped define these issues and spearheaded collaborative improvements. Dave served as division chair in Pain Medicine from 2008 through 2014, overseeing steady growth, the relocation of the clinic to the Phoenix 3 Building, and comprehensive reorganization of operations. In 2014 he partnered with administrator Roshy Didehban to recruit Cynthia Townsend, PhD and establish the Pain Rehabilitation Center, the first of its kind in the region.
In 2005, Dave’s clinical anesthesia responsibilities migrated from cardiac to liver transplantation. During the past nineteen years, he has been involved in more than 400 transplants. He is a national leader in abdominal transplant anesthesia and serves on committees in the ASA and the Society for the Advancement of Transplant Anesthesia. He has devoted his career to advancing the specialty of anesthesiology in education, research, mentoring, and patient safety. In 2022 Dr Rosenfeld was appointed as chair of our Department of Anesthesiology and Perioperative Medicine in Arizona. He has also served as the department Vice Chair, medical director of Surgical Services and section chair of Abdominal Transplant Anesthesiology before becoming department chair.
Dave has been married to Dr. Missi Rosenfeld for 26 years. Missi works for Valley Anesthesiology Consultants/Envision Healthcare and recently joined Mayo Clinic as a supplemental consultant. They have two children, Ethan and Eliana. In his spare time, Dave plays ice hockey, skis, and is an avid hiker who loves the outdoors. He is an accomplished musician/guitarist and has played in a number of different rock bands since high school.
Mystery Photo Contest Winner

Last week’s contest winner was Alyssa Janousek.
Here are this week’s Mystery Photos. Reminder: We are now featuring two individuals each week for the Updates. To be placed into the Mystery Photo Starbucks contest, you will need to correctly guess at least one of the featured individuals. If you identify both of them, you will double your chances of having your name drawn.
Please email your response at warner.mark@mayo.edu within 3 days of this update. I will also need your name and contact information. All correct responses will be placed into a Monday morning drawing for a $10 Starbucks card. Only one winner per individual over the 80 weeks of Mystery Photos. If you win a weekly drawing, however, please keep submitting your responses. An overall winner (with the most correct responses in the series of 80 Updates) will receive a $100 Starbucks card.

The Department of Anesthesiology: Richard Lundborg, M.D. and Advocacy

Richard O. (Dick) Lundborg, M.D. is a native Minnesotan who was on our Rochester staff from 1965 through 1972. He left Mayo Clinic to coordinate and improve anesthesia services on the Big Island of Hawaii from 1972 through 1982. By 1982, the Hawaii Medical Association enlisted him to assist with tort reform in the state as malpractice cases were growing exponentially. This was a period before the start of the anesthesia patient safety movement in1985. Physicians were being priced out of the malpractice insurance market and there was risk of loss of anesthesia services across the state. He served as a legislative consultant in tort reform and other medical insurance issues. His efforts, along with the dramatic improvements in patient safety during the late 1980s that accompanied the introduction of intraoperative monitoring standards and advocacy by the newly formed Anesthesia Patient Safety Foundation, resulted in a marked lowering of malpractice insurance premiums, a reduction in the number of malpractice claims against anesthesia providers in the state, and a stabilization of anesthesia services on the islands.
Dick tells a very interesting story about his time in Rochester as a resident and staff member, as well as his Hawaiian experiences, in an article from our department’s newsletter in 2007. Please note his comments about working with a young resident, Dr. Rungson Sittipong, in obstetrics. More on Rungson follows below.
Mystery Photos
Last week’s Mystery Photos were Rungson Sittipong, M.D. and John W. Pender, M.D.

Rungson Sittipong, M.D. was born in Chiang-Mail, Thailand on July 16, 1941. His family moved to Bangkok while he was still in primary school. Rungson graduated from the Chulalongkorn University School of Medicine in 1965, receiving his M.D. degree as his class valedictorian. He was handed his degree directly from the King of Thailand. After a one-year internship at Chulalongkorn Hospital, he made an unlikely move in 1966 from Bangkok to Duluth, Minnesota where he was an intern at St. Luke’s Hospital. He impressed Mayo alumni while working at St. Luke’s and was encouraged to move to Rochester. From 1967 through 1968, Rungson was a resident in physiology, working closely with two of the world’s most eminent authorities on pulmonary physiology, our own Drs. Kai Rehder and Bob Hyatt. He then was an anesthesiology resident here from 1968 through 1972.
Rungson was brilliant and served as a remarkable resource of knowledge related to respiratory physiology. As such, he was recruited in 1972 to join Dr. Alan Sessler in his growing Section of Respiratory Care. That same year, Dr. H. Michael Marsh, who had previously been a clinical fellow in intensive care in Rochester, returned from Australia and joined the section. Together, to quote Dr. Peter Southorn’s summary in our department’s Art to Science history book, “(Marsh and Sittipong) were the advance guard of what came to be called . . . ‘Sessler’s foreign legion in intensive care’.” In 1976, Rungson left the Section on Respiratory Care and moved to full-time practice in the Rochester Methodist Hospital operating rooms. He joined forces with Drs. Duane Rorie, David Byer, Dave Nelson, and others in a growing regional anesthesia practice. He remained in this position until his initial retirement in 1996. He returned temporarily to Thailand to care for his elderly family members. During his time in Thailand, he volunteered at the medical schools and anesthesiology training programs in Bangkok. In 2001, he returned to Rochester and rejoined the department as a supplemental consultant. He continued in that role, with a special focus on working in the Preoperative Evaluation Clinic, through 2017.
There are so many wonderful stories about Rungson. Dr. Scott Atchison (Sioux Fall, South Dakota) wrote a short synopsis of “Rungson-isms” in our department newsletter of September 2002. In brief, he was beloved by everyone, including colleagues and patients. Most anyone who ever connected with him has one or more Sittipong stories, most of which have an element of truth in them (ha!). These range from his love of students of all types (he was Teacher of the Year for the residency in 1974 and 1986) to his joy for caring for patients and being with trainees and colleagues and to his enchantment with gambling, a trait he gained from his grandmother. A few of my favorite stories include his prize guppy, Fishong; his incredibly strong Manhattan drinks that he’d prepare for residents and friends during poker games in his Rochester Tower apartment; his mischievousness during the workday that brought smiles to everyone during especially busy late afternoons; and his way of simplifying the most difficult physiologic issues for trainees to understand. Regarding those Manhattan drinks, it is surprising how many of the plants in his living room suffered when Rungson would prepare “just one more drink” for his poker-playing guests. They would often pour those last drinks onto his plants when he wasn’t looking. No one ever wished to offend Rungson, but they also knew they could not possibly drink those last Manhattans before leaving for the evening.
If you have other Sittipong stories that you would like to share and allow us to archive, please send them to me at warner.mark@mayo.edu.
Rungson traveled extensively, loved the opera, and knew almost every Thai chef in New York City by first name. He had friends in most of the world’s major cities and would always let them know if you were going for visits to those cities. He had an extensive collection of stamps and coins, as well as an encyclopedic knowledge about philately and numismatics. He was one of the most generous individuals you would ever meet, sharing both his expertise and his collections.
He lived at Charter House in Rochester for most of his time after returning in 2001 from Bangkok. Rungson passed away August 21, 2020.

John W. (Bill) Pender, M.D. was born on September 3, 1912, in Hesterville, Mississippi. After earning an M.D. at Tulane University in 1935, an internship in New Orleans, and time in a general practice, Dr. Pender moved to Rochester in 1940 to begin fellowship training in our department. He was called to the U.S. Navy in 1942 and served admirably during World War II, inventing the “Pender Lemon”to assist with administration of ether to injured Marines, sailors, and airmen who required endotracheal intubation for their care. The device allowed careful titration of open drop diethyl ether, reducing spillage, waste, and the risk of aerosolization in the surgical environment and potential fire hazard. Subsequently, it was used in routine clinical practice, especially in cases in which patient positioning did not easily facilitate direct methods of using open drop ether (e.g., unique neurosurgical positions). This device continued to be used in our department until 1978, most often by Dr. Paul Leonard and Lucille Chen, CRNA.
Upon completion of the war, Dr. Pender returned to Mayo Clinic where he remained on the staff until 1954. During this time in Rochester, he published a number of papers. One of his most influential articles reported on the early use of endotracheal intubation in children. His observations (e.g., that the endotracheal tube should fit firmly but not tightly as it passes the vocal cords and through the cricoid ring) were put into practice for many years and continue to represent good practice. Dr. Pender moved from Rochester in 1954 and became chair of the Department of Anesthesiology at the Palo Alto Medical Clinic in California. He continued to be very involved in academics in this private practice setting, attaining a professor rank from Stanford University in 1977 and serving as an associate editor of Anesthesiology from 1956 through 1965. He was elected as a director of the Wood Library Museum of Anesthesiology in 1969, a position he held until 1978. He also was chair of the Section on Anesthesia of the AMA in 1970 and 1971. He became President of the Academy of Anesthesiology in 1965 and was recognized with its Citation of Merit Award in 1983.
Dr. Pender and his wife, Catherine, had six children. He died in 2001. Upon his death, he bequeathed a “Mayo Room” at the Wood Library Museum. You may read about the room and Dr. Pender’s many contributions in this story by Dr. Mary Ellen Warner that appeared in our department’s newsletter in January 2005. Dr. Pender also provided a leadership gift to establish the John W. Pender, M.D. Collection of the Living History of Anesthesiology at the museum (Living History Interviews - Wood Library-Museum of Anesthesiology (woodlibrarymuseum.org). This collection contains nearly 150 oral histories of leaders in anesthesiology and continues to grow in number annually.
Mystery Photo Contest Winner

Last week’s contest winner was Steve Endres.
Here are this week’s Mystery Photos. Reminder: We are now featuring two individuals each week for the Updates. To be placed into the Mystery Photo Starbucks contest, you will need to correctly guess at least one of the featured individuals. If you identify both of them, you will double your chances of having your name drawn.
Please email your response at warner.mark@mayo.edu within 3 days of this update. I will also need your name and contact information. All correct responses will be placed into a Monday morning drawing for a $10 Starbucks card. Only one winner per individual over the 80 weeks of Mystery Photos. If you win a weekly drawing, however, please keep submitting your responses. An overall winner (with the most correct responses in the series of 80 Updates) will receive a $100 Starbucks card.

The Start of the Section on Respiratory Intensive Care and Its Evolution into the Critical Care Service
In Centennial Update #52 (September 5, 2024), I wrote about Drs. Walter Boothby and Fred Helmholz and their contributions to starting oxygen therapy and rudimentary respiratory care at Mayo Clinic in the 1940s and 50s. By the late 1950s and early 60s, several U.S. institutions were developing respiratory care units that could support patients who were receiving positive-pressure ventilation with early models of ventilators.
During the first several years of the 1960s, Drs. Helmholz at St. Marys Hospital and E. Paul Didier at the Methodist Hospital were on call nearly at all times to assist with patients who needed respiratory support. In 1964, our department chair, Dr. Albert Faulconer, addressed this growing, untenable situation by forming an ad hoc committee to develop a plan to provide better care to patients with respiratory failure. They advised establishing a respiratory intensive care unit led by anesthesiologists and staffed 24 hours a day. Neither of these recommendations was universally appreciated by our Mayo surgical and medical colleagues at the time. However, Dr. Faulconer prevailed, received permission from the Board of Governors to proceed, and appointed Dr. Didier at Methodist Hospital and Dr. Alan Sessler at St. Marys Hospital to establish these new intensive care units. Each was assigned a nurse anesthetist as a partner. Dr. Didier worked with Renee Casperson, CRNA and Dr. Sessler worked with Bernie Gilles, CRNA. Respiratory intensive care at Mayo Clinic was started!
From left to right: Dr. Alan Sessler; Dr. E. Paul Didier; Bernie Gilles, CRNA; and Renee Casperson, CRNA
Dr. Peter Southorn worked in the intensive care units starting in 1976 and served as a valuable member of our Critical Care Service for more than two decades. By the late 1990s, he had known all of the members of the service, interviewed many of the early participants, reviewed many sets of minutes, and did an outstanding job of documenting the start of respiratory intensive care in the institution. His remarkably detailed story of this start of the critical care service is found in the department’s Art to Science book published in 2000. Our archivist, Alec Thicke, has digitized the story.
For brevity, I will not repeat Dr. Southorn’s story but will highlight a timeline from 1966’s start of the Rochester intensive care units through 1981’s formation of a joint Critical Care Service.
- 1966: Drs. Didier and Sessler, along with nurse anesthetists Renee Casperson and Bernie Gilles, establish respiratory care units at Methodist and St. Marys Hospitals, respectively.
- 1966: Dr. Didier and Mr. Earl Schwerman, head of Methodist Hospital’s pharmacy, start our “Code 45” system for emergency resuscitation services in both hospitals.
- 1967: Blood gas analyzers are placed into space near each new intensive care unit using technology and knowledge from the laboratories of Drs. Emerson Moffit, Kai Rehder, Dick Theye, and Ward Fowler.
- 1968: Dr. Rehder joins the intensive care team and begins a life-long distinguished research program into the pathophysiology of impaired gas exchange in anesthetized as well as mechanically ventilated patients.
- 1969: Myron Ricks, CRNA, establishes the institution’s airway management and cardiopulmonary resuscitation courses.
- 1969: Drs. Helmholz and Rehder establish the first pulmonary function lab at St. Marys Hospital.
- 1971: Dr. Theye, new chair of the department, receives permission from the Board of Governors to establish a Section on Respiratory Care. Anesthesiologists involved include Drs. Sessler, Didier, Rungson Sittipong, and Sheila Muldoon.
- 1972: Internists in pulmonary medicine (i.e., Drs. Bill Douglas and Matt Divertie) and, subsequently, in nephrology (Dr. Dan Wochos), work part-time in the Section on Respiratory Care.
- 1973: The first class of respiratory therapists graduate.
- 1974: Pulmonary artery catheters are introduced into the clinical practice in the Mayo intensive care units, bronchial lavage therapy for alveolar proteinosis is first used, and NIH funds are obtained to study acute respiratory distress syndrome (ARDS).
- 1976: Anesthesiologists covering the intensive care units are dedicated to this practice and not asked to cover operating rooms at the same time.
- 1976: Dr. John McMichan becomes the first critical care fellow and advocates for the use of cardiac output determinations and advanced hemodynamic monitoring
- 1980: Jeff Ward, RT, is appointed to lead the respiratory therapy training program.
- 1981: The Board of Governors approves the establishment of a multidisciplinary Critical Care Service. Dr. Didier is appointed chair of the department’s new Section on Critical Care.
From left to right: Dr. Kai Rehder; Myron Ricks, CRNA; Dr. Rungson Sittipong; Dr. Sheila Muldoon; Dr. John McMichan; Dr. Edward Daw; Dr. Edward B. Tuohy; Dr. Steven H. Rose; and Jeff Ward, R.T.
Mystery Photos
Last week’s Mystery Photos were John S. Hattox, M.D. and R. Charles Adams, M.D.
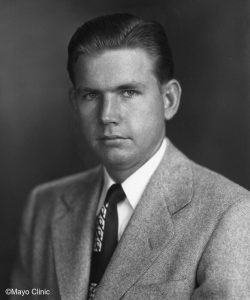
John S. Hattox, M.D. was born in Coldwater, Mississippi in 1921. After receiving his undergraduate degree from Mississippi College in Jackson, Mississippi, he earned his M.D. at the University of Tennessee in 1945. At that time, the University of Mississippi did not yet have a medical school. After several years in the U.S. Navy, he moved to Rochester and joined our department as a resident in anesthesiology. He completed his training in 1951. Classmates included Drs. David Massa, inventor of the intravenous catheter, and Robert Devloo, long-time cardiac anesthesiologist in our department. During his time at Mayo Clinic, Dr. Hattox earned a Master’s degree in anesthesiology. His thesis was entitled, “A New Method for the Analysis of Blood Nitrous Oxide and Its Application to a Study of Anesthesia with this Agent.”
Dr. Hattox moved to San Diego in 1951 and joined the fledgling Anesthesia Service Medical Group. During his time in that group, it grew to be the largest private practice anesthesia group in the country for a period of time. Dr. Bob Adams, noted below in the story about his dad, Dr. Charlie Adams, served as president of the group from 1983 through 1988. Dr. Hattox remained in clinical practice with that group until retiring in 1990.
As described in Dr. James Arens’ memorial article for Dr. Hattox in 2018, Dr. Hattox was influenced by his former Mayo Clinic instructors as well as past ASA presidents, Drs. Rick Siker and Harry Bird, to participate in the California Society of Anesthesiologists and the ASA. Both Drs. Siker and Bird were great friends of our own Dr. Alan Sessler. Dr. Sessler, one of the specialty’s finest and most successful mentors, also supported Dr. Hattox’s involvement in ASA. Dr. Hattox served as president of the California Society of Anesthesiologists in 1966. He rose to president of the ASA in 1980, with his term as president matching the first years in the specialty as residents for Drs. Steve Rettke, Bob Chantigian, Mary Ellen Warner, and me. He was the first ASA president that I heard present his summary of the year at an ASA House of Delegates’ meeting. Dr. Hattox also served as chair of the ASA’s AMA Section Council in Anesthesiology. He was an ABA examiner. He was recognized for his contributions to the specialty in 1982 when he received the Distinguished Service Award from the California Society of Anesthesiologists and, in 1992, received the Distinguished Service Award from the ASA. He is one of only 8 Mayo Clinic anesthesiology alumni to receive the ASA Distinguished Service Award (Mayo Clinic | Anesthesiology | Department Awards Statistics).
Dr. Hattox was married to Kathy Crippen Hattox. Kathy was an amazing spouse, an outstanding lawyer in the San Diego area, and one of the city’s most generous philanthropists. Hattox Hall in The Old Globe Theater in Balboa Park is named from Kathy and John. You may learn more about Kathy at Old Globe Mourning Death of Board Member Kathryn Crippen Hattox - Times of San Diego. Dr. Hattox passed away on December 31, 2017. He was a modest soul. Dr. Bob Adams recalled a time when someone complimented Dr. Hattox on his many successes and contributions to anesthesiology. His response was typical: “Well, I don’t know about that. I do know that if I died tomorrow, all anyone would be asking would be who’s going to take my call that weekend.”

Charles Adams, M.D. was born in Woolner, Ontario, Canada on August 7, 1906. He earned his M.D. at Queen’s University in Kingston, Ontario in 1931. After 4 years of general practice in Ontario, he moved to Rochester as a resident in anesthesiology. His classmates were Ralph T. Knight, M.D. (highlighted in Centennial Update #48; August 8, 2024) and John H. Hutton, M.D. He completed his training and earned a Master’s degree in anesthesiology from the University of Minnesota in 1937. His thesis for his degree was “Intravenous Anesthesia: Chemical, Pharmacologic and Clinical Considerations of the Anesthetic Agents Including the Barbiturates.”
Dr. Adams’ work with intravenous anesthesia in 1936 and 1937 aligned him closely with Dr. John Lundy. Dr. Lundy had first used sodium pentothal in June 1934, yet little was known about the barbiturate, its metabolism, and its physiologic impact in various disease states and trauma. Together, they gathered data and wrote extensively about their clinical experiences and laboratory evaluations of pentothal. Their advocacy for intravenous anesthesia led to a remarkable shift in the care of surgical patients in the coming decades. When reports from Pearl Harbor suggested that pentothal was a dangerous drug to use in traumatized military personnel who were in shock, it generated an extended controversy. In 1944, Dr. Adams wrote an article in the Journal of the American Medical Association describing the use of pentothal in peace and war. That article was cited worldwide over the following decade and was a major contributor to the advancing popularity and safe use of intravenous anesthesia. As a protégé of Dr. Lundy and, therefore, knowledgeable about Lundy’s advocacy for balanced anesthesia, he also noted in that and other articles the efficacy and safety of using intravenous anesthesia as an adjunct for regional anesthetic techniques and in combination with nitrous oxide or other inhaled anesthetics.
Drs. Adams and Lundy worked together for two decades and advocated for improvements in anesthesia care that have advanced the specialty. For example, they suggested that a hemoglobin of less than 10 mg/dl should be considered as a trigger point for transfusion in the perioperative period. In the decades before ubiquitous hemodynamic and oxygenation monitoring during the perioperative period, this trigger proved valuable in improving patient safety and was used around the globe. In 1944, Dr. Adams wrote an exhaustive text (663 pages) of the chemistry, pharmacology, physiologic actions, and his reflections and observations on the use of barbiturates and other intravenous anesthetics. Following Dr. Lundy’s footsteps in organized medicine, he served in both the ASA House of Delegates and as a member of its Board of Directors.
In 1952, Dr. John Lundy was asked to step down as chair of the Section on Anesthesiology and Intravenous Therapy. His 28-year leadership of the department was remarkable and advanced the specialty in so many ways. However, after nearly 3 decades as chair, the institution’s leaders sought someone with a different leadership style . . . perhaps less confrontational. It appears that Dr. Lundy wanted Dr. John Pender as his successor, but the Mayo Board of Governors chose the gentlemanly, affable Dr. Adams instead. Unfortunately, medical issues led him to step down just a year later in 1953. He was succeeded by Dr. Albert Faulconer.
Dr. Adams and his wife, Elma Maude, had two children. He and his wife were highly respected citizens of Rochester and strongly supported music and theater in the city. Dr. Adams passed away on January 21, 1956. An excellent summary of his life can be read on page 3 of Volume 7, No. 7 of the 1956 MayoVox edition.
Post-Script for the Dr. Adams story -- The Creation of the Anesthesia Foundation: According to Dr. Doug Bacon’s 75th Anniversary book on the Academy of Anesthesiology, Dr. Adams was the first of 6 amazing leaders in the specialty and members of the Academy to pass away in 1956. The other five include luminary leaders Drs. Arthur Guedel, Henry Ruth, Robert Hammond, Brian Sword, and Roland Whitacre. My guess is that you will recognize at least several of these names, no matter your length of time in working in anesthesia. In their memories, the Academy established the Anesthesia Foundation (The Anesthesia Foundation® – Helping Anesthesiologists Succeed). The foundation continues to this day with a goal:
- To support young physicians in their choice of anesthesiology as a specialty
- Support specific projects that enhance the specialty of anesthesiology and are not supported by other agencies
- Recognize and preserve the American heritage of anesthesiology
A Second Post-Script for the Dr. Adams’ Story -- his son, Dr. Robert Adams: Dr. Adams’ son, Bob, also trained in anesthesiology and worked in our department. He completed his training in 1971 with Dr. Michael Marsh as one of his classmates. Bob served 2 years of active duty in the U.S. Naval Hospital in San Diego, California and returned to Rochester to join our staff in 1973. However, within a year he headed back to San Diego and joined the Anesthesia Service Medical Group. This group during Bob’s leadership of it from 1983 through 1988 became the largest private practice group of anesthesiologists in the country. Ironically, one of the founders of the group was Dr. John Hattox (see above).

Mystery Photo Contest Winner
For the first time in 53 weeks, there is no winner for last week’s Mystery Photo contest. Four individuals correctly named one or more of the two Mystery Photos (Drs. Charlie Adams and John Hattox) but each has been a previous winner of the contest. Their correct answers will be added to their cumulative total of correct answers but they are not eligible to win more than one weekly contest. All four have a large number of overall correct answers and are in the running for the final “top prize” of a $100 Starbucks card at the end of the 80 Centennial Updates. I promise that this week’s contest will have many correct responses.
I note that more than 350 alumni and current staff members have one or more correct responses to the Mystery Photos in the first 53 weeks. These responses come from 12 countries and 38 states. I am very grateful for the wide readership of the Centennial Updates and hope that you enjoy learning about the history of the department and our remarkable past and current colleagues and their achievements.
Here are this week’s Mystery Photos. Reminder: We are now featuring two individuals each week for the Updates. To be placed into the Mystery Photo Starbucks contest, you will need to correctly guess at least one of the featured individuals. If you identify both of them, you will double your chances of having your name drawn.
Please email your response at warner.mark@mayo.edu within 3 days of this update. I will also need your name and contact information. All correct responses will be placed into a Monday morning drawing for a $10 Starbucks card. Only one winner per individual over the 80 weeks of Mystery Photos. If you win a weekly drawing, however, please keep submitting your responses. An overall winner (with the most correct responses in the series of 80 Updates) will receive a $100 Starbucks card.

Photograph of Mayo Clinic Alix School of Medicine entrance.
The Department of Anesthesiology: Training Beyond the Norm, Providing Unique Opportunities for the Department to Expand Its Sphere of Influence
From the start, our department has been blessed with outstanding anesthesiologists who had a thirst for learning. Many of our department’s anesthesiologists and trainees from 1924 through the 1960s obtained Master’s degrees from the University of Minnesota and expanded their expertise and contributions to the growing specialty.
By the 1970s, our physicians began seeking training in core specialties such as Internal Medicine before entering anesthesiology. Many of these (e.g., Drs. Mike Murray, Brad Narr, Dave Plevak, and others) worked in our intensive care units. They were “triple board certified” in Internal Medicine, Anesthesiology, and Critical Care Medicine. Additional anesthesiologists in the 1980s trained in more than one subspecialty fellowship. Examples include Drs. Gary Vasdev (Obstetric Anesthesia and Critical Care), Gerard Kamath (Critical Care and Cardiac Anesthesia), and Bob Chantigian (Pediatric and Obstetric Anesthesia). Starting in 2000, others (e.g., Drs. Chris Burkle and Matt Kumar) obtained legal degrees. Quite a few of our colleagues have earned Ph.D. degrees either before, during, or after anesthesiology residency training.
The concept of having multiple board certifications in clinical specialties expanded in the 1990s and early 2000s when people such as Randall (Randy) P. Flick, M.D. and W. Michael (Mike) Hooten, M.D. became our earliest “quad board certified” colleagues. Randy came to Mayo Clinic after completing training in Pediatrics, Pediatric Critical Care Medicine, Anesthesiology, and Pediatric Anesthesiology (see story about Randy below). Mike joined us after completing training in Psychiatry, Internal Medicine, Anesthesiology, and Pain Medicine. Their broad bases of knowledge and experiences made them uniquely valuable as we integrated pediatric and pain medicine services across the institution.
Since Randy and Mike have joined the staff, we now have multiple colleagues who are board certified in four specialties. One of these, Dr. Francis (Fran) Whalen, Jr. currently is board certified in five specialties after recently adding certification in Hospice Medicine to certification in Internal Medicine, Pulmonary Medicine, Critical Care Medicine, and Anesthesiology. Having colleagues with their breadths of expertise plays an important role in our department’s ability to provide outstanding care across and beyond the continuum of perioperative care. This expansion of expertise is crucial as we seek to increase the value of our department to our Mayo Clinic patients, the institution, and the specialty overall.
One example of expanding our value to patients is pediatric anesthesiology in Rochester. There are approximately 70 anesthesiologists in the U.S. who currently are board certified in Pediatrics, Pediatric Critical Care Medicine, Anesthesiology, and Pediatric Anesthesiology. Seven of those remarkable individuals are in our department. They are both pediatricians and anesthesiologists. They include: Devon O. Aganga, M.D.; Matthew G. Di Giusto, M.D.; Randall P. Flick, M.D.; Steven J. Gleich, M.D.; Michael E. Nemergut, M.D., Ph.D.; Gregory J. Schears, M.D.; and Ashley V. Wong Grossman, M.D.
The Rochester-based Division of Pediatric Anesthesia has 7 other anesthesiologists who are not pediatricians but who have trained in additional fellowships that augment their training in Pediatric Anesthesia. These include Kathryn S. Handlogten, M.D. (Regional Anesthesia); Tracy E. Harrison, M.D. (Pain Medicine); Lindsay R. Hunter Guevara, M.D. (Neuroanesthesia); Elena A. Swan, M.D., Ph.D. (Pediatric Cardiac Anesthesia); Elizabeth R. Vogel, M.D. Ph.D. (Pediatric Cardiac Anesthesia); Lindsay L. Warner, M.D. (Obstetric Anesthesia); and Robert T. Wilder, M.D., Ph.D. (Pain Medicine).
Our division membership of very highly trained pediatric anesthesiologists is augmented by pediatrician intensivist colleagues (non-anesthesiologists) who share coverage of our Pediatric Intensive Care Units and who have additional training and certification in Cardiology (two) and Infectious Disease (one).
This example of integration of broadly trained anesthesiologists in pediatrics demonstrates how our department is meeting the vision of William J. Mayo, M.D. At the commencement address to graduates of Rush Medical College, University of Chicago on June 15, 1910, he said, "The best interest of the patient is the only interest to be considered, and in order that the sick may have the benefit of advancing knowledge, a union of forces is necessary." Indeed, our department has the ability to bring together that “union of forces” to provide outstanding care to patients undergoing surgical and diagnostic procedures, those who are critically ill, and those who experience acute and chronic pain. We should be proud of all that we have accomplished in our first 100 years as a department and look to an even brighter future.
Mystery Photos
Last week’s Mystery Photos were Randall P. Flick, M.D. and Marie L. De Ruyter, M.D.

Randall (Randy) P. Flick, M.D. was born in Fargo, North Dakota on June 24, 1957. He received an R.N. diploma from St. Luke’s Hospital School of Nursing in 1980 and a B.A. degree from Moorhead State University in 1983. He earned an M.D. degree from the University of North Dakota School of Medicine in 1987. Randy completed an internship and residency in pediatrics at St. Louis Children’s Hospital, Washington University in 1990; a residency in anesthesiology at Barnes Hospital-Washington U. in 1992; and a fellowship in advanced specialty training in pediatric anesthesiology and intensive care at The Johns Hopkins Hospital in 1995. He joined the staff of Mayo Clinic that same year. He holds board certification in four specialities: Pediatrics and Pediatric Critical Care, as well as Anesthesiology and Pediatric Anesthesiology.
Randy made an immediate impact on the quality of our care of children upon his arrival to Rochester. He was an outstanding clinician and educator in our operating rooms and our pediatric intensive care units. He received multiple Excellence in Teaching Awards from the Mayo Medical School in his first decade on staff. He was appointed chair of the Division of Pediatric Anesthesia in 2006 and continued in that role through 2013. In his years at Mayo Clinic, Randy has played a major role in recruiting and developing high quality and well-trained pediatric anesthesiologists (see above story). In 2009, he was asked to serve as the medical director of the Mayo Clinic’s Eugenio Litta Children’s Hospital. In 2014, he advanced to medical director of the entire Mayo Clinic’s Children’s Center. In that role, he oversaw all pediatric activity across the institution. He completed his time as our Mayo pediatric services leader in 2023.
Randy is a past president of the Society for Pediatric Anesthesia (SPA; 2016-2018). He previously chaired the ASA Committee on Pediatric Anesthesiology. He has served as chair of the U.S. FDA’s Advisory Committee on Anesthetics and Analgesic Drug Products and has been a member of the Pediatric Advisory Committee reporting directly to the FDA commissioner. Dr. Flick currently serves as a member of the National Institute on Child Health and Human Development’s (NICHD’s) Pediatrics Study section.
Randy’s research interests have included outcomes in pediatric anesthesia, neurodevelopment effect of anesthetic exposure, and quality in pediatric hospital care. Working with colleagues such as Drs. David Warner, Bob Wilder, Juraj Sprung, Toby Weingarten, Yu Shi, Steve Gleich, Mike Nemergut, Lindsay Hunter Guevara, and Devon Aganga, he has played a major role in elucidating and understanding the impact of repeated general anesthetics on the brains of infants and children. He currently is a co-PI on a federally funded study of the effects of anesthetic exposure on the developing brain and co-investigator on another NIH grant, “Neuroimaging Studies in Pediatric Anesthesia Neurotoxicity. “
Dr. Flick and his wife, Loree, have three sons. In the community, he has served as president of the local Ronald McDonald House Board, is a global medical advisor to Americares International, a current trustee of the Minnesota Zoo, and a board member of the SPA’s Women’s Empowerment and Leadership Initiative. Loree is also very involved in the children’s services in the community (e.g., SPARK, Rochester’s Children’s Museum).

Marie L. De Ruyter, M.D. was born in Riverside, California on January 5, 1962. She received her undergraduate degree from Santa Clara University in 1984, a Master’s degree in Biological Sciences from California Polytechnic State University, Pomona in 1986, and her M.D. from Creighton University, Omaha, Nebraska in 1990. Marie completed her internship and anesthesiology residency in Rochester in 1994. She graciously joined our staff at Mayo Clinic Florida that same year. Coincidently, her older brother, Marty, completed his anesthesiology training and a critical care fellowship here in Rochester, also in 1994, and joined our Rochester department.
Marie is an outstanding educator and her career interest has always been focused on resident education. She was voted “Teacher of the year” in 1996, 1997, and 2013. She was the Jacksonville program director of our institutionally integrated anesthesiology residency program from 1997 through 2001. In 2000 and early during the chairmanship of Dr. Mike Murray, Marie embarked on applying for an independent residency program at Mayo Clinic Florida. The ACGME awarded provisional accreditation for the residency program in 2002, and the first residents started in July 2003. Marie was the program director until 2013. Marie served as chair of the residency program’s Clinical Competency Committee from 2016 through 2021. Among her many career interests, she pursued adding simulation education into our Florida training programs. She developed and coordinated the residency simulation curriculum from 2010 – 2023. Outside of Mayo Clinic, Marie has been a long-time member of the Faculty Development and the Research Committees of the Society for Education in Anesthesia.
Her clinical practice interests are in neuroanesthesia where she has worked to improve the practice on various quality improvement projects. From 2006 through 2008, Marie chaired the department’s Division of General Anesthesia.
Marie and her husband, Dr. Mark Parkulo, an internist at Mayo Clinic Florida, have 3 children. They live in Ponte Vedra Beach, FL and enjoy Jacksonville Jaguar football (sometimes – ha!) and travelling.
Mystery Photo Contest Winner
Last week’s winner of the Mystery Photo contest was Maria De Castro.

Here are this week’s Mystery Photos. Reminder: We feature two individuals each week for the Updates. To be placed into the Mystery Photo Starbucks contest, you will need to correctly guess at least one of the featured individuals. If you identify both of them, you will double your chances of having your name drawn.
Please email your response at warner.mark@mayo.edu within 3 days of this update. I will also need your name and contact information. All correct responses will be placed into a Monday morning drawing for a $10 Starbucks card. Only one winner per individual over the 80 weeks of Mystery Photos. If you win a weekly drawing, however, please keep submitting your responses. An overall winner (with the most correct responses in the series of 80 Updates) will receive a $100 Starbucks card.
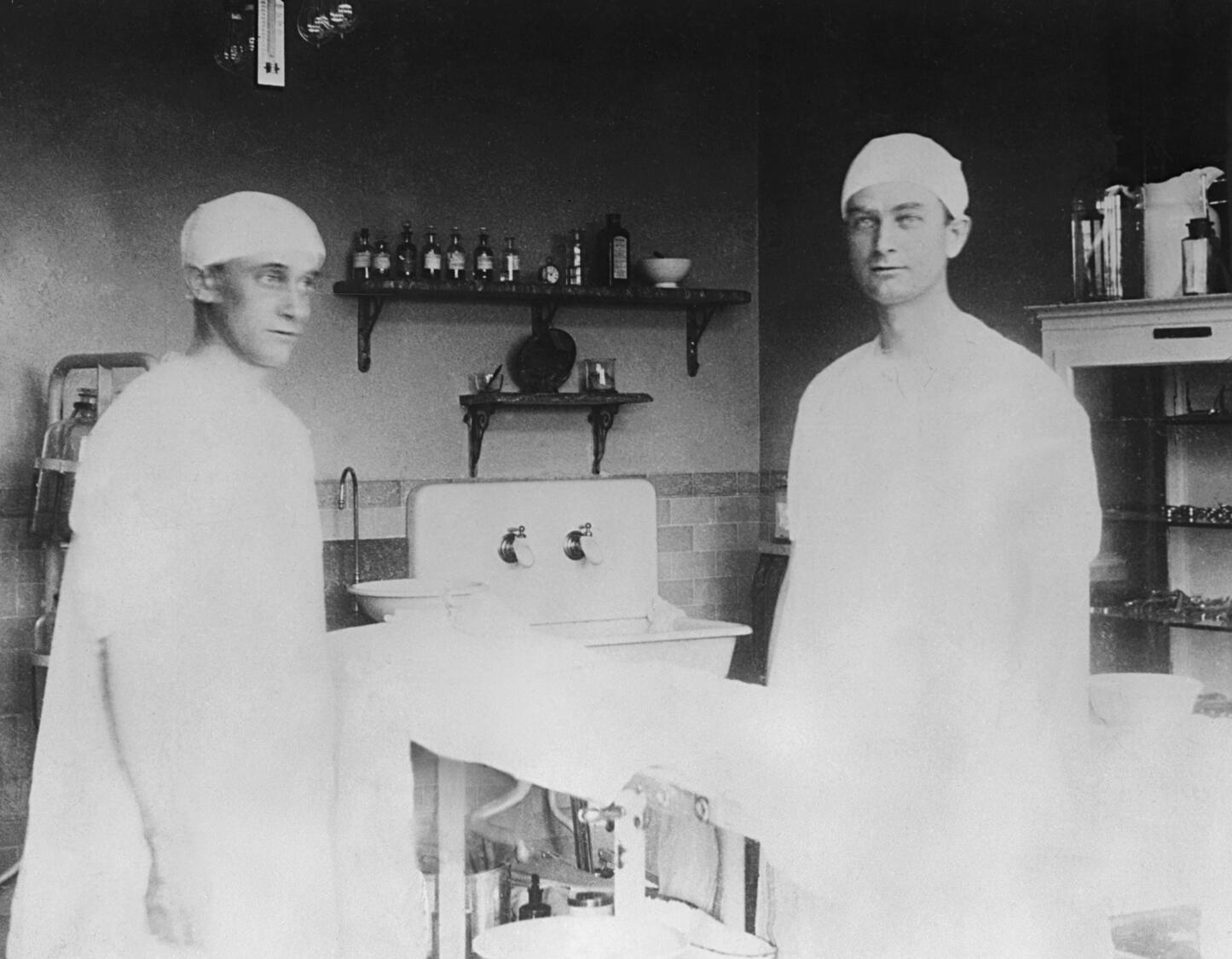
The Start of Mayo Clinic: A Remarkable New Movie
Please note that there will not be Centennial Updates for the next two weeks. We’ll pick back up on October 24th.
During the past year we have learned about many aspects of the start of anesthesiology. We also have highlighted some of the important steps that led to Mayo Clinic’s origin in Rochester, Minnesota.
This past month, the Mayo Clinic History & Heritage Center released a new movie, “An Adventure in Medicine: The Story of the Mayo Brothers” (An Adventure in Medicine: The Story of the Mayo Brothers (mayoclinic.org). This movie is 29 minutes in duration and tells the story of William Worrell Mayo; his journey with family to Rochester; the return of Will and Charlie Mayo to Rochester after completing medical school; and the rise of the uniquely new, multi-disciplinary Mayo Clinic. It is well worth watching as it will provide you with insights into the start and evolution of our Mayo culture; the role of Mayo physicians, scientists, nurses, and other personnel in developing innovations that continue to impact the practice of medicine; and the spirit of community and generosity that led to the Mayo brothers giving much of their personal wealth to create the Mayo Foundation.
I highly recommend that you pour a cup of coffee or tea and spend a half-hour watching the movie. You’ll hear short clips about early nurse anesthetists Edith Graham and Alice Magaw and the story of 12-year-old Charlie being emergently put into duty to anesthetize a patient on a kitchen table. The latter story is described in more detail in a 34-minute video, “Our Father Taught Us: A Journey Towards Teamwork” (Our Father Taught Us: A Journey Toward Teamwork | Films | Mayo Clinic History & Heritage).
There currently are 31 excellent Mayo Heritage movies available online. You may find them at Mayo Clinic Heritage Films | Mayo Clinic History & Heritage.
Mystery Photos
Last week’s Mystery Photos were James R. Hebl, M.D. and Douglas R. Bacon, M.D.

James R. (Jim) Hebl, M.D. was born in Mankato, Minnesota on January 1, 1969. He graduated from Saint John’s University (MN) in 1991 and earned his M.D. at the University of Minnesota in 1995. Jim completed his anesthesia residency, an NIH Clinical Research fellowship, and a Regional Anesthesia fellowship in Rochester. He joined our department as a staff member in 1999.
Jim made many contributions to our department’s clinical practices during his first 17 years on staff. Under the mentorship of leaders such as Drs. Denise Wedel, Terre Horlocker, and Bob Lennon, he gained national visibility in regional anesthesia and acute pain medicine. He was the program chair for the Annual Meeting of the American Society of Regional Anesthesia (ASRA) in 2010; chaired ASRA’s Practice Advisory on Infectious Complications Associated with Regional Anesthesia and Pain Medicine, was an associate editor for the journal Regional Anesthesia and Pain Medicine (RAPM), and served as a member of the ASRA Board of Directors. In 2010, Jim and Dr. Bob Lennon co-edited a textbook, Mayo Clinic Atlas of Regional Anesthesia and Ultrasound-Guided Nerve Blockade.
In our Rochester department, Jim was instrumental in changing our orthopedic surgical practice. For example, he co-directed a multidisciplinary team to develop the Mayo Clinic Total Joint Regional Anesthesia Clinical Pathway. He served in a variety of leadership roles, including chair of our Methodist North Division, program director of our Regional Anesthesia Fellowship, chair of our Community Division, and chair for Integration and Practice Convergence. In Mayo Clinic’s Midwest, he has been a member of its Executive Operations Team and a number of its highest-level committees.
In 2016, Jim had the opportunity to “change careers” without leaving Mayo Clinic when he was appointed as a Regional Vice-President of our Mayo Clinic Health System (MCHS). This transition brought him back to his hometown of Mankato. In this role, Jim currently serves as the senior physician executive for five of our MCHS hospitals, 22 primary and specialty care clinics, and nearly 4,000 staff across southern Minnesota. In May 2024, Jim and his team opened a new $155 million hospital expansion project in Mankato, which is the largest MCHS capital project thus far in Minnesota. With these internal leadership roles, Jim has become a certified executive coach and a new member of Mayo Clinic’s executive coaching team.
On a state and national level, Jim served as president of the Minnesota Society of Anesthesiologists, director and board member of the American Society of Anesthesiologists (ASA), and has been the ASA’s representative to the American Academy of Orthopaedic Surgeons (AAOS).
Jim and his wife, Heather, live in Madison Lake, Minnesota, and have 3 children—Zachary, Matthew, and Gabriela (Gabi). Tragically, Gabi passed away in a car accident in 2022. During his free time, Jim enjoys traveling internationally, cooking, reading, and enjoying time with Heather and family and friends at their lake home.

Douglas R. (Doug) Bacon, M.D. was born in Buffalo, NY on January 28, 1959. He graduated from the State University of New York (SUNY) at Buffalo in 1981 and then earned his M.D. at SUNY Stony Brook’s School of Medicine in 1985. Doug interned at Millard Fillmore Hospital in Buffalo, followed by a residency in Anesthesiology at SUNY Buffalo Affiliated Hospitals. He joined the Roswell Park Cancer Institute as an anesthesiologist and completed a Master of Arts in History degree at SUNY Buffalo in 1994. His interest and training in medical history has played a major role in his career.
During his clinical career, Doug practiced in a variety of academic settings and institutions, including the Roswell Park Cancer Institute, the Buffalo Veterans Administration Medical Center (VAMC), our department in Rochester, Wayne State University, and the University of Mississippi Medical Center. At SUNY Buffalo, he had the honor of being the vice-chair for Education. He also served as Chief of Anesthesia Services of the New York Upstate VAMC from 1995 through 2000. In April 2001, I was able to persuade Doug to move to Rochester with the goal of establishing an anesthesia history program in Rochester and supporting scholarship for trainees and early career staff in that field. During his 11 years in our department, Doug published anesthesia history papers with a remarkable 63 of our trainees and colleagues and established Mayo Clinic as an international leader in the field. Doug served as our department vice-chair of Faculty Development from 2008 through 2012. He is our first anesthesiologist to become professor of both Anesthesiology and the History of Medicine.
In 2012, Doug moved to Detroit where he spent two and a half years as chair of anesthesiology at Wayne State University. He subsequently moved to Jackson, Mississippi and spent 8 years as chair of the Department of Anesthesiology at the University of Mississippi. Doug became visually impaired in June 2022. This impairment ended his clinical career, and he left the University of Mississippi. We were fortunate to entice him to join our Rochester department as an administrative consultant at that time, and he has helped lead our current Centennial Project and represent Mayo Clinic in anesthesia history meetings nationally and internationally.
Doug’s research interest has focused on the organizational history of anesthesiology during the first half of the twentieth century and the challenges of creating the definition of and the infrastructure for the specialty. He has been a prolific author in anesthesia history and has become one of the world’s leading authorities in the field. He was honored as the 2012-2016 Laureate of the History of Anesthesiology, an international career award given by the Wood Library Museum of Anesthesiology (Dr. Douglas R. Bacon - Wood Library-Museum of Anesthesiology (woodlibrarymuseum.org). Doug served as secretary of the WLM from 2001 through 2008 and has been a council member of the History of Anaesthesia Society, United Kingdom. He also served as president of the Anesthesia History Association from 2006 through 2010.
Doug has been a highly visible spokesperson for anesthesiology during his career, serving as editor of both the New York Society of Anesthesiologists’ Sphere newsletter and the ASA Newsletter. He has been an associate or section editor for journals such as the Bulletin of the History of Medicine, Regional Anesthesia and Pain Medicine, and the Journal of Clinical Anesthesia. He currently serves as secretary of the Academy of Anesthesiology.
Doug now makes his home in East Amherst, New York, a suburb of Doug’s hometown of Buffalo. He and his wife, Dr. Melissa Bacon, have 4 adult sons and a middle-school-aged daughter.
Mystery Photo Contest Winner

The winner of the Mystery Photo contest in Update #55 was Sherry Alexander.
Here are this week’s Mystery Photos. Reminder: We feature two individuals each week for the Updates. To be placed into the Mystery Photo Starbucks contest, you will need to correctly guess at least one of the featured individuals. If you identify both of them, you will double your chances of having your name drawn.
Please email your response at warner.mark@mayo.edu within 3 days of this update. I will also need your name and contact information. All correct responses will be placed into a Monday morning drawing for a $10 Starbucks card. Only one winner per individual over the 80 weeks of Mystery Photos. If you win a weekly drawing, however, please keep submitting your responses. An overall winner (with the most correct responses in the series of 80 Updates) will receive a $100 Starbucks card.
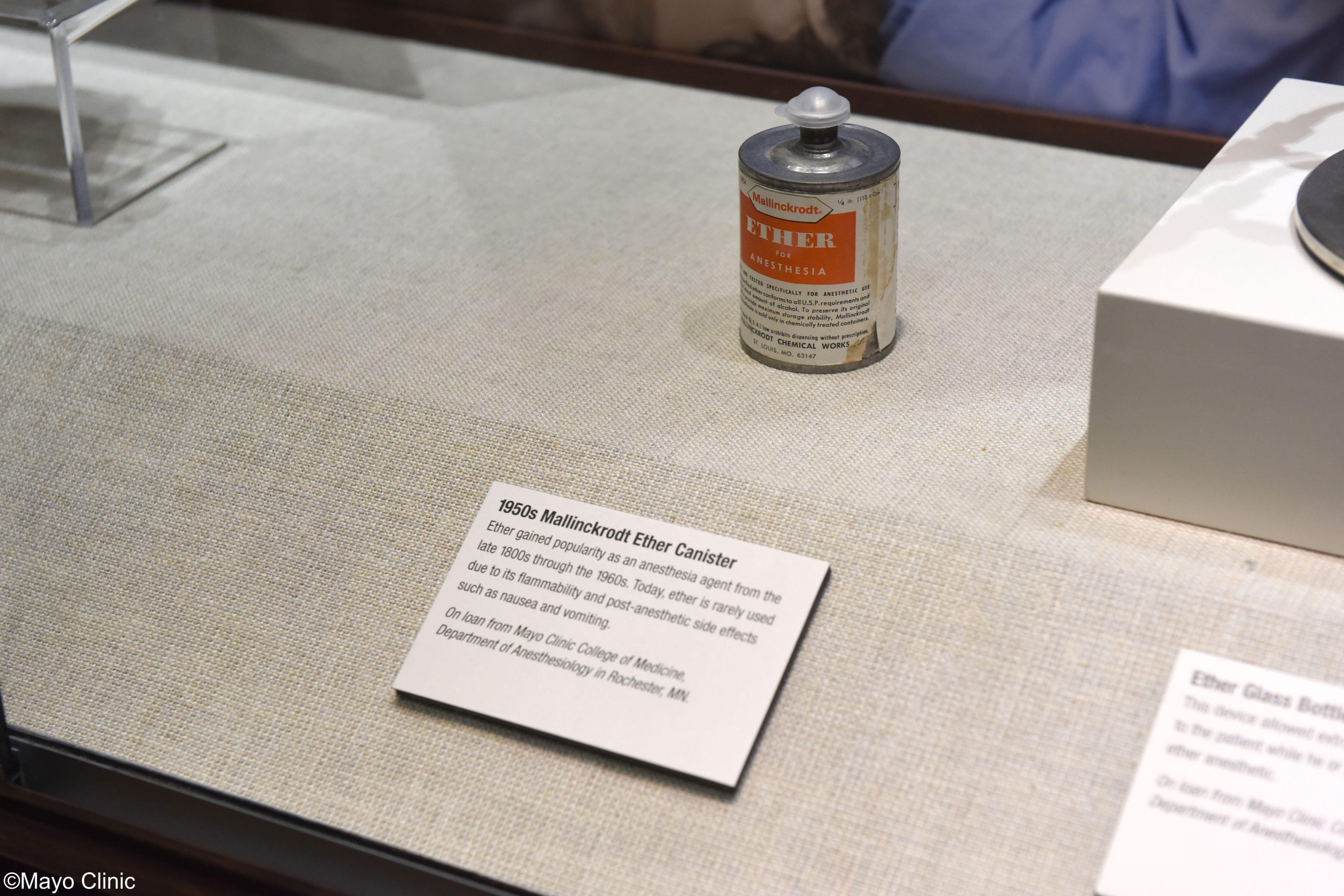
Ether Day, October 16: Mayo Clinic’s Role in the Use of Ether in the U.S.
On October 16, 1846, dentist Thomas Green Morton first publicly demonstrated the use of ether as an anesthetic in the surgical theater of the Massachusetts General Hospital. The October 16th date is now celebrated annually in Boston as Ether Day and around the world as World Anaesthesia Day. This first public demonstration of ether is summarized in detail by Dr. Paul Firth in a 2022 article in the Annuals of Surgery.
The introduction of ether was one of the two major advances in surgery in the 19th century, the other being the development of antisepsis by Joseph Lister. It was so important that communication about its successful use on October 16th spread remarkably quickly. It spread so quickly, in fact, that the first communications about ether have garnered considerable interest. A very interesting, even amusing, story about ether’s first use in London can be read at How Ether Transformed Surgery from a Race against the Clock | Scientific American.
William Worrell Mayo likely learned about ether anesthesia when in medical school at the University of Missouri (he graduated in 1854). He gained more experience with it during the Civil War period as he served the Minnesota Volunteer Army as the physician for its recruitment station (first in Mankato and then in Rochester). He learned more about it from physicians who used it on the battlefields of that war. Over his subsequent years, he used ether as his primary general anesthetic as chloroform and other inhaled agents proved to be too unsafe. As his sons took over all of the family’s surgical practice in the mid-1880s, he provided ether anesthesia to many of their patients. By age 70, he decided to reduce his time in medicine and trained a young nurse, Edith Graham, to provide ether for his sons’ patients who required general anesthesia. This training took place in autumn 1889, and Edith became the Mayo brothers’ anesthetist in December of that year. More about this story can be found in Centennial Update #12, November 23, 2023.
Edith Graham married Dr. Charlie Mayo in 1893. Fortunately, she trained a nursing school classmate, Alice Magaw, before marrying Charlie. It was Alice who became one of the world’s most famous anesthetists of the time and established expectations for success within the U.S. with the use of ether. Her 1906 publication, “A Review of Over Fourteen Thousand Surgical Anaesthesias” set the bar for the safe use of ether as she reported no deaths attributable to these ether anesthetics. This and subsequent reports of low anesthesia-related mortality rates for ether, several of which came from the Mayo brothers and Alice, played a significant role in the establishment of ether as the primary general anesthetic in the U.S. and elsewhere for more than a century.
Ether remained in use at Mayo Clinic until 1978. Dr. Paul Leonard and Lucille (Lucy) Chen were the last of our staff to use ether.
Mystery Photos
Last week’s Mystery Photos were Christina M. Pabelick, M.D. and Y.S. Prakash, M.D., Ph.D.

Christina M. Pabelick, M.D. was born in Dusseldorf, Germany where her father was a private practice internist and her mom supported the practice while bringing up Christina and her sister, Judith. Both children were expected to pursue rewarding professions. Judith became a lawyer while Christina pursued medicine at Heinriche Heine University in her hometown (our colleague, Dr. Thomas Comfere, went to the same school a bit later). After earning her M.D. in 1988, Christina was an intern in pediatrics in Dusseldorf. She subsequently trained in anesthesiology and critical care at Goethe University in Frankfurt under the mentorship of the chair Prof. Rafael Dudziak. Upon completion of her training in 1995, Christina received funding from the German government to do a research fellowship at Mayo Clinic. Because Dr. Kai Rehder in Rochester knew Dr. Dudziak, a connection was made with Dr. David Warner. Christina joined David’s lab in 1995.
The first few years as a fellow in David’s lab were tremendously productive for Christina. Beyond the great research on anesthestics and bronchodilation, she got to meet and interact with colleagues such as Drs. Tony Jones, Bill Perkins, and Gary Sieck. Perhaps most importantly, she also met and worked with Dr. Y.S. Prakash, a postdoctoral fellow in Gary’s lab. Collaborations led to Prakash and Christina working together. Their work and growing personal relationship led to a difficult decision for Christina to not return to Germany to become an anesthesiologist “back home.” To our good fortune, we were able to entice Christina to become a resident in our anesthesiology training program. She completed her residency in 2003.
Having Christina as an anesthesia resident during my time as chair of the department allowed me to better understand and appreciate the difficulties that foreign medical graduates encounter, especially those who have already been highly trained in their home countries but are subject to our rules regarding residency training. Using Christina as a case study and leveraging my position at the time as a director of the ABA, we were able to modify the ABA’s certification requirements and its rules for U.S.-based residency training. Essentially, we were able to reduce the re-training time for individuals from countries with training programs comparable to those in the U.S.
Christina spent her 4 years of residency training at Mayo while also helping Prakash go through medical school at the University of Minnesota from 1998 through 2002. They spent a good amount of their free time on the road between Rochester and the Twin Cities. This shuttle romance also helped them consolidate their research programs during this time. During her residency training, we were able to arrange for Christina to become trained in neonatal cardiac critical care at the world renown Great Ormond Street Hospital in London.
When Christina came on staff in 2003, she quickly set up her own research program in airway biology, focusing on what she has been most passionate about: the care of the most vulnerable, especially children. She has spent the past 20 years since working on exciting areas in airway biology at the extremes of age, from prematurity through aging. Her group has explored clinically relevant topics like cigarette smoke and nicotine exposure, the effect of hydrogen sulfide as a bronchodilator, and more recently the impact of Down Syndrome in premature lungs.
Christina is now a Professor of Anesthesiology and Physiology. She distributes her efforts between research, mentoring, administration and OR practice in the Pediatric Anesthesia Division. She has previously served as the Pediatric Anesthesiology fellowship director and as Chair of the Mayo Animal Care and Use Committee (IACUC), a position previously held by stalwart anesthesiologists such as Drs. Bill Lanier and Philippe Housmans. She has been remarkably successful in her research lab. Her success has been recognized in numerous ways, including her selection as chair of the ASA’s Committee on Research, the Scientific Advisory Board of the Association of University Anesthesiologists, and the NIH’s Surgery, Anesthesia, and Trauma Study Section. Christina is also an inductee into the Foundation for Anesthesia Education and Research (FAER) Academy of Research Mentors. Indeed, mentoring is a passion for Christina, and she has served as mentor for many of our junior faculty and emerging leaders. She recently became the Principal Investigator on an NIH T32 training grant that will keep her going in terms of her mentoring. She was appointed this past month as our department’s Vice-Chair for Research.
In her spare time, Christina enjoys working in the garden out in Elgin, Minnesota. She and Prakash now are the owners of the old “Dozois place” (many of you may know of Dr. Roger Dozois, emeritus professor of Colorectal Surgery and his son, Eric, current chair of our Division of Colorectal Surgery). Christina loves taking care of many cats who are all “momma’s boys and girls,” the chickens who think they run the place, the rental goats who want to check out the chicken coop, and the many other animals and birds that know of Christina’s generosity. She and Prakash enjoy traveling when they can, visiting family in Germany and Dubai, touring historic places, and photographing nature.

Y.S. Prakash, M.D., Ph.D. was born in India and grew up in multiple places in Western India as his engineer father moved every few years to try something new in the field. After high school, he gained entrance into the highly competitive Indian Institutes of Technology (IITs) and finished a degree in Electrical Engineering from IIT Bombay in 1988. He garnered a scholarship from the University of Southern California (USC) in Biomedical Engineering (BME). While at USC, he joined the lab of Dr. Gary Sieck, our distinguished colleague who was then a faculty member at that institution in BME working on respiratory physiology. As you know, Gary got recruited by Dr. Kai Rehder to come to Mayo Clinic in Rochester in 1990 to join our department as Vice-Chair for Research.
Although Prakash loved sunny Southern California, his USC chair convinced him of this amazing place called Mayo Clinic where he could do world-class research working with amazing teams with amazing resources (Prakash’s own words). So, after earning his M.S. in BME in 1990 and having never actually visited Rochester or the Mayo Clinic, Prakash packed his worldly belongings in his little Brazilian-made Volkswagen Fox and drove cross-country, camping in multiple national parks along the way. After an all-night driving marathon from Yellowstone National Park through Wyoming, South Dakota and Minnesota (well before the age of GPS, using AAA TripTiks), he arrived in Rochester: and drove right through it not realizing how small the town actually was. Ha!
After this pass-through introduction to Rochester and turning around back to Rochester, Prakash got his first taste of the Mayo way when he realized that nobody at the Mayo Graduate School knew he was coming! And that he was not going to get a paycheck until the paperwork was cleared! Kai Rehder picked up a phone and with his usual soft and gentlemanly manner convinced someone to give Prakash a $500 check so he could survive for at least his first week.
Prakash spent the next 4 years at Mayo Clinic in Gary Sieck’s lab getting his PhD in physiology (1994). Along the way, a lot of us in the department got to know Prakash for his quirky ways and his fun attitudes. And never following the Mayo dress code. However, we also got to know him for his research and his potential as he then took a postdoctoral research fellowship in our department. It was during this time that Prakash met Dr. Christina Pabelick who was then a research fellow in Dr. David Warner’s lab down the hall from the Sieck lab in St. Marys Hospital. They worked together for a while before they got together with a lot of our encouragement and are now happily married.
And that’s where things got interesting. Prakash was fascinated by all the medicine around him and decided to apply to medical school while he was looking to get NIH funding as well. To his good fortune, he got both an NIH grant and admission to the University of Minnesota medical school. He is one of the few medical students in the U.S. to have ever been a Principal Investigator on an NIH R01 grant and the only one at that time. Although it was a little daunting, Prakash decided to pursue both medical school and his research simultaneously. We were fortunate to get Prakash as an anesthesia resident four years later (by then Christina had finished re-doing her anesthesia training to meet certification criteria and was ready to come on staff). The rest is history, so to speak.
Prakash is now a Professor of Anesthesiology and Physiology. He is the Chair of the Department of Physiology and BME and the Vice-Dean of Research for Mayo Clinic. He is not the first member of our department to be the chair of the Mayo Clinic Department of Physiology and BME; Gary Sieck served in that role previously. We are very proud of both. Remarkably, Prakash is doing this while working part-time in the clinical practice. He is a named Clinician-Investigator at Mayo (only the 3rd from a total of 5 anesthesiologists in our department to have gotten that position). He distributes his efforts between research, administration and OR practice in the Central Division at St. Marys Hospital.
Prakash directs a longstanding NIH-funded program in lung disease research, focused on pathophysiology of neonatal wheezing, asthma, and pulmonary vascular disease, exploring the role of inflammation, environmental factors, and life events from prematurity through aging. His lab is funded by 4 R01s and intramural grants. He has served as Editor-in-Chief of Comprehensive Physiology (formerly Handbook of Physiology) and is an Associate Editor of the Am J Physiol Lung Cell Mol Physiol. He served as chair of the NIH Lung Cellular, Molecular, and Immunobiology Study Section. He has served in leadership positions on ASA Committees, AUA, American Thoracic Society, and American Physiological Society. He is the first and only anesthesiologist from Mayo Clinic to be inducted into American Society for Clinical Investigation (ASCI) and is also an inductee into the Foundation of Anesthesia Education and Research (FAER) Academy of Research Mentors. He is the current chair of the Board of Trustees of the IARS. Other Mayo Clinic anesthesiologists to serve as chair of the IARS include T. Harry Seldon (1955); Emerson Moffitt (1977); J. Tom Martin (1979); E. Paul Didier (1985); Adrian Gelb (2003); Denise Wedel (2016); and K. Tony Jones (2020).
With all his spare time, Prakash and Christina enjoy their little piece of heaven out in Elgin, Minnesota in the old “Dozois place” (see summary of Dr. Christina Pabelick above), working in the garden, taking care of their cats, chickens, rental goats, and the many other animals and birds that flock to their sanctuary. They enjoy traveling when they can, visiting family in Germany and Dubai, touring historic places, and photographing nature.
Mystery Photo Contest Winner

The winner of the Mystery Photo contest in Update #56 was Chelsey Aubart.
Here are this week’s Mystery Photos. Reminder: We feature two individuals each week for the Updates. To be placed into the Mystery Photo Starbucks contest, you will need to correctly guess at least one of the featured individuals. If you identify both of them, you will double your chances of having your name drawn.
Please email your response at warner.mark@mayo.edu within 3 days of this update. I will also need your name and contact information. All correct responses will be placed into a Monday morning drawing for a $10 Starbucks card. Only one winner per individual over the 80 weeks of Mystery Photos. If you win a weekly drawing, however, please keep submitting your responses. An overall winner (with the most correct responses in the series of 80 Updates) will receive a $100 Starbucks card.
Dear alumni, staff, and trainees in the Mayo Clinic Department of Anesthesiology and Perioperative Medicine and friends of the department,
Thank you for your readership and welcome to Update #58. This is going to be the next-to-last issue in this series of Centennial Updates. It has been a wonderful privilege to write these Updates over the past 14 months and to provide you with insights into the many contributions that the institution-wide department has made and will continue to make into the future. In many ways, our department helped shape the specialty of anesthesiology in the U.S. and influenced the specialty worldwide. We all should be proud of our department’s contributions to the specialty, patient safety, and Mayo Clinic.
I’ll provide more final thoughts in next week’s Update, the last of the series. In the meantime, please remember that we now have a remarkable, evolving department website on our history (Anesthesiology Department | Mayo Clinic | History and Heritage). Our archivist, Alec Thicke, and our history team will work in the coming months to ensure that the website continues to expand and serve as a repository for our history far into the future. For example, we will soon be adding digitized books (e.g., Art to Science, the book published in 2000 by Drs. Kai Rehder, Peter Southorn, and Alan Sessler that showcased the early history of our department), important publications and department newsletters, a set of webpages specifically related to our CRNA Alumni Newsletters, relevant photos, and all of our Updates.
You will find an announcement of the 2025 Spring Meeting of the Anesthesia History Association in a new section on our history website titled "Anesthesia History Association 2025 Annual Meeting".
Later this autumn and into Spring 2025, we will be hosting 3 extraordinary anesthesiologists who have leadership roles in the specialty and anesthesia history. They will be giving Grand Rounds in Rochester.
- Christine Ball, M.D., is an anaesthesiologist at Alfred Hospital in Melbourne, Victoria, Australia. She was the 2020-2024 Wood Library-Museum of Anesthesiology’s Laureate of the History of Anesthesiology. She also is the long-serving Honorary Curator of the Geoffrey Kaye Museum of Anaesthesia History. She will present on November 18, 2024.
- Peter J. Featherstone, M.B.B.Ch., is an anaesthesiologist and intensivist at Cambridge University Hospitals in England. He has won numerous awards in anesthesia history. He currently is the president of the History of Anaesthesia Society (Great Britain). He will present on December 9, 2024.
- David J. Wilkinson, M.B.B.S., is a retired consultant anaesthesiologist from St. Bartholomew’s Hospital in London. He was the 2008-2012 Wood Library-Museum of Anesthesiology’s Laureate of the History of Anesthesiology. He also served as president of the World Federation of Societies of Anaesthesiologists from 2008 through 2012. He will present on April 28, 2025.
Mayo Clinic: The American Society of Anesthesiologists and Mayo Clinic Leadership of the Society
John S. Lundy, M.D. was an important leader in the establishment of the American Society of Anesthetists in 1936. The society evolved in 1945 to the American Society of Anesthesiologists (ASA). Other Mayo alumni made major contributions to the early development and evolution of the ASA. During the 12-year period from 1941 through 1953, 5 Mayo anesthesiologists or alumni served as president of the fledging society. This remarkable run is unmatched by any other department of anesthesiology. More recently, however, the department has produced another excellent run of ASA presidents. Starting in 2000 and running through 2030, 6 of our colleagues will have served or will be serving as ASA presidents.
This past week, our own Jeff T. Mueller, M.D. was elected as ASA First Vice-President. This election starts a 4-year leadership role that will culminate in his serving as president in 2027. In addition, David P. Martin, M.D., Ph.D. was elected for another term as ASA Vice-President of Scientific Affairs. I believe that Dave will advance in his officer role and likely become our next Mayo colleague in the presidential line. He would serve as ASA president in 2030, if elected. Congratulations to Jeff and Dave on their contributions to the advancement of anesthesia safety, quality, and value and for continuing the long line of Mayo Clinic anesthesiologists who have led the ASA over the years.

- Ralph M. Tovell, M.D. (1941)

- John S. Lundy, M.D. (1946)

- Edward B. Tuohy, M.D. (1947)

- Charles F. McCusky, M.D. (1948)
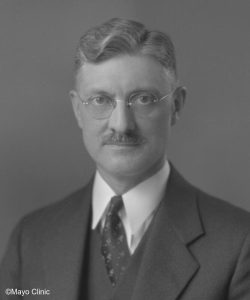
- Ralph T. Knight, M.D. (1953)
- John S. Hattox, M.D. (1980)

- Ronald A. Mackenzie, D.O. (2000)

- Mark A. Warner, M.D. (2011)

- John P. Abenstein, M.D. (2015)

- Daniel J. Cole, M.D. (2016)

- Jeff T. Mueller, M.D. (2027)

- David P. Martin, M.D., Ph.D. (2030, if elected)
Mystery Photos
Last week’s Mystery Photos were Stephen M. Brzica, Jr., M.D. and Michael T. Walsh, M.D.

Stephen (Steve) M. Brzica, M.D. was born on Victory in Europe (VE) Day, May 8th, 1945, in Sioux Falls, South Dakota. He was originally named Victor Emmanuel until his father returned from the war and he was renamed Steve, Jr. After graduating high school, Steve attended Creighton University and the Creighton Medical School. A rotating internship at the University of Missouri, Kansas City led him to meet Dr. Jerry Tuohy, a graduate of our Rochester anesthesiology residency program in 1962. Jerry was a classmate of remarkable anesthesiologists and alumni such Drs. Maurice Albin, Martha (Smith) Sessler, and Alan Sessler. Jerry convinced Steve to visit Mayo Clinic, and thus began Steve’s career in anesthesiology.
Steve became a Mayo Clinic resident in 1971, completing his anesthesiology training in 1974. While a resident, he spent much time in the research laboratory of department chair Dr. Richard (Dick) Theye. He enjoyed his time with Dr. Theye but quickly realized research was not in his future. As he neared the end of his training, Dr. Theye called Steve to talk about joining the staff. He presented Steve with a proposal to take a year-long fellowship in Blood Banking (now days, Transfusion Medicine). Steve would then join the staff, half time in the Mayo Blood Bank and half in anesthesia. Dr. Theye crafted his request in such a way that he knew Steve couldn’t turn it down. For example, Steve and his wife, Sheila, had four children; Dr. Theye arranged for Steve to be appointed as an Associate Consultant while a fellow, a financial inducement that worked.
Steve joined our Mayo Hematology fellows working in the Blood Bank for his fellowship. At that time, the Blood Bank was located on the 9th floor of the Plummer Building. There, the fellows and staff would diagnose relatively recently described antigen/antibody interactions that were responsible for blood transfusion mismatches. For emergency requests for blood, the elevators in the Plummer Building at that time were slow. On weekends of call, Steve would run up 9 stories of the Plummer Building to begin crossmatching and testing. That year as a fellow Steve lost 50 pounds! It apparently was worthwhile -- the following year, he passed the board exam given by the American Board of Pathology in Blood Banking.
In the Blood Bank, Steve began working with exceptional transfusion leaders such as Dr. Howard Taswell. They spent their time studying and writing about transfusion practices in surgery. Specifically, they worked on the issue of cell salvage during surgery, trying to find what damage was being done to the cells that were to be re-transfused. They were never able to find the appropriate tests to determine the status of the cells that were to be transfused, but the company marketing the early version of what is now the Cell Saver® was able to convince others to use the product without this information. Steve soon became a very popular speaker on transfusion therapy at many continuing education programs. During this time, he co-authored the chapter on transfusion in Dr. Ron Miller’s first edition of his textbook, Anesthesia (1981).
Once Steve was on staff and while working at Methodist Hospital in 1977, Dr. Theye asked him to go to lunch. He then told Steve that he had self-diagnosed himself with ALS and was heading to see a neurologist that afternoon. Sadly, Steve never saw him again as Dr. Theye died shortly thereafter on November 21st of that year. It was a difficult time for Steve since Dr. Theye and he had an unusually strong bond. For example, in 1975 when Steve was taking his oral board examination in anesthesiology, Dr. Theye, a director of the American Board of Anesthesiology (ABA), arranged for Steve to be examined on a Friday, the last day of a week of examinations. The night before Steve’s examination, Dr. Theye came to his hotel room with two suitcases of dirty clothes. Dr. Theye was going bone fishing in the Florida Keys with Dr. John (Jack) Michenfelder immediately after the examination week concluded. He wanted Steve to take the suitcases back to Rochester and give them to Jane Post, Dr. Theye’s secretary. Steve did, and Jane said, “Dr. Theye wanted you to know that you passed the exam.” Probably a fair trade -- dirty clothes carrier service for early notification about the outcome of Steve’s examination. As a former ABA director, I believe that Dr. Theye’s insider information to Steve would probably not be ethical by today’s standards, but it was probably marginally acceptable in 1978.
Things changed dramatically for Steve after Dr. Theye’s ALS diagnosis and rapid death. With child #5 on the way, Steve and Sheila decided that he should join Mayo anesthesiology alumnus Dr. Bill Cant in a new outpatient surgical practice in St. Paul in 1979. Bill was a pediatrician in Red Wing, Minnesota who transitioned to our anesthesiology residency in 1972 and completed his training with Steve in 1974. Our own Dr. Allan Gould had told Steve and Bill that anesthesia in the Cities was in the “dark ages” when they moved to St. Paul. They quickly found out that they were in great demand, not so much for their new surgical center (the St. Paul Surgery Center), but for their anesthesia skills. They soon found themselves working at Shriner’s Children’s Hospital, and Steve also took a part-time job working with medical students and residents at Hennepin County Medical Center. Once there, he taught them to use new inhalation anesthetics such as enflurane and isoflurane. At the time, no one else was using these new drugs in the Twin Cities.
In 1982, Fairview Southdale Hospital in Edina, Minnesota asked Steve and Bill to start a same-day surgical facility to prevent others like them from starting a competing outpatient surgical facility in the area. They did this and added two additional Mayo anesthesiology alumni, 1974 fellow resident classmates Drs. Bob Venegoni and Jerry Edelman. Steve remained in this Edina practice until his retirement in 2017.
Regarding Steve’s career in blood banking, after leaving Mayo Clinic in 1978, Dr. Taswell asked Dr. Herb Polesky, director of Memorial Blood Bank in Minneapolis, to contact Steve. This started a 20-year relationship for Steve with that organization. Those initial years with the blood bank were exciting since Dr. Polesky was active in developing tests for the AIDS virus and transfusion services across the country were tasked with preventing transmission of the virus through blood transfusions. Steve served on the Board of Directors of Memorial Blood Centers of Minnesota starting in 1981. He oversaw the restructuring and expansion of Memorial Blood Bank during his time on the blood center’s board. He subsequently served as president of that board from 1993 through 1995. He was recognized by Memorial Blood Centers of Minnesota with its 1997 Service Award and its Presidential Award for Outstanding Vision and Leadership.
Steve and Sheila, a former nursing school instructor at Mayo Clinic, have five children and fourteen grandchildren. They reside in Bloomington, Minnesota. They now spend their time visiting the grandkids in Omaha, Nashville, and Washington, DC. Steve enjoys playing golf at Hazeltine National Golf Club and occasionally consulting on anesthesia issues for Minnesota Gastroenterology, a large group gastroenterology practice in Minnesota and Wisconsin.

Michael (Mike) T. Walsh, M.D. was born in Gary, Indiana, the 4th of 6 children and the first in his family to become a physician. Mike graduated from the University of Notre Dame in 1984 and earned his M.D. at the Indiana University School of Medicine in 1988. He was a resident in anesthesiology at the Cleveland Clinic from 1990 through 1993. Mike joined the Cleveland Clinic faculty after completing his training, focusing primarily on ENT anesthesia and difficult airway management. In a few short years he was appointed as Head of the ENT Anesthesia Section and co-developed the Cleveland Clinic Difficult Airway Workshop. He was also part of the team that performed the first laryngeal transplant in the U.S.
In 1998, Mike moved back to Indiana to be closer to family. He served as Medical Director for the SurgiCare Ambulatory Care Center in Bloomington, Indiana from 1998 through 2002. It was there that Mike became involved in organized medicine generally, and ambulatory anesthesia specifically. He served on the Board of Directors of the Indiana Society of Anesthesiologists and joined a number of committees in the Society for Ambulatory Anesthesia (SAMBA).
After four years, Mike realized that he missed the excitement and variety of academic anesthesia and came to the Mayo Clinic in Rochester in 2002 to help Drs. Mary Ellen Warner and Ron Mackenzie in the newly formed Gonda 7 outpatient practice. His second practice site in the department was in the Methodist South Division (currently the Jacobson Division). Over time, the balance between Methodist South and Gonda practices shifted towards the hospital. He was appointed Chair of the Methodist South Division in 2006 and served in that role for the next ten years.
Soon after arriving in Rochester, Mike became actively involved in the Minnesota and American Society of Anesthesiologists. He became Secretary/Treasurer of the MSA in 2005 and joined the board of directors. He subsequently advanced to serve as the President of MSA in 2014. As part of his MSA roles, he was one of the society’s representatives to the ASA’s House of Delegates for 10 years.
Mike’s involvement in ASA focused on ambulatory anesthesia. He spent several years on the ASA’s Educational Track Subcommittee on Ambulatory Anesthesia and 18 years on the Ambulatory Care Committee; 4 years as its chair. He has been one of the ASA’s most prominent speakers on ambulatory surgery and anesthesia during the past 15 years. Mike’s SAMBA journey began almost 30 years ago and has been an important part of his career. He started on SAMBA’s Office-Based Anesthesia Committee and, over the years, he served on almost every SAMBA committee, chairing quite a few. Mike joined the SAMBA Board of Directors in 2010 and ascended to the society’s presidency in 2017. The colleagues, mentors, and friends he met along the way have been a great source of joy in his career. He was honored by SAMBA in 2020 with its Distinguished Service Award. He had the added privilege of having his daughter, Emily E. Walsh, M.D., present him with the award. Emily currently is a resident in our department in Rochester and, at the time of the award, was a medical student member of SAMBA.
Mike spent several years involved in accreditation issues in ambulatory surgery and was the ASA’s representative to the Ambulatory Surgery Division of the Joint Commission. He also represented ASA on the Board of Directors of the American Association for Accreditation of Ambulatory Surgery Facilities.
Outside of anesthesia, Mike’s interests include spending time with his wife, Liz, and Emily. Mike and Liz enjoy travel and literature. Mike admits to being addicted to golf; Liz is not yet addicted to it but is patiently learning to play.
Mystery Photo Contest Winner
The winner of the Mystery Photo contest in Update #57 was Sher-Lu Pai.

Here are this week’s Mystery Photos. This is the final week of Mystery Photos. There are four this time. To be placed into the Mystery Photo Starbucks contest, you will need to correctly guess at least one of the featured individuals. If you identify more than one of them, you will increase your chances of having your name drawn.
Please email your response at warner.mark@mayo.edu within 3 days of this update. I will also need your name and contact information. All correct responses will be placed into a Monday morning drawing for a $10 Starbucks card. Only one winner per individual over the 80 weeks of Mystery Photos. If you win a weekly drawing, however, please keep submitting your responses. An overall winner (with the most correct responses in the series of 59 Updates) will receive a $100 Starbucks card.

Thank you for your readership and welcome to Update #59, the final issue in this Centennial Project series. It has been a privilege to be able to provide you with insights into our department’s important contributions to the specialty and medicine, plus have fun with writing the long line of Mystery Photos stories. In the future, additional historical insights, photos, and stories will continue to be placed into our department’s history website, Mayo Clinic | Anesthesiology | Anesthesia History Association 2025 Annual Meeting. For those who want a quick reminder of our department’s proud history, I have prepared a very brief Mayo Clinic | Anesthesiology | Anesthesia History Association 2025 Annual Meeting. You are free to use any part of it (or all of it) for your own presentations. It can also be found on our department’s history website.
This past June 6th, I wrote a summary of a number of the key accomplishments and innovations of the department through 2000 (Centennial Update #40). I’ve reproduced that list here with minor modifications:
- 1904: Alice Magaw publishes a series of 14,000 anesthetics without an intraoperative death, a remarkable and almost unfathomable achievement at that time.
- 1920: Gaston Labat joins Mayo Clinic and becomes the country’s leading advocate for the use of regional anesthesia and a founder of the original American Society of Regional Anesthesia.
- 1925: John Lundy develops the Mayo Clinic’s Section on Anatomy, using dissections to teach regional anesthesia techniques.
- 1926: Lundy coins the term “balanced anesthesia” and advocates for its use.
- 1929: Lundy pulls together 15 leading academic anesthesiologists from the U.S. and Canada; the Anesthetists’ Travel Club is formed.
- 1933: Lundy establishes the Mayo Clinic’s intravenous fluid, blood, and medication service.
- 1934: Lundy and Charlie Adams publish on cold storage of citrated blood; the nation’s first blood bank is established.
- 1935: Lundy reports the successful trial of sodium pentothal and advocates for its use; it becomes the leading anesthetic induction agent for more than 5 decades.
- 1935: Lundy and Charlie Adams promote a hemoglobin transfusion trigger of 10 mg/dl; although debatable, this value stands the test of time for more than the next half century.
- 1938: Lundy plays a leading role in founding the American Board of Anesthesiology, a sub-board of the American Board of Surgery at its founding.
- 1940: Lundy is the country’s leading advocate for the successful establishment of a Section on Anesthesia within the American Medical Association.
- 1942: Lundy starts the Mayo Clinic’s first post-anesthetic care unit (PACU) and advocates for PACU development across the U.S. and Canada.
- 1942: Lundy starts one of the nation’s “90-Day Wonders” training courses for new physicians to learn anesthesia during WWII.
- 1944: Ed Tuohy introduces the epidural catheter technique.
- 1948: Florence McQuillen, the Mayo Clinic supervisor of nurse anesthetists, joins the AANA and serves 22 years as the association’s executive director.
- 1950: David Massa produces the world’s first intravenous catheter, an innovation considered to be one of the greatest advances in medicine in the 20th century.
- 1955: Bob Patrick, Albert Faulconer, and Emerson Moffitt are part of the Mayo Clinic team that perfect the Mayo-Gibbons heart-lung machine and advance cardiac surgery.
- 1967: Kai Rehder discovers the metabolism of halothane and its connection to halothane hepatitis.
- 1968: John (Jack) Michenfelder coins the subspecialty name, “neuroanesthesia,” and leads advances in the field.
- 1972: Sait Tarhan describes the risks of perioperative myocardial infarction (MI) and advocates for 6 months between MI and general anesthesia for elective procedures.
- 1973: Gerry Gronert discovers the association between succinylcholine and hyperkalemia when used in patients who have burns, disuse atrophy, and neurologic disorders.
- 1979: Joe Wang and Lee Nauss report on the first use of intrathecal narcotics.
- 1980: Gerry Gronert highlights triggers and treatment for malignant hyperthermia.
- 1985: Alan Sessler is a founder of the Foundation for Anesthesia Education and Research (FAER).
- 1985: John (Jack) Michenfelder and Alan Sessler are founding directors of the Anesthesia Patient Safety Foundation (APSF).
- 1996: Bill Lanier’s decade of study of augmentation of ischemic brain injury by minor changes of blood glucose transforms perioperative fluid practices worldwide.
- 1996: Roger White gets defibrillators into the vehicles of first responders, leading to Rochester having the world’s best survival results of ventricular fibrillation/cardiac arrest at that time.
- 1998: Denise Wedel and Terre Horlocker lead the development of guidelines on the use of anticoagulants in patients receiving regional anesthetics.
I realize that there are many important contributions to the advances in the specialty made by our department and our colleagues that I have not been able to highlight in the 59 Centennial Updates. Fortunately, our department’s compilation of historical information will continue far into the future within our website repository. I encourage you to view the material that is already in the website (link in the paragraph above) and let our archivist, Alec Thicke (thicke.alec@mayo.edu) or me (warner.mark@mayo.edu) know of any suggestions or corrections that you might have.
Our goal is to continually expand and improve the collection of stories related to our department in all sites. For example, we plan on developing site-specific webpages, not only for our departments in Jacksonville and Phoenix but also for our Mayo Clinic Health System sites. Please check our history website periodically and assist us with the collection of stories and information. These will help future generations understand how our Mayo Clinic Department of Anesthesiology and Perioperative Medicine made so many outstanding contributions to the specialty and medicine in both its first century and upcoming decades.
Mystery Photo Contest Winners from Last Week and the Full Centennial Celebration

The winner of the Mystery Photo contest in Update #58 was Nicole M. Lenort, RRT.

The overall winner of the Mystery Photo contest for the entire series of 59 Updates is Susan C. Quering, CRNA. Congratulations, Susie! Amazing effort! Susie correctly guessed 96% of the Mystery Photos. She gets the top prize of a $100 Starbucks gift card. It has been donated by a department supporter and grateful donor.
Mystery Photos from Issue #58
Last week’s Mystery Photos were Daryl J. Kor, M.D.; Carlos B. Mantilla, M.D., Ph.D.; Alan D. Sessler, M.D.; and Mark A. Warner, M.D.

Daryl J. (DJ) Kor, M.D. was born on March 24, 1974 in Marshall, Minnesota and was raised in nearby Cottonwood, northeast of Marshall. He attended St. John’s University in Collegeville, Minnesota from 1992 through 1996. While there, he played football for the legendary Coach John Gagliardi, the winningest coach in American college football. He participated in the 1993 and 1994 NCAA Division 3 semi-finals games and his teams posted a 90% winning percentage over his 4 years of play. He was recognized as both an All-Minnesota Intercollegiate Athletic Conference and an Academic All-American running back in 1995. Definitely an underachiever. Ha!
After graduating from St. John’s University in 1996, DJ attended the University of Minnesota School of Medicine, earning his M.D. in 2001. He was an anesthesiology resident here in Rochester from 2001 through 2005. At that time, he became a Mayo Clinic Scholar and was a critical care medicine fellow for a year. He joined the Rochester staff in 2006. During the next decade, he was honored with Distinguished Clinician and Teacher of the Year awards from trainees in the Department of Anesthesiology and from the Surgical Critical Care fellows. Along the way, he earned a Master’s degree in Clinical and Translation Sciences, receiving it in 2014.
DJ’s academic career has followed several unique paths.
- Data, Analytics, and Information Management.
He has played major roles in creating, expanding, and improving these three fields in the institution. Within the department he has served as the catalyst and medical director for creating our Perioperative Information Management, Implementation, and Analytics Program (PRIISM). This program is expanding to many other areas within the institution and providing data support that is extraordinarily helpful to our clinical practices and research efforts. The institution has recognized his success in clinical informatics by placing him in leadership roles such as medical director for our Center for the Science of Healthcare Delivery’s Clinical Informatics Program, the Unified Data Platform Oversight Group, and the Center for Digital Health Data Analytics program, as well as appointing him Dean of Research Data and Digital Solutions. - Transfusion Medicine.
DJ has been a leader in transfusion medicine within Mayo Clinic and in our specialty. He first obtained an NIH R01 grant related to transfusion practices. He subsequently gained institutional and national visibility in transfusion medicine. He has served as chair of Mayo Clinic’s Transfusion Medicine Committee and as chair of the ASA’s Committee on Transfusion Medicine. He’s been very involved in multiple committees of the American Association of Blood Banks. - Leadership. As a former elite college football player, DJ believes strongly in teamwork, especially on specific projects and across Mayo Clinic’s three mission shields of clinical practice, research, and education. He has become an oral examiner for the ABA and the chair of both the Research Committee and the Education Committee of the Society of Critical Care Anesthesiologists. He is a frequent visiting professor to high profile academic medical centers and is in high demand to speak at annual meetings of the ASA and other specialty societies. In August of this year, DJ became our Rochester department chair. In this role, he oversees a department of approximately 1,400 staff members. We know that he will enjoy the role, and that the Rochester department will benefit from his extensive leadership experience.
DJ and his wife, Molly, have 3 sons ranging from 15 to 20 years of age. Hockey predominates as a family activity, with many weekends and most weekdays filled with events and practices in ice arenas. In whatever spare time they have, DJ and Molly love to travel, preferably to warm places that have sand, sun, and water.

Carlos B. Mantilla, M.D., Ph.D. was born in Medellin, Colombia but moved to the U.S. shortly after with his family. They were mostly in Nashville, TN where his late father pursued training in Pharmacology. His family instilled in him the importance of education from an early age. Upon returning to Colombia, they lived in Bogotá, where Carlos attended a high school founded by Benedictine monks from North Dakota. He distinguished himself in school academically and had the honor of being part of the mathematics Olympiad team representing Colombia in the International Olympiad in Warsaw, Poland during his senior year. He then attended medical school at the Universidad del Rosario, where he was awarded among several distinctions that of Collegian, a member of a council that in the tradition of the oldest Spanish universities elects the institutional governing body.
Upon completing medical school, Carlos went on to fulfill his social service year working as a general practitioner in the Amazon jungle. It was there that he met his wife, Pilar, who was working with the Office of the First Lady of Colombia on a joint project with UNICEF to serve women and children in the Amazon basin. After fulfilling his social service year, Carlos moved to Rochester and was followed by Pilar a year later to further their education.
Carlos became a resident in our anesthesiology program and completed his training in 1998. This was followed by a fellowship in pain medicine in 2001. During his fellowship he pursued research under the mentorship of our own Dr. Gary Sieck, earning a Ph.D. in Biomedical Sciences – Molecular Neuroscience in 2003. He studies the control of breathing, with the long-term goal to develop rational and effective therapies for the treatment of diseases that impair the ability to breathe independently. His work has explored the mechanisms behind aging-related susceptibility to respiratory infections and other complications, the restoration of mechanical ventilator independence following cervical spinal cord injury, and recently, the use of diaphragm muscle shear wave elastography to identify patients at risk for opioid-induced respiratory depression.
Carlos is a Professor of Anesthesiology and Physiology and a named Clinician-Investigator. He served as chair for our department from 2016 to 2024 and has maintained a long-standing record of extramural funding for his research work, including during his time as chair. He also has contributed to the institution in other roles, including service as director of the research programs for the Center of Clinical and Translational Sciences and member of the Research Committee. Carlos also has served the NIH as member of the Aging Systems and Geriatrics study section and as chair of the Respiratory Integrative Biology and Translational Sciences study section. He has a long-standing commitment to education and has served as Associate Program director for our residency and as director for the Ph.D. program in Biomedical Engineering and Physiology. He is a member of the Committee for Academic Anesthesiology for the American Society of Anesthesiologists and an oral examiner for the American Board of Anesthesiology. He and his wife have been founding supporters of the Alliance of Chicanos, Hispanics and Latinoamericans (ACHLA) in Rochester, including their math tutoring program “Juntos”.
Pilar and Carlos also have supported numerous patients being treated at Mayo for reconstructive and other needs following landmine injuries as part of a joint Mayo program with the United for Colombia Foundation. They enjoy traveling and spending time with family, friends and their dog, Vida.
Alan D. Sessler, M.D. was born on April 4, 1932, in Boston. After completing Boston Latin High School in 1949 and Dartmouth College in 1953, he entered Tufts Medical School in Boston and earned his M.D. in 1957. He entered an anesthesiology residency at Dartmouth’s Mart Hitchcock Memorial Hospital in Hanover, New Hampshire that year but his training was interrupted by 2 years of service from 1959 through 1961 in the U.S. Navy. He served as a medical officer at the U.S. Naval Hospital, Great Lakes, Illinois and aboard a heavy cruiser, the U.S.S. Des Moines in the Mediterranean Sea. Upon completion of his service in 1961, he moved to Rochester as a fellow in anesthesiology for a final year of training. He was appointed as a consultant in 1962.
Alan left a lasting imprint on our Rochester department, medicine, and our specialty.
Education. Alan dramatically improved our residency training, implemented subspecialty fellowships, and expected all graduates to obtain ABA certification. This expectation led to Mayo Clinic having the highest success rate for board certification of graduates of any program in the U.S. for decades. He was a lifelong advocate for education, pushing for new programs, higher expectations of trainees, and support of certification. His love of education led to him serving on the ACGME’s Residency Review Committee for Anesthesiology and the ABA’s Board of Directors (president in 1988). He also became dean of the Mayo Clinic School of Graduate Medical Education, starting an anesthesia tradition within the school that led to Drs. Mark Warner and Steve Rose following as deans of the school. He was a trustee and president of his alma mater’s Dartmouth Hitchcock Clinic, Hospital, and Medical Center and, in that role, provided guidance and oversight on the college’s School of Medicine and other healthcare programs. In his final years of retirement, Alan served as a tireless advocate for our Rochester school system and was a leader of our Rochester Public Library, boosting efforts to improve literacy in the community.
Practice. Within Mayo Clinic, Alan teamed with Dr. Paul Didier to develop the institution’s critical care services and fellowships. He strongly believed that anesthesiology should evolve from intraoperative to perioperative care in its many facets. He was encouraged by Dr. Albert Faulconer, his initial department chair and mentor, to push for expanded opportunities for anesthesiologists . . . and he adopted this approach vigorously for the remainder of his career. During his leadership as our Rochester department chair from 1977 through 1989, Alan steadily increased the proportion of our department’s efforts to expanded practices in pain medicine, critical care medicine, preoperative evaluation, and transfusion medicine. He envisioned a broader role for respiratory care and quietly influenced institutional leaders to open new practice opportunities (e.g., the pulmonary function laboratory, and the emergency and postoperative recovery room practices). He was an influential leader in the ASA and ABA in starting subspecialty certification and increasing the roles of anesthesiologists in pain medicine, critical care, transfusion medicine, pediatric anesthesia, and hyperbaric medicine.
Research. While Alan was not an independent researcher, he supported expansion of anesthesia research within the institution and extramurally. He used his role as ASA Vice-President of Scientific Affairs to encourage the NIH to increase anesthesia-related funding. He played a major role in starting the Foundation for Anesthesia Education and Research (FAER), an organization that has provided today more than $70 million of funding to support new investigators in the specialty. He served as president as well as executive director of FAER for more than a decade and started many new programs to increase the number of medical students and trainees with interest in pursuing clinical and basic research in the specialty. Alan also was a founding director of the Anesthesia Patient Safety Foundation (APSF), an organization that, like FAER, have provided millions of dollars of support for trainees and junior anesthesiologists as they start their research careers in patient safety-related fields.
Administration. In addition to serving as the department’s first chair of its Section on Critical Care, Alan was our department chair from 1977 through 1989. He was a member of the Mayo Clinic Board of Governors from 1988 through 1992 and dean of the Mayo Clinic School of Graduate Medicine Education from 1989 through his retirement in 1995. He served as a long-time director of the ASA and as its Vice-President of Scientific Affairs. He was a director of the ABA from 1977 through 1989 and president during 1988. He was executive director of FAER from 1995 though 2008. He received the ASA’s Distinguished Service Award and was an honorary fellow of the Faculty of Anaesthetists of Royal College of Surgeons in Ireland and the Royal College of Anaesthetists of the U.K.
Simply put, Alan was one of the country’s most influential anesthesiologists for more than 5 decades (1960-2010). Our own Dr. Doug Bacon summarized his contributions in his elegant memorial tribute following Alan’s death on March 18, 2020. Alan was even more than an incredible leader in our department and specialty; he was a mentor and sponsor for many of us. As I note in a personal tribute I wrote about Alan, he was a parental figure, providing us with expectations for success and continual encouragement to excel and make those around us do the same. Alan and his wife, Dr. Martha (Smith) Sessler, were proud parents of three children. Martha completed her training in anesthesiology in Rochester in the Class of 1962 with Alan. She currently lives in Charter House in Rochester.

Mark A. Warner, M.D. was born in Greenville, Ohio on October 7, 1953 and was raised on a Jersey dairy farm with his family and grandparents. He graduated from Miami University in Oxford, Ohio in 1976 and entered the Medical College of Ohio (now the University of Toledo School of Medicine). At 7:57 AM on July 6, 1976, he met his future wife, Mary Ellen, as she stood on the medical school steps and unknowingly captured his attention on their way into their first class. After 6 months of relentless pursuit, Mary Ellen finally agreed to a first date.
During their junior year of medical school, they obtained ASA Preceptorship awards with the assistance of their mentor, Dr. J. Tom Martin, a former Mayo Clinic anesthesiologist and Rochester Methodist Division leader. Drs. Alan Sessler, Duane Rorie, Ron Faust, and Jim Prentice were their advocates during their two months in Rochester in Spring 1978. Mark and Mary Ellen married in their senior year, graduated in 1979, and moved to Rochester as new residents in 1979. The first two people they met in the department were Ann (Tvedt) Brumm and Donna (née Huntley, formerly Goetsch) Baxter, two of the secretaries in our St. Marys 4 Joseph department office. Dr. Faust was their program director and Dr. Sessler was the chair. Their first-year classmates included Drs. Bob Chantigian, Steve Rettke, Mark Martinson, and John Billings.
Mark completed his residency training in December 1982 and joined the staff. Two of the first new residents assigned to him in July 1983 were Drs. Brad Narr and Jim Eisenach. Of his clinical activities, he is exceptionally proud that the old General Section (now the Multispecialty Division at St. Marys Hospital) provided anesthesia for 225 consecutive children with severe mandibular hypoplasia (e.g., Pierre Robin and Treacher Collins syndromes) without any lost airways or tracheostomies in a time before pediatric fiberoptic endoscopy was available. Colleagues who were extensively involved in the care of these children with him included Drs. Steve Kunkel, Scott LeBard, Lynn Christianson, and Doug Bell and nurse anesthetists such as Mary Marienau, Curt Buck, and John Carter. By the mid-1980s, Mark and colleagues recognized the need for a unique team to care for the institution’s smallest children and formed the pediatric call group. This call group expanded their scope of practice to the evolving pediatric transplant services and postoperative pain management. Recruitment over time of key pediatric anesthesiologists such as Drs. Randy Flick, Bob Friedhoff, Greg Shears, and Bob Lunn rapidly escalated the skill set and size of the pediatric anesthesia group and tied the department closely to the overall integrated pediatric practice at Mayo.
For much of his career, Mark assumed administrative roles within the department and the institution. He was sequentially the chair of the General Section within the department at St. Marys Hospital, the inaugural chair of the Pediatric Council for the institution, the vice-chair of the institution’s Clinical Practice Committee, and the first chair of what is now the institution’s Hospital Practice Committee. He became chair of the Rochester Department of Anesthesiology in 1999 and continued in that role through 2006. Working closely with Drs. Brad Narr, his vice-chair of the practice; Steve Rose, his vice-chair of education; and Mary Ellen who developed the new, innovative Gonda ambulatory practices with colleagues such as Steve Jorgensen, Marla Judd, and Steve Osborn, he was able to watch the department thrive. The department grew in size and academic stature internally and externally. At two different points during his term as department chair, department colleagues served as presidents of 6 of the 8 primary subspecialty societies and Dr. Ron Mackenzie served as ASA president in 2000. He is most proud of the outstanding care provided by his colleagues, the department’s national visibility, and the leadership that colleagues throughout the institution provide for the advancement of specialty.
In 2006, Mark stepped down from his department chair role and joined the Mayo Clinic Board of Governors. He remained a director of that Board as it evolved to the Rochester Board of Governors. He also served the institution as Dean, Mayo Clinic School of Graduate Medical Education (MCSGME; 2006-2012) and Executive Dean of Education (2012-2016). Throughout his time as an education leader, he worked side-by-side with colleague Dr. Steve Rose. Steve was his vice-dean of MCSGME and then later dean of that school. His mentor, sponsor, and surrogate father figure, Dr. Alan Sessler, also provided daily advice.
Mark was involved in the specialty within Minnesota and nationally. He served as a director of the American Board of Anesthesiology from 1998 through 2010 and was president of the ABA in 2009. He also was president of the ASA in 2011, the Academy of Anesthesiology in 2015, and the Anesthesia Patient Safety Foundation from 2016 through 2021. He has received Distinguished Service Awards from the ASA and the Minnesota Society of Anesthesiologists, as well as a Distinguished Educator Award from Mayo Clinic and a Distinguished Alumnus Award from the Medical College of Ohio. He is an honorary fellow of the College of Anaesthesiologists of Ireland. His ASA Distinguished Service Award was announced by former Mayo Clinic Arizona department chair Dr. Dan Cole.
Mark and Mary Ellen have four sons and 10 grandchildren. Two of their sons, along with their wives, are anesthesiologists in our Rochester department. Mark’s first cousin, Dr. David Warner, is one of the recruits he helped to attract to the department. Both Mark and Mary Ellen continue to work clinically. They enjoy traveling, having stayed overnight in more than 100 countries, and visiting their grandchildren. They maintain a farm and spend their spare time caring for their land and contributing to the community.
Finally, a Farewell.
Best wishes to you all. On behalf of the Centennial Project Team, thank you for all you do to support the education of our students and trainees, the safety of our patients, and the success of our department, the specialty, and the institution.





















































































































































